Eye dilation—a critical diagnostic procedure that temporarily enlarges your pupils using specialized mydriatic drops—enables ophthalmologists and optometrists to thoroughly examine your retina, optic nerve, and blood vessels for early disease detection. While this routine examination proves essential for maintaining ocular health and preventing vision-threatening conditions like glaucoma, diabetic retinopathy, and macular degeneration, the temporary side effects require careful attention to specific safety protocols.
What Not To Do After Eye Dilation – This comprehensive guide covers the absolute contraindications following pupil dilation, explaining the physiological mechanisms behind each restriction, optimal recovery strategies, emergency warning signs, and expert recommendations for minimizing discomfort while maximizing safety during the recovery period.
Understanding Eye Dilation: The Medical Foundation

What Happens During Pupillary Dilation?
Mydriatic eye drops, typically containing phenylephrine 2.5% or tropicamide 0.5%-1%, temporarily paralyze the iris muscles that control pupil constriction. This pharmacological intervention allows your eye care professional to visualize structures normally hidden behind the naturally constricted pupil, including the macula, peripheral retina, and optic disc.
Common Temporary Side Effects
The dilation process produces predictable physiological responses that create temporary visual disturbances:
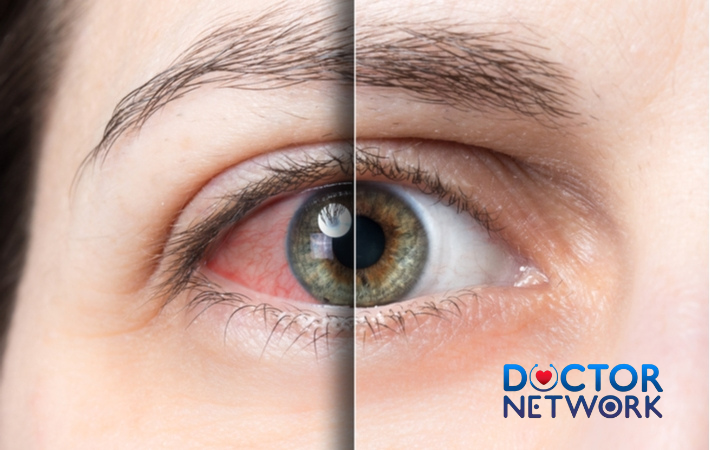
- Photophobia: Extreme sensitivity to bright illumination due to excessive light entering the dilated pupil
- Accommodation paralysis: Inability to focus on near objects, causing significant blur at reading distance
- Glare sensitivity: Pronounced difficulty with light sources, particularly reflective surfaces and direct illumination
- Mild ocular discomfort: Temporary stinging or dry sensation lasting 15-30 minutes post-instillation
Duration and Individual Variations
Standard Recovery Timeline:
- Typical duration: 2-6 hours for most patients
- Extended effects: Up to 24 hours in certain individuals
- Pediatric considerations: Children often experience prolonged effects requiring stronger concentrations
Factors Influencing Recovery Speed:
| Factor | Impact on Duration | Explanation |
|---|---|---|
| Iris Pigmentation | Dark eyes: Longer duration | Higher melanin content binds mydriatic agents more effectively |
| Age | Youth: Extended effects | Stronger concentrations needed; slower metabolism |
| Medication Type | Tropicamide vs. Phenylephrine | Different pharmacokinetic profiles affect elimination |
| Concurrent Medications | Variable interactions | Certain systemic drugs may prolong or reduce effects |
Critical Actions to Avoid After Pupillary Dilation
1. Driving or Operating Dangerous Equipment
Never attempt to drive or operate machinery immediately following eye dilation. The compromised visual acuity, severely impaired depth perception, and extreme photophobia create hazardous conditions that significantly increase accident risk.
Physiological Mechanisms:
- Accommodation paralysis prevents proper focusing on dashboard instruments and road signs
- Photophobia causes debilitating glare from oncoming headlights, sunlight, and reflective surfaces
- Reduced contrast sensitivity impairs hazard detection and reaction times
- Compromised peripheral vision due to light scatter within the dilated pupil
Extended Safety Considerations: Beyond vehicular operation, avoid using:
- Power tools (drills, saws, grinders)
- Sharp implements requiring precision
- Heavy machinery or industrial equipment
- Bicycles or motorcycles in traffic
Alternative Transportation Solutions:
- Arrange designated drivers before your appointment
- Utilize rideshare services or public transportation
- Schedule appointments when family members can provide transport
- Consider afternoon appointments to minimize work disruption
2. Direct Exposure to Bright Light Sources
Avoid direct sunlight, artificial lighting, and high-intensity illumination that can cause severe discomfort and potential retinal stress when protective pupillary constriction is pharmacologically blocked.
Why Light Sensitivity Occurs: Under normal circumstances, your iris automatically constricts in bright conditions, functioning as a natural aperture control system. Mydriatic agents disable this protective mechanism, allowing excessive luminous energy to reach light-sensitive retinal structures.
Specific Light Sources to Avoid:
- Direct sunlight and solar glare
- Vehicle headlights and streetlights
- Fluorescent and LED lighting systems
- Computer monitors and television screens
- Photography flashes and stage lighting
Protective Strategies:
| Protection Method | Effectiveness | Additional Benefits |
|---|---|---|
| UV-blocking sunglasses | Excellent | Prevents UV-related retinal damage |
| Wraparound frames | Superior | Blocks peripheral light infiltration |
| Indoor tinted lenses | Good | Reduces artificial lighting discomfort |
| Wide-brimmed hats | Moderate | Additional overhead protection |
3. Extended Digital Screen Usage
Minimize smartphone, computer, tablet, and television use during the acute dilation period to prevent digital eye strain and accelerated visual fatigue.
Digital Device Complications:
- Blue light emission intensifies photophobic symptoms in dilated pupils
- Near-focus demands prove impossible due to accommodation paralysis
- Screen glare creates multiplicative discomfort when combined with mydriatic effects
- Prolonged viewing delays natural recovery and increases ocular stress
Consequences of Excessive Screen Time:
- Severe asthenopia (eye strain)
- Cephalgia (headaches) from focusing attempts
- Lacrimation disturbances
- Delayed return to baseline visual function
Essential Modifications if Screen Use is Unavoidable:
- Brightness Adjustment: Reduce display luminosity to minimum tolerable levels
- Blue Light Filtering: Activate night mode or specialized filtering applications
- Text Enlargement: Increase font sizes to maximum comfortable settings
- Viewing Distance: Position screens at arm’s length or farther
- Frequent Breaks: Follow modified 20-20-20 rule (every 15 minutes, look 20 feet away for 20 seconds)
4. Near-Vision Activities and Detailed Work
Cease all reading, fine motor tasks, and close-up work requiring precise visual accommodation until pupillary function normalizes.
Physiological Limitation: Mydriatic agents specifically target the ciliary muscle responsible for lens accommodation—the mechanism allowing focus adjustment between distant and near objects. This temporary paralysis makes near-vision tasks physiologically impossible without significant strain.
Activities to Postpone:
- Book and magazine reading
- Needlework, embroidery, and sewing
- Model building and assembly work
- Jewelry repair and watchmaking
- Detailed artwork and crafting
- Document review and paperwork
- Smartphone texting and mobile applications
Adaptive Strategies for Urgent Tasks:
| Technique | Application | Effectiveness |
|---|---|---|
| Increased Working Distance | Hold materials at arm’s length | Moderate improvement |
| Magnification Aids | Reading glasses or magnifying devices | Temporary assistance |
| Large Print Materials | Newspapers, books with enlarged text | Enhanced readability |
| Voice-to-Text Technology | Smartphone dictation features | Eliminates near-vision demands |
5. Eye Rubbing and Direct Ocular Contact
Resist the urge to rub or touch your eyes despite temporary discomfort, irritation, or foreign body sensation following drop instillation.
Risks of Eye Rubbing:
- Corneal abrasions from mechanical trauma to the sensitive epithelium
- Infectious contamination introducing bacteria from hands to ocular surface
- Increased inflammation and prolonged recovery time
- Chemical irritation from residual mydriatic solution on fingers
Managing Ocular Discomfort:
- Preservative-free artificial tears provide gentle lubrication
- Cool compress application (closed eyelids only) reduces inflammation
- Gentle eyelid cleansing with sterile saline if necessary
- Consultation with eye care provider for persistent symptoms
6. Immediate Contact Lens Insertion
Delay contact lens insertion for at least 2-4 hours post-dilation to prevent complications and ensure optimal comfort.
Contact Lens Considerations: While limited research exists on specific waiting periods, clinical experience suggests postponing lens insertion until initial mydriatic effects subside. The altered tear film, potential chemical residue, and increased photosensitivity create suboptimal conditions for contact lens wear.
Recommended Protocol:
- Soft lenses: Wait minimum 2 hours, preferably until pupil size normalizes
- Rigid gas permeable lenses: Extended waiting period of 4-6 hours recommended
- Specialty lenses: Consult your optometrist for specific guidance based on lens type and eye condition
Alternative Vision Correction:
- Prescription eyeglasses during recovery period
- Over-the-counter reading glasses for temporary near-vision assistance
- Postpone non-essential activities requiring optimal vision
Recommended Actions During Recovery
Essential “Do” List for Optimal Comfort
Immediate Post-Dilation Care:
- UV Protection: Don wraparound sunglasses before leaving the clinic
- Ambient Lighting: Seek dimly lit environments and avoid harsh illumination
- Transportation Arrangements: Confirm pre-arranged safe transport home
- Digital Detox: Minimize screen exposure for 4-6 hours minimum
- Rest and Relaxation: Allow eyes to recover in comfortable, low-light settings
- Hydration: Use preservative-free artificial tears as needed for comfort
- Activity Modification: Postpone visually demanding tasks until recovery
Progressive Recovery Monitoring
Signs of Normal Recovery:
- Gradual reduction in light sensitivity
- Improved ability to focus on distant objects
- Decreased glare from artificial lighting
- Return of normal pupil size (usually within 4-6 hours)
Optimizing Recovery Environment:
- Indoor lighting: Use table lamps instead of overhead fixtures
- Window treatments: Close blinds or curtains to reduce natural light
- Entertainment alternatives: Audio books, podcasts, or music instead of visual media
- Meal preparation: Pre-plan simple foods requiring minimal preparation
Duration and Individual Factors Affecting Recovery
Understanding Your Personal Timeline
Average Recovery Expectations:
| Time Frame | Expected Improvements | Remaining Limitations |
|---|---|---|
| 0-2 hours | Severe photophobia, complete near-vision loss | All restrictions apply |
| 2-4 hours | Moderate light sensitivity, improving distance vision | Continue near-vision limitations |
| 4-6 hours | Mild residual symptoms, functional distance vision | Possible reading difficulties |
| 6-24 hours | Near-complete recovery in most patients | Occasional mild sensitivity |
Individual Variation Factors
Genetic and Physiological Influences:
Iris Pigmentation Impact: Individuals with darker brown eyes typically experience prolonged dilation effects compared to those with lighter blue or green eyes. The higher concentration of melanin pigment in darker irides binds mydriatic medications more effectively, creating extended pharmacological activity.
Age-Related Considerations:
- Pediatric patients (under 18): Often require stronger concentrations and experience longer recovery periods
- Young adults (18-40): Standard recovery times with individual variation
- Mature adults (40+): May experience faster recovery but increased accommodation difficulties
- Elderly patients (65+): Variable responses depending on overall ocular health
Medication-Specific Factors:
- Tropicamide: Shorter duration (2-6 hours), preferred for routine examinations
- Phenylephrine: Intermediate duration (4-8 hours), often combined with tropicamide
- Atropine: Extended duration (7-14 days), reserved for specific therapeutic applications
Planning Considerations for Next-Day Activities
Even after apparent recovery, some patients experience residual effects including:
- Mild photosensitivity lasting until the following morning
- Subtle accommodation difficulties affecting fine print reading
- Increased eye fatigue with prolonged visual tasks
Scheduling Recommendations:
- Book dilation appointments for late afternoon or early evening
- Avoid critical meetings or presentations the following morning
- Plan lighter work schedules for 24 hours post-procedure
- Consider taking the remainder of the examination day off work
Emergency Situations Requiring Immediate Medical Attention
Recognizing Serious Complications
While adverse reactions to routine mydriatic agents remain extremely rare, certain symptoms warrant immediate emergency evaluation for acute angle-closure glaucoma—a sight-threatening condition that can be precipitated by pupillary dilation in susceptible individuals.
Critical Warning Signs:
| Symptom Category | Specific Manifestations | Urgency Level |
|---|---|---|
| Severe Ocular Pain | Intense, stabbing eye pain unrelieved by standard measures | EMERGENCY |
| Visual Disturbances | Rainbow halos around lights, severe vision reduction | EMERGENCY |
| Systemic Symptoms | Nausea, vomiting, severe headache | EMERGENCY |
| Ocular Appearance | Marked redness, cloudy cornea, fixed pupil | EMERGENCY |
Acute Angle-Closure Glaucoma Recognition
Pathophysiology: In predisposed individuals with narrow anterior chamber angles, mydriatic-induced pupillary dilation can mechanically obstruct aqueous humor drainage, causing rapid intraocular pressure elevation to dangerous levels (often exceeding 40-50 mmHg).
Emergency Symptoms Checklist:
- ✓ Severe, unilateral eye pain described as deep, boring, or knife-like
- ✓ Dramatic vision reduction with possible light perception only
- ✓ Colored halos visible around light sources
- ✓ Corneal edema creating a cloudy, steamy appearance
- ✓ Systemic nausea and vomiting from severe pain
- ✓ Headache often described as the worst of patient’s life
Emergency Response Protocol
Immediate Actions:
- Contact emergency services or proceed directly to the nearest emergency department
- Do not delay seeking care hoping symptoms will resolve spontaneously
- Bring medication list including all eye drops used during examination
- Note time of symptom onset for medical team assessment
Specialized Emergency Eye Care Centers:
United Kingdom:
- St Thomas’ Hospital Eye Casualty (London): 24-hour emergency eye care
- King’s College Hospital (London): Comprehensive emergency ophthalmology
- St George’s Hospital (London): Acute eye conditions specialist center
- Queen Mary’s Hospital (Sidcup): Regional emergency eye services
When to Contact Your Regular Eye Care Provider: For non-emergency concerns such as:
- Prolonged recovery beyond 24 hours
- Persistent mild discomfort after expected recovery time
- Questions about resuming normal activities
- Unusual but non-threatening symptoms
General Practitioner Consultation: Contact your GP for systemic symptoms not directly related to the eyes, such as:
- Unexpected allergic reactions
- Medication interactions with current prescriptions
- General health concerns following the procedure
The 5 most frequently asked questions about “what not to do after eye dilation” along with expert answers based on the latest information:
1. What should I avoid doing right after my eyes are dilated?
After eye dilation, avoid driving, direct sunlight, bright artificial lights, using digital screens, and reading small print up close. Your vision will be blurry and your eyes will be very sensitive to light because the pupils are enlarged and let in more light than usual.
2. Why is driving not recommended after eye dilation?
Driving is unsafe because dilation causes blurred vision and increased light sensitivity, impairing your ability to see clearly and react quickly to hazards. It’s best to have someone else drive you home or use alternative transportation until your vision returns to normal.
3. How long should I avoid bright lights and screens?
The effects of dilation typically last 4 to 6 hours, sometimes longer depending on eye color and the type of drops used. During this time, avoid bright sunlight and artificial lights, including computer, phone, and TV screens, as they can cause discomfort and worsen light sensitivity.
4. Can I read or use my phone after eye dilation?
It’s best to avoid reading small fonts or using digital devices up close because your near vision will be blurry and focusing can cause eye strain, fatigue, or headaches. If you must read, hold materials at arm’s length or use a magnifier, and take frequent breaks.
5. Is it okay to rub my eyes or wear contact lenses after dilation?
Do not rub your eyes as they may feel dry or itchy after dilation; rubbing can cause irritation or damage. You can wear contact lenses, but it’s recommended to wait at least 30 minutes to an hour after dilation before putting them in to reduce discomfort.
Okay, here’s information on what not to do after eye dilation, with explanations and references to common medical advice from authoritative sources.
The primary reasons for these precautions are that dilation causes:
Mydriasis: Widening of the pupils, letting in too much light (light sensitivity/photophobia).
Cycloplegia: Paralysis of the ciliary muscle, which controls focusing, leading to blurred vision, especially for near tasks.
Scientific References
Driving a Vehicle:
Reasoning: Your vision will be blurred (both distance and near, depending on the drops used), and you will be very sensitive to light (glare from sunlight or headlights can be debilitating). This significantly impairs your ability to react to road conditions, see clearly, and judge distances.
Source/Authoritative Bodies: This is standard advice universally given by ophthalmologists and optometrists.
American Academy of Ophthalmology (AAO): Routinely advises patients to arrange for transportation after a dilated eye exam. Their patient education materials consistently state this.
Specific article/guideline (example): “Getting a Dilated Eye Exam” (Patient education materials on aao.org). While specific authors aren’t usually listed for these general patient advice pages, the AAO as an organization is the authoritative source.
National Eye Institute (NEI), part of the National Institutes of Health (NIH): Also strongly recommends having someone drive you home.
Specific article/guideline (example): “Dilated Eye Exam” information on nei.nih.gov.
American Optometric Association (AOA): Provides similar guidance.
Specific article/guideline (example): Patient resources on comprehensive eye exams often include this advice (aoa.org).
Scientific Backing (Implicit): Numerous studies on visual acuity, contrast sensitivity, and glare disability demonstrate how these functions are compromised by dilating drops, making driving unsafe. While individual studies might not be directly about “what not to do,” their findings underpin the clinical advice.
Example of a relevant study type: Research like “Effects of mydriasis on driving performance” or “Visual function under mydriasis and its implications for daily activities.” (e.g., Wood, J. M., & Lappe, M. (2016). Mydriasis impairs pooling of visual motion. Journal of Vision, 16(5), 10-10. – While this is specific, it shows how visual processing is affected. Many other studies look at acuity directly).
Operating Heavy or Dangerous Machinery:
Reasoning: Similar to driving, blurred vision and light sensitivity make it unsafe to operate machinery that requires clear vision, good depth perception, and quick reactions.
Source/Authoritative Bodies: AAO, NEI, AOA, and general occupational safety guidelines. This advice is a direct extension of the reasons for not driving.
Reading or Performing Detailed Close-Up Work:
Reasoning: Cycloplegic drops (often used in dilation, especially for children or when a refractive error measurement is critical) paralyze the focusing muscles. This makes it very difficult or impossible to focus on near objects, so reading, using a computer, or doing crafts will be challenging and frustrating.
Source/Authoritative Bodies: Standard patient advice from eye care professionals.
AAO, NEI, AOA: Their patient education materials will mention blurred near vision as a side effect.
Exposing Your Eyes to Bright Sunlight Without Sunglasses:
Reasoning: With your pupils wide open, significantly more light enters your eyes than usual. This can cause discomfort, pain (photophobia), and excessive glare.
Source/Authoritative Bodies:
AAO, NEI, AOA: All recommend wearing sunglasses (often provided by the clinic) after dilation.
Specific article/guideline (example): Patient advice sheets from any ophthalmology or optometry clinic.
Making Important Decisions Based on Visual Information:
Reasoning: If your work or activity relies on precise visual judgments (e.g., quality control, certain sports), it’s best to postpone these until the effects of dilation wear off.
Source/Authoritative Bodies: This is a logical extension of the known visual impairments and is part of general clinical advice.
General Note on Sources:
Much of this advice comes from standard clinical practice guidelines and patient education materials disseminated by major ophthalmological and optometric organizations like the American Academy of Ophthalmology (AAO), the National Eye Institute (NEI), and the American Optometric Association (AOA). These organizations synthesize vast amounts of research and clinical experience to provide these recommendations. Individual “authors” are typically the organizations themselves for these types of public health/patient care documents.
Specific research studies would more likely focus on the effects of dilating agents (e.g., “The effect of tropicamide on accommodative amplitude” or “Glare disability following pupil dilation”) rather than a study titled “What not to do after eye dilation.” The “what not to do” advice is a direct clinical application of the known scientific effects of these medications.
Important Considerations:
Duration: The effects of dilation can last for several hours (typically 4-6 hours, but sometimes longer, especially in individuals with lighter-colored eyes or with certain types of drops).
Specific Instructions: Always follow the specific instructions given to you by your eye doctor, as they may vary slightly based on the type of drops used and your individual circumstances.
Anesthetic Drops: Sometimes, anesthetic drops are used before dilating drops or for other parts of the exam (like checking eye pressure). If anesthetic drops were used, avoid rubbing your eyes, as you might not feel it if you scratch your cornea. However, this is separate from the dilation effects themselves.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.