Tooth pain occurring months after dental filling placement creates significant concern for patients who believed their dental problems were permanently resolved. This delayed discomfort affects approximately 5-15% of patients who undergo restorative procedures, challenging the assumption that successful initial healing guarantees long-term comfort.
Understanding why does my tooth filling hurt after months requires examining multiple factors including nerve irritation, secondary decay development, bite irregularities, and material-related complications. This comprehensive guide explores the underlying causes of delayed dental pain, diagnostic approaches, and effective treatment solutions available to resolve persistent discomfort.
Understanding the Timeline: Why Pain Can Appear Weeks or Months Later
Delayed onset dental pain differs significantly from immediate post-procedural sensitivity, which typically resolves within days following restoration placement. This temporal distinction serves as a crucial diagnostic indicator, helping dental professionals differentiate between normal healing responses and pathological conditions requiring intervention.
Certain dental complications manifest gradually rather than immediately following restorative procedures. The biological processes underlying delayed pain include progressive pulpal inflammation, bacterial colonization around restoration margins, and occlusal trauma accumulation over time. These mechanisms explain why patients experience symptom onset weeks or months after initially successful treatments.
What Does Your Pain Feel Like? A Symptom-Based Guide
Dental pain characteristics provide essential diagnostic information that helps identify underlying causes and guide appropriate treatment decisions. Understanding specific pain patterns enables effective communication with dental providers and targeted therapeutic interventions.
Sharp, stabbing pain during biting or chewing typically indicates occlusal trauma, restoration height discrepancies, or tooth fractures. Dull, throbbing aches often suggest inflammatory processes within the dental pulp or surrounding tissues. Temperature sensitivity, particularly to cold stimuli, frequently indicates compromised pulp vitality or exposed dentinal tubules around restoration margins.

Common Pain Patterns and Their Implications:
| Pain Type | Characteristics | Likely Causes |
|---|---|---|
| Sharp, intermittent | Occurs with biting/chewing | High restoration, tooth fracture |
| Dull, constant | Persistent aching, worse at night | Pulpal inflammation, infection |
| Temperature sensitive | Cold/hot triggers discomfort | Nerve irritation, exposed dentin |
Common Causes of Tooth Filling Pain After Months
Sensitivity to Bite Pressure and Occlusion Issues
Occlusal interference represents one of the most frequent causes of delayed filling-related pain, occurring when restoration height exceeds optimal parameters. Even minimal elevation differences can create excessive force concentration during mastication, leading to progressive periodontal ligament irritation and chronic discomfort.
The biomechanical stress from high restorations affects multiple oral structures including the restored tooth, opposing dentition, and temporomandibular joint complex. Continuous trauma from premature contacts results in tooth mobility, sensitivity, and eventual pulpal pathology if left untreated.
Deep Filling Near the Dental Nerve and Pulpitis
Deep cavities requiring extensive tooth structure removal often necessitate restorations placed in close proximity to the dental pulp. Even when initial post-operative symptoms remain minimal, the pulp-dentin complex may develop delayed inflammatory responses due to bacterial toxins, thermal shock, or desiccation during the restorative procedure.
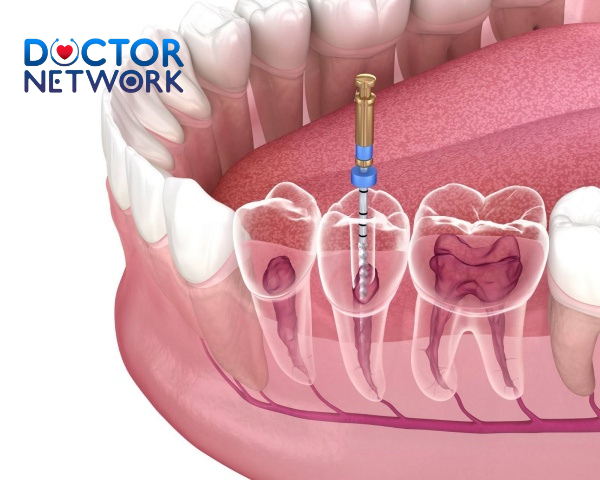
Progressive pulpitis develops through several stages, beginning with reversible inflammation that may resolve spontaneously. However, continued irritation can progress to irreversible pulpitis, characterized by severe spontaneous pain, prolonged thermal sensitivity, and eventual pulpal necrosis requiring endodontic intervention.
Secondary Decay Development
Secondary caries development around existing restorations accounts for a significant percentage of delayed dental pain cases. Marginal breakdown, inadequate oral hygiene, and bacterial microleakage create conditions favorable for renewed decay processes beneath or adjacent to restoration margins.
The progression of secondary decay differs from primary caries, often advancing more rapidly due to altered tooth structure and potential bacterial reservoirs around restoration interfaces. Initial stages may remain asymptomatic until decay reaches deeper tooth layers, stimulating pulpal inflammation and associated pain responses.
Cracked Tooth Syndrome
Cracked tooth syndrome represents a challenging diagnostic entity characterized by incomplete tooth fractures that may develop months after restoration placement. Large restorations, particularly those involving multiple tooth surfaces, can weaken remaining tooth structure and predispose to crack formation under normal occlusal forces.
The clinical presentation typically includes sharp, intermittent pain during chewing, especially when releasing bite pressure. Temperature sensitivity and difficulty localizing discomfort are common features that complicate accurate diagnosis and treatment planning.
Filling Material Issues
Contemporary restorative materials can develop complications over time that contribute to delayed pain symptoms. Composite resin restorations may experience polymerization shrinkage, leading to marginal gaps that allow bacterial penetration and secondary decay development. Amalgam restorations can undergo corrosion and expansion processes that create internal stress within tooth structure.
Comparison of Common Filling Materials:
| Material | Advantages | Potential Issues | Longevity |
|---|---|---|---|
| Composite Resin | Aesthetic, conservative | Shrinkage, wear | 5-10 years |
| Amalgam | Durable, cost-effective | Corrosion, expansion | 10-15 years |
| Ceramic | Natural appearance | Brittleness | 10-15 years |
Infection or Abscess Formation
Dental infections represent serious complications that can develop months after restoration placement, particularly when deep decay or pulpal exposure occurred during initial treatment. Bacterial colonization of necrotic pulpal tissue leads to periapical pathology, including acute apical periodontitis and abscess formation.
Clinical signs of dental infection include spontaneous throbbing pain, percussion sensitivity, soft tissue swelling, and possible systemic symptoms such as fever or malaise. Treatment typically requires endodontic therapy or extraction, often combined with antibiotic therapy for cases involving cellulitis or systemic spread.
When to Seek Professional Help
Persistent dental pain following restoration placement warrants professional evaluation to prevent complications and ensure optimal treatment outcomes. Certain symptoms indicate urgent conditions requiring immediate dental attention.
Signs requiring immediate professional attention include:
- Severe, constant throbbing pain unresponsive to analgesics
- Facial swelling extending beyond the oral cavity
- Difficulty swallowing or opening the mouth
- Fever or systemic symptoms accompanying dental pain
- Visible pus drainage or abscess formation
Symptoms warranting scheduled consultation include:
- Intermittent pain lasting more than 2-3 weeks
- Temperature sensitivity interfering with normal function
- Discomfort during chewing or biting
- Changes in restoration appearance or margins
Visiting the Dentist: What to Expect
Professional evaluation of delayed filling-related pain follows systematic diagnostic protocols designed to identify underlying causes and develop appropriate treatment plans. The initial consultation begins with comprehensive medical and dental history review, focusing on symptom characteristics, timing, and aggravating factors.
Clinical examination involves visual inspection of the restoration and surrounding tissues, percussion testing to evaluate periapical sensitivity, and palpation of adjacent structures. Dentists assess restoration margins, tissue health, occlusal relationships, and overall oral condition during this phase.
Diagnostic procedures may include:
- Radiographic imaging to evaluate internal structures
- Pulp vitality testing to assess nerve health
- Bite analysis to check occlusal contacts
- Periodontal probing to evaluate gum health
Treatment Options Based on Diagnosis
Therapeutic interventions for delayed filling-related pain depend on accurate diagnosis and may range from simple adjustments to complex surgical procedures. Conservative approaches include occlusal adjustment for bite-related discomfort, desensitizing agents for mild sensitivity, and restoration polishing or marginal refinement.
Intermediate interventions encompass restoration replacement for material failure or secondary decay, protective restorations for cracked teeth, and periodontal therapy for gum-related complications. Advanced treatment modalities include endodontic therapy for irreversible pulpitis, surgical endodontics for persistent periapical pathology, and crown placement for extensively restored teeth.
Treatment success rates vary depending on the underlying condition and intervention timing. Early diagnosis and appropriate treatment typically result in favorable outcomes, while delayed care may compromise treatment effectiveness and require more extensive procedures.
Preventing Future Pain and Maintaining Oral Health
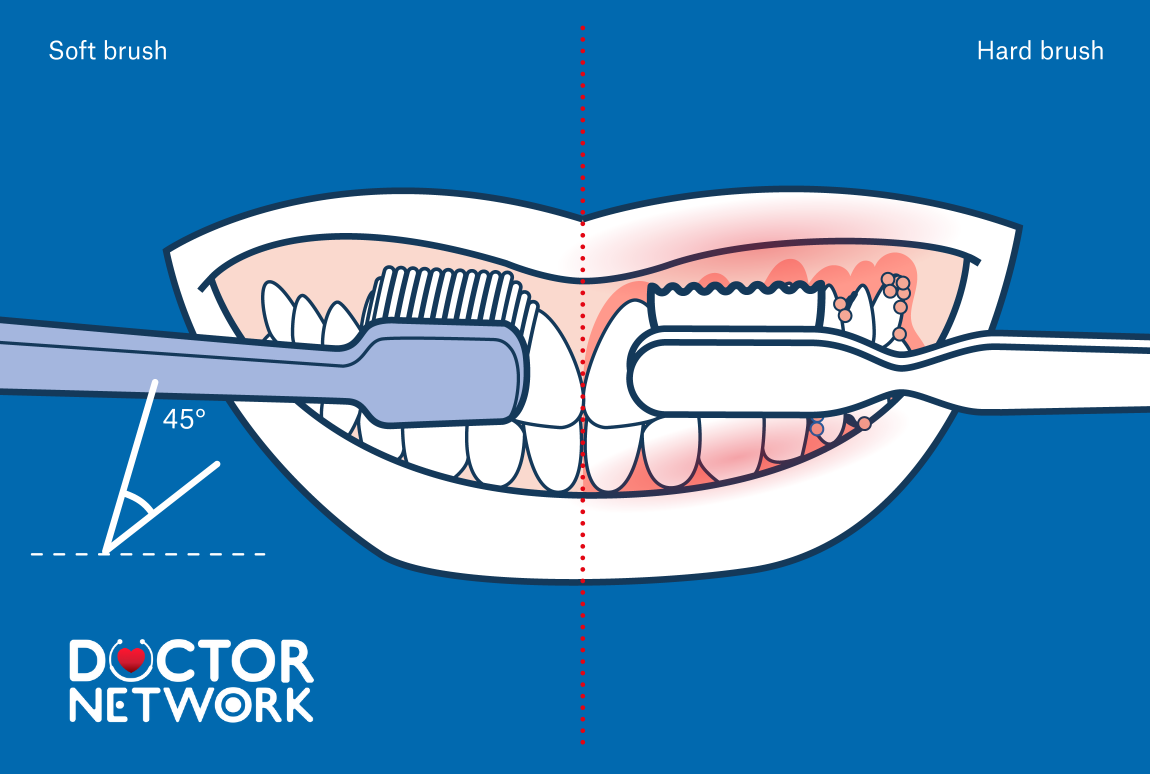
Preventive strategies play crucial roles in minimizing recurrent dental problems and maintaining long-term oral health following restorative treatment. Essential oral hygiene practices include twice-daily brushing with fluoride toothpaste, daily interdental cleaning, and regular professional cleanings and examinations.
Dietary modifications involve limiting sugar and acidic food consumption, choosing tooth-friendly snacks, and avoiding sticky or hard foods that stress restorations. Behavioral modifications include using protective nightguards for bruxism management and avoiding harmful habits like ice chewing or using teeth as tools.
Regular dental surveillance allows early detection of developing problems before they become symptomatic. Risk factor modification reduces the likelihood of restoration failure and associated complications, with high-risk patients benefiting from additional fluoride supplementation or more frequent professional interventions.
Conclusion

Delayed tooth filling pain represents a complex clinical challenge with multiple potential causes requiring professional evaluation and targeted treatment. Understanding various etiologies, from occlusal trauma and secondary decay to pulpal pathology, helps patients recognize when professional care becomes necessary.
The importance of timely dental consultation cannot be overstated, as early intervention typically results in more conservative treatment approaches and better long-term outcomes. Modern dentistry offers numerous effective treatment modalities for addressing delayed filling-related pain, and with proper diagnosis and appropriate treatment, most patients can expect successful symptom resolution and restoration of normal oral function.
5 most frequently asked questions about topic: Why Does My Tooth Filling Hurt After Months
1. Why does my tooth filling hurt months after it was done?
There are several reasons why a tooth filling might cause pain months after placement:
New decay or decay around the filling: Bacteria can infiltrate and cause new cavities or recurrent decay around the filling.
Cracked or broken filling: Cracks or chips in the filling can irritate the tooth and cause pain.
Leaking or loose filling: If the filling is not sealed properly, bacteria and saliva can enter, leading to inflammation or decay.
Pulp inflammation or infection: If the filling is close to the tooth’s nerve (pulp), it can cause irritation or infection, resulting in prolonged pain.
Bite issues: A filling that is too high or uneven can cause abnormal bite forces, leading to pain when chewing.
Allergic reaction to filling material: Some people may react to metals or composite materials used in fillings, causing discomfort.
2. Is it normal to have pain after a filling?
Mild sensitivity or discomfort for a few days to weeks after a filling is normal as the tooth adjusts.
However, persistent or severe pain months later is not normal and should be evaluated by a dentist to identify and treat the cause.
3. How can I tell if my filling is damaged or needs replacement?
Signs include pain when biting or chewing, feeling that the filling is loose, visible cracks, or gaps between the filling and tooth.
Regular dental check-ups help detect these issues early for timely repair or replacement.
4. What can I do to reduce pain from a filling?
Use toothpaste designed for sensitive teeth to help reduce discomfort.
Avoid very hot, cold, or sweet foods that can trigger sensitivity.
Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage pain.
If the pain is due to bite problems, a dentist can adjust the filling to balance your bite.
5. When should I see a dentist if my filling hurts?
If the pain lasts more than a few weeks, worsens, or is accompanied by swelling, redness, or pus, you should see a dentist promptly.
Severe pain with fever, facial swelling, or signs of infection requires immediate dental care.
References
Recurrent Decay (Secondary Caries):
Explanation: New decay forms under or around the existing filling.
Source: Mjör, I. A. (1997). “The reasons for replacement and the age of failed restorations in general dental practice.” Acta Odontologica Scandinavica.
Source (on microleakage facilitating decay): Kidd, E. A. M. (2004). “Microleakage: a review.” Journal of Dentistry.
Pulp Inflammation (Pulpitis) or Necrosis (Nerve Death):
Explanation: The tooth’s nerve (pulp) becomes irreversibly inflamed or dies, often due to the original decay being deep or trauma from the procedure, with symptoms developing over time.
Source: Bergenholtz, G. (2000). “Pathogenic mechanisms in pulpal disease.” Journal of Endodontics.
Reference (Textbook concept): “Cohen’s Pathways of the Pulp” (various editions) details the progression of pulpal disease.
Cracked Tooth Syndrome:
Explanation: A crack in the tooth (either pre-existing or new) under or near the filling can cause pain, especially on biting.
Source: American Association of Endodontists (AAE). “Cracked Teeth.” (Position statements and patient information available).
Link (AAE general page on cracked teeth): https://www.aae.org/patients/dental-symptoms/cracked-teeth/
Link (Example of an older AAE Position Statement PDF): https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/07/crackedteethstatement.pdf (Note: AAE updates these, but this 2008 one is often cited).
Source (Classic paper): Cameron, C. E. (1976). “Cracked-tooth syndrome.” The Journal of the American Dental Association.
Bite (Occlusal) Problems:
Explanation: The filling might be slightly too high, causing trauma to the tooth when you bite or chew. This repeated stress can lead to pain over time.
Source (Concept of occlusal trauma): While specific studies on delayed pain from high fillings are part of general dental knowledge, the impact of occlusal forces is well-documented. For context on occlusal adjustment: Clark, G. T., & Takeuchi, H. (1992). “Occlusal adjustment therapy for the painful TMJ.” Dental Clinics of North America. (This discusses occlusal adjustment broadly, the principle applies).
Filling Wear, Fracture, or Debonding:
Explanation: The filling material itself may wear down, chip, crack, or lose its bond to the tooth, exposing sensitive areas or allowing leakage.
Source: Van Nieuwenhuysen, J. P., D’Hoore, W., Carvalho, J., & Qvist, V. (2003). “Long-term evaluation of extensive restorations in permanent teeth.” Journal of Dentistry.
Bruxism (Teeth Grinding/Clenching):
Explanation: Excessive forces from grinding or clenching can stress the filled tooth and the surrounding structures, leading to pain.
Source: Lobbezoo, F., et al. (2013). “Bruxism defined and graded: an international consensus.” Journal of Oral Rehabilitation.
Link: [https://pubmed.ncbi.nlm.nih.gov/231162 Bruxism](https://pubmed.ncbi.nlm.nih.gov/2311626 Bruxism defined and graded: an international consensus) (Correct link: https://onlinelibrary.wiley.com/doi/full/10.1111/joor.12011 or https://pubmed.ncbi.nlm.nih.gov/23116266/)
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.