Vertebral compression fractures (VCFs) significantly correlate with increased mortality rates, with studies showing 15-30% higher death risks compared to fracture-free patients. However, this relationship stems primarily from underlying health conditions rather than the fracture itself. This analysis explores how Life Expectancy After Compression Fracture: Understanding the Prognosis and Influencing Factors
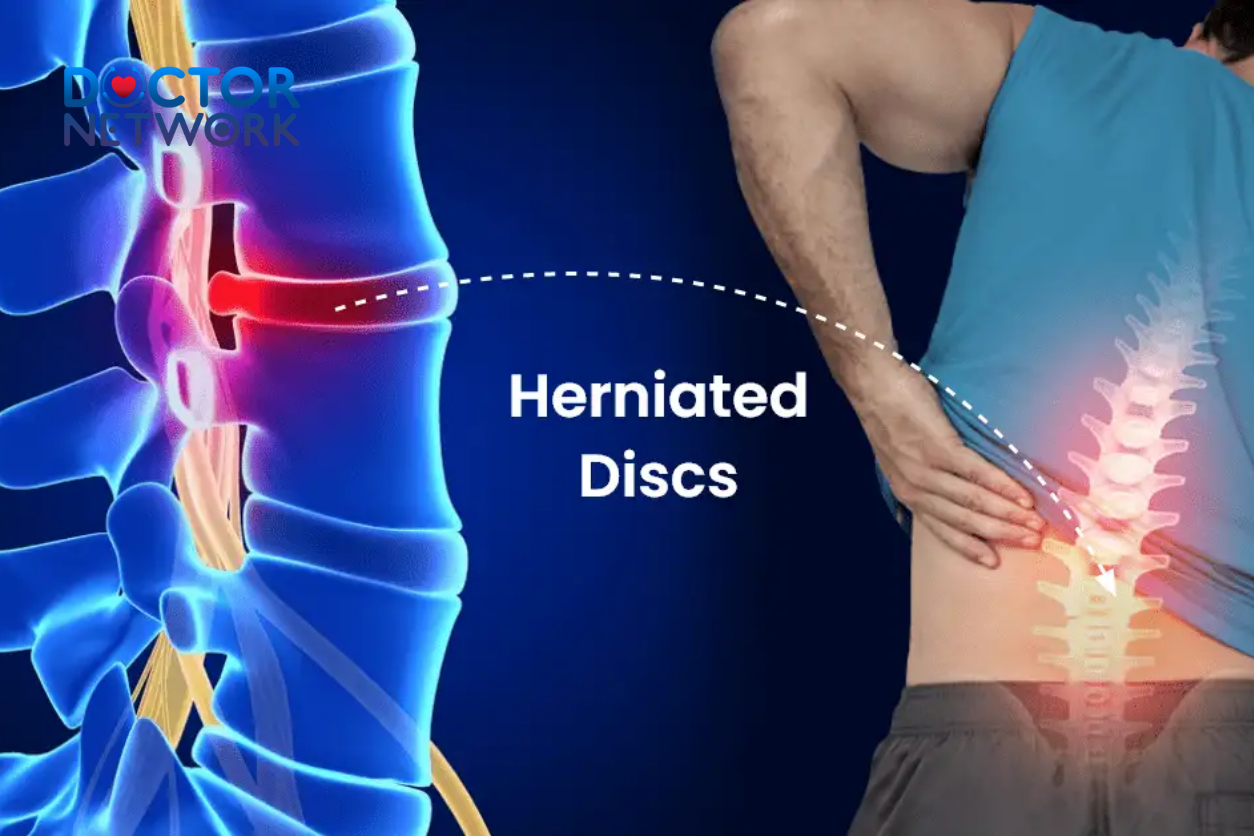
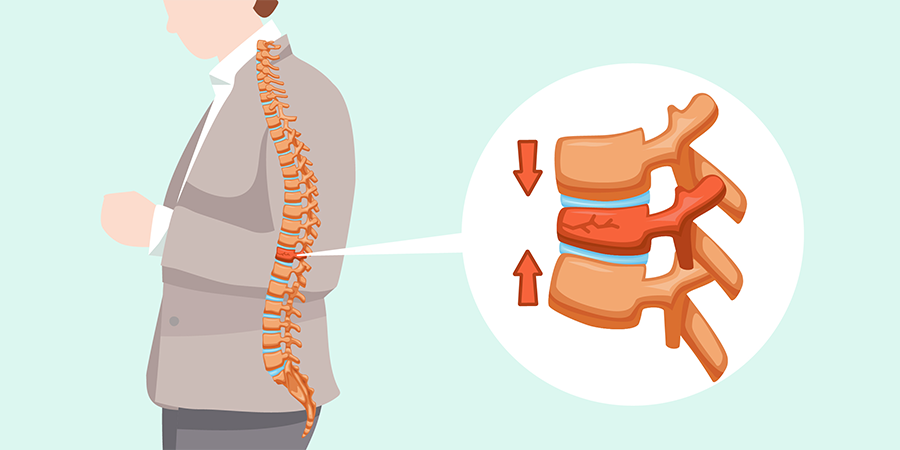
Understanding Vertebral Compression Fractures
A vertebral compression fracture occurs when spinal vertebrae collapse, creating wedge-shaped deformities most commonly in the thoracic and lumbar spine. Primary causes include:
- Osteoporosis (85% of cases in patients >65 years)
- Malignancy (metastatic disease from breast, lung, prostate cancers)
- Trauma (high-impact injuries in younger patients)
- Metabolic bone disease (steroid use, hyperparathyroidism)
Diagnosis relies on MRI and CT imaging to assess fracture patterns and spinal stability, with some patients experiencing severe acute pain while others remain asymptomatic.
 Spinal Compression Fracture is a common condition recently
Spinal Compression Fracture is a common condition recently
Direct Impact on Life Expectancy
Compression fractures rarely cause immediate mortality but serve as sentinel events indicating advanced osteoporosis, frailty, or underlying malignancy. Research by Kado et al. demonstrated 23% higher mortality risk over 15 years in women with vertebral fractures.
| Patient Group | Mortality Increase | Primary Driver |
|---|---|---|
| Women >65 years | 15-30% | Osteoporosis complications |
| Cancer patients | 40-60% | Disease progression |
| Trauma victims | 5-15% | Associated injuries |
Key Prognostic Factors
Age represents the strongest predictor of outcomes, with patients over 80 experiencing substantially higher mortality rates. Critical factors include:
- Advanced age (>75 years): 2-3x increased mortality risk
- Multiple fractures: Exponentially worse prognosis
- Severe vertebral collapse (>50% height loss)
- Comorbidities: COPD, heart disease, diabetes
- Poor nutritional status: Protein-energy malnutrition
The cumulative effect of multiple risk factors creates multiplicative rather than additive mortality risks.
Osteoporosis and Mortality Connection
Osteoporotic patients with vertebral fractures show 20-40% higher mortality than those with osteoporosis alone. The skeletal fragility evidenced by compression fractures indicates advanced bone disease and predicts future hip fractures, which carry even higher mortality risks (2.3-fold increased risk per additional vertebral fracture).
Complications Affecting Longevity
Post-fracture complications create the primary pathway linking compression fractures to increased mortality:
Major Complications:
- Chronic pain (60-80% of patients) → activity restriction, depression
- Immobility → 20-30% muscle strength loss, cardiovascular deconditioning
- Respiratory compromise → up to 20% lung capacity reduction from kyphosis
- Fall risk → 40-60% increased probability, leading to secondary fractures
- Depression → affects 40-50% of patients, correlating with poor outcomes
Treatment and Management Impact
Early diagnosis and treatment primarily improve quality of life rather than directly reducing mortality. Treatment options include:
| Treatment | Success Rate | Key Benefits |
|---|---|---|
| Conservative therapy | 60-70% | Bracing, medications, PT |
| Vertebroplasty | 80-85% | Rapid pain relief |
| Kyphoplasty | 85-90% | Pain relief + height restoration |
Conservative management includes pain medications, bracing, physical therapy, and osteoporosis treatment. Minimally invasive procedures like vertebroplasty and kyphoplasty provide immediate structural support and pain relief in selected patients.
 There is an impact on life expectancy after compression fracture
There is an impact on life expectancy after compression fractureNon-Medical Factors
Beyond clinical interventions, broader factors significantly influence outcomes:
- Social support: 25-30% better outcomes with strong networks
- Nutritional status: Malnutrition affects 20-30% of patients
- Economic factors: Annual costs $15,000-$25,000 per patient
- Housing environment: Home modifications reduce fall risk
Socioeconomic disparities create barriers to optimal care, with lower-income patients experiencing delayed diagnosis and higher complication rates.
Prevention Strategies
Prevention offers the most effective approach to reducing mortality risks:
Evidence-Based Prevention:
- DEXA screening for patients over 65
- Bisphosphonate therapy for osteoporosis
- Fall prevention programs
- Weight-bearing exercise
- Calcium and vitamin D supplementation
Comprehensive prevention programs can reduce fracture incidence by 40-60% in high-risk patients.
Future Directions
Emerging therapies include anabolic bone agents, advanced biomaterials for vertebral augmentation, and AI applications in fracture risk prediction. Research faces challenges including long follow-up periods and confounding variables affecting mortality studies.
Conclusion
Vertebral compression fractures associate with increased mortality primarily as indicators of underlying frailty and systemic disease rather than direct causes of death. Individual prognosis depends on age, overall health, fracture severity, and complication development.
Key Takeaways:
- Prompt medical evaluation enables early intervention
- Aggressive osteoporosis management reduces future fracture risk
- Comprehensive pain control improves quality of life
- Prevention strategies offer the greatest mortality reduction potential
While compression fractures signal increased health risks, appropriate medical management combined with comprehensive support can help maintain quality of life and potentially mitigate mortality risks. Success requires recognizing these fractures as opportunities for comprehensive health assessment rather than isolated orthopedic events.
Related 5 most frequently asked questions
1. What is the average life expectancy after suffering a compression fracture?
Life expectancy after a compression fracture, especially in older adults, varies widely depending on factors such as age, gender, overall health, and treatment method. Studies show that patients over 65 years old who undergo surgery have about a 65.6% survival rate at 4 years, compared to 51.9% for those treated conservatively. Procedures like kyphoplasty have been associated with a significant increase in adjusted life expectancy. However, the fracture itself rarely directly reduces life expectancy; rather, complications and underlying health conditions play a major role.
2. Does a compression fracture directly affect life expectancy?
Compression fractures rarely cause death directly. However, they can lead to serious complications such as chronic pain, reduced mobility, nerve damage, and increased risk of secondary conditions like pneumonia or deep vein thrombosis, especially in the elderly. These complications can indirectly reduce life expectancy. Research indicates that mortality rates are higher in patients with compression fractures compared to matched controls, particularly in men and those with pre-existing illnesses.
3. What factors influence life expectancy after compression fracture?
Factors that increase the risk of mortality after a compression fracture include:
Advanced age and male gender
History of cancer or other chronic diseases
Fractures caused by severe osteoporosis rather than trauma
Presence of complications or comorbidities during treatment and hospitalization
Type of treatment received: surgical interventions like kyphoplasty may improve survival compared to conservative care
4. How do treatment methods affect life expectancy after a compression fracture?
Treatment can be conservative (rest, pain medication, physical therapy) or surgical (vertebroplasty, kyphoplasty). Studies suggest that patients undergoing surgery tend to have better adjusted survival rates than those treated conservatively, with kyphoplasty showing the most benefit. However, some research shows no significant difference in long-term survival between surgical and non-surgical treatments, highlighting the importance of individualized care.
5. How can quality of life & life expectancy be improved after a compression fracture?
To improve life expectancy and quality of life after a compression fracture, it is important to:
Effectively manage pain to maintain mobility and participate in rehabilitation
Treat and prevent osteoporosis with calcium, vitamin D, and medications
Adopt a healthy lifestyle: regular appropriate exercise, quitting smoking, limiting alcohol
Monitor and treat complications and comorbid conditions promptly
Have regular follow-ups to assess recovery and prevent new fractures
Key scientific evidence
Kado DM et al. (1999)
Study Title: “Vertebral Fractures and Subsequent Mortality: Results From the Study of Osteoporotic Fractures.”
Source: Archives of Internal Medicine, 1999;159(11):1215-1220.
Link to Abstract (PubMed): https://pubmed.ncbi.nlm.nih.gov/10371229/
Center JR et al. (1999)
Study Title: “Mortality after all types of osteoporotic fracture in men and women: an observational study.”
Source: The Lancet, 1999;353(9156):878-882.
Link to Abstract (PubMed): https://pubmed.ncbi.nlm.nih.gov/10093980/
(Alternative via The Lancet, may require login/purchase for full text): https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(98)07211-X/fulltext
Bliuc D et al. (2009)
Study Title: “Mortality Risk Associated With Low-Trauma Osteoporotic Fracture and Subsequent Fracture in Men and Women.”
Source: JAMA (Journal of the American Medical Association), 2009;301(5):513-521.
Link to Abstract (PubMed): https://pubmed.ncbi.nlm.nih.gov/19190316/
(Alternative via JAMA Network, may require login/purchase for full text): https://jamanetwork.com/journals/jama/fullarticle/183370
Schlaich C et al. (1998)
Study Title: “Reduced pulmonary function in patients with spinal osteoporotic fractures.”
Source: Osteoporosis International, 1998;8(3):261-267.
Link to Abstract (PubMed): https://pubmed.ncbi.nlm.nih.gov/9797900/
(Alternative via SpringerLink, may require login/purchase for full text): https://link.springer.com/article/10.1007/s001980050060
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.