Cataracts represent one of the most prevalent causes of vision impairment worldwide, affecting millions of individuals as they age. This progressive eye condition occurs when the eye’s natural lens becomes clouded, obstructing light from reaching the retina clearly and resulting in various degrees of visual dysfunction. Understanding the early warning signs and characteristic symptoms of cataracts is crucial for maintaining optimal eye health and preserving quality of life throughout the aging process.
Signs and Symptoms of Cataracts – This comprehensive medical guide will explore the hallmark signs of cataract development, from the initial cloudy vision to advanced symptoms like severe light sensitivity and color perception changes. We’ll examine the underlying mechanisms behind each symptom, discuss common risk factors and causes, outline diagnostic procedures, and provide essential guidance on when to seek professional eye care. Additionally, we’ll address frequently asked questions, debunk common myths, and offer practical advice for managing early-stage cataracts before surgical intervention becomes necessary.
Understanding Cataracts: The Foundation of Visual Decline
What is a Cataract?

A cataract develops when proteins within the eye’s crystalline lens begin to clump together, creating opaque areas that scatter incoming light rays instead of allowing them to pass through clearly. The lens, which sits behind the iris and pupil, normally remains transparent throughout life to focus light precisely onto the retina. However, various factors including natural aging, ultraviolet radiation exposure, diabetes, and genetic predisposition can cause these proteins to denature and aggregate.
This lens opacification progresses gradually over months or years, typically beginning as small cloudy spots that expand and merge over time. The progression rate varies significantly among individuals, with some experiencing rapid deterioration while others maintain functional vision for extended periods. Most cataracts develop bilaterally, though one eye often becomes more severely affected than the other.
The Importance of Early Recognition
Recognizing cataract symptoms early provides several critical advantages for preserving visual acuity and maintaining independence. Early detection allows ophthalmologists to monitor progression rates, optimize corrective lens prescriptions, and plan appropriate intervention timing. Patients who identify symptoms promptly can make lifestyle adjustments to compensate for visual changes and reduce accident risks, particularly when driving or navigating unfamiliar environments.
Furthermore, early awareness prevents unnecessary anxiety about unexplained vision changes and enables proactive eye care management. Many individuals initially attribute vision decline to normal aging or inadequate lighting, delaying essential medical evaluation that could significantly improve their quality of life.
Primary Signs and Symptoms of Cataracts
1. Cloudy or Blurry Vision: The Hallmark Indicator
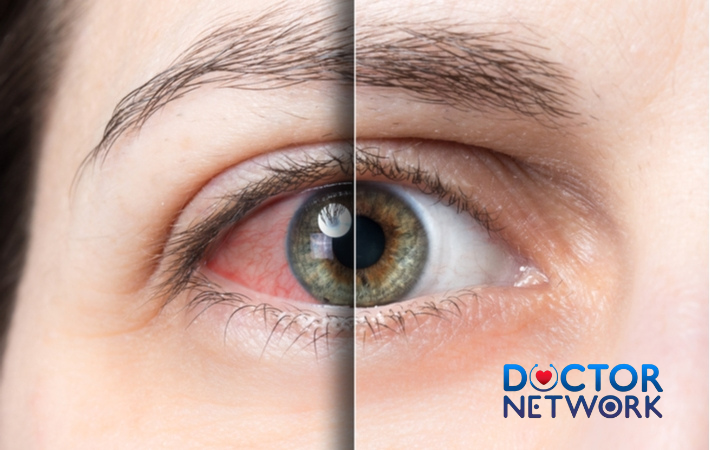
The most characteristic symptom of cataract formation manifests as progressive clouding or blurring of vision, often described by patients as looking through a dirty window, frosted glass, or dense fog. This visual disturbance results from light scattering as it encounters protein aggregations within the lens, preventing clear image formation on the retina.
Initially, this cloudiness may affect only small portions of the visual field, causing minor inconveniences like difficulty reading fine print or recognizing distant faces. As the cataract matures, the affected area expands, encompassing larger portions of the lens and significantly impairing visual sharpness across all distances. Patients frequently report that increasing lighting or magnification provides temporary relief, but these compensatory measures become less effective as the condition progresses.
The impact on daily activities becomes increasingly pronounced as cataracts advance. Reading comprehension decreases due to reduced contrast sensitivity, making newspapers, books, and digital screens appear washed out or indistinct. Driving safety becomes compromised, particularly during challenging conditions like dawn, dusk, or inclement weather when visual demands are highest.
2. Increased Light Sensitivity and Glare Problems
Photophobia, or excessive sensitivity to bright light, represents another cardinal symptom of cataract development. The clouded lens causes incoming light to scatter in multiple directions rather than focusing it properly, creating uncomfortable glare and making normal lighting levels feel overwhelmingly bright.
Patients commonly experience significant discomfort when exposed to:
- Direct sunlight or bright outdoor lighting
- Automobile headlights during night driving
- Indoor fluorescent or LED lighting
- Computer screens and digital devices
- Camera flashes or photography lighting
This light scattering phenomenon also produces characteristic halos or rings around light sources, particularly noticeable in low-light conditions. These optical aberrations make night driving especially hazardous, as oncoming headlights create blinding glare surrounded by prominent halos that obscure road visibility and traffic signs.
The severity of photophobia often correlates with cataract density and location within the lens. Central cataracts typically produce more pronounced glare problems than peripheral opacities, as they directly interfere with the primary optical pathway.
3. Compromised Night Vision and Low-Light Performance
Nyctalopia, or poor night vision, develops as cataracts reduce the eye’s ability to function effectively in dim lighting conditions. The clouded lens decreases overall light transmission to the retina while simultaneously reducing contrast sensitivity, making it difficult to distinguish objects from backgrounds in low-light environments.
This symptom particularly affects:
- Night driving safety and confidence
- Navigation in dimly lit indoor spaces
- Outdoor activities during evening hours
- Reading or detailed work in subdued lighting
- Stair climbing and mobility in dark areas
The combination of reduced light transmission and increased intraocular light scatter creates a “double burden” for night vision. Not only does less light reach the retina, but the available light becomes diffused throughout the eye, washing out contrast and making fine details nearly impossible to discern.
Many patients initially compensate by avoiding night driving or installing brighter lighting in their homes. However, as cataracts progress, even these adaptations become insufficient, leading to social isolation and reduced independence.
table 1: Comparison of Cataract Symptoms vs. Other Eye Conditions
| Symptom | Cataracts | Glaucoma | Macular Degeneration | Dry Eye Syndrome |
|---|---|---|---|---|
| Blurry Vision | Gradual, overall haziness | Peripheral vision loss first | Central vision affected | Intermittent, fluctuating |
| Light Sensitivity | Significant glare, halos | Minimal | Moderate | Mild to moderate |
| Night Vision | Severely impaired | Tunnel vision effect | Variable | Normal typically |
| Color Changes | Yellow/brown tinting | Normal color vision | Color distortion possible | Normal color vision |
| Pain/Discomfort | Usually painless | Often painless | Painless | Burning, scratching sensation |
| Progression | Months to years | Variable, can be rapid | Progressive over years | Chronic, fluctuating |
4. Color Perception Alterations and Fading
Cataracts frequently cause significant changes in color perception, with affected individuals experiencing fading, dulling, or yellowing of their visual world. This occurs because the clouded lens acts as a filter, absorbing certain wavelengths of light while allowing others to pass through more readily.
The most common color changes include:
- Overall reduction in color vibrancy and saturation
- Yellowish or brownish tinting of white objects
- Difficulty distinguishing between similar hues (blues and purples)
- Reduced ability to appreciate subtle color variations
- Colors appearing washed out or muted
These alterations can significantly impact quality of life, affecting enjoyment of art, nature, fashion choices, and food presentation. Many patients don’t initially recognize these changes, attributing them to poor lighting or fading photographs until the condition becomes quite advanced.
Interestingly, some individuals only become aware of their color perception problems after successful cataract surgery, when they’re amazed by the sudden return of vivid, saturated colors they hadn’t realized they were missing.
5. Frequent Changes in Eyeglass Prescriptions
As cataracts develop, they alter the eye’s refractive properties, causing frequent changes in vision correction needs. Patients often require increasingly stronger prescriptions within relatively short timeframes, sometimes needing new glasses every few months instead of the typical every few years.
This occurs because the changing density and shape of the clouded lens affects how light rays bend as they enter the eye. The irregular protein deposits within the lens create areas of varying optical power, making it difficult to achieve consistent vision correction with standard eyeglasses or contact lenses.
Some individuals with nuclear cataracts (affecting the lens center) may experience temporary improvement in near vision, called “second sight.” This phenomenon occurs when the cataract increases the lens’s refractive power, temporarily reducing presbyopia. However, this improvement is short-lived and eventually gives way to overall vision deterioration.
6. Double Vision in One Eye (Monocular Diplopia)
Monocular diplopia, or double vision occurring in a single eye, can develop when cataracts create irregular optical surfaces within the lens. Unlike double vision caused by eye muscle problems (which affects both eyes), monocular diplopia persists even when the unaffected eye is covered.
This symptom results from light rays taking multiple paths through areas of varying lens density, creating duplicate or multiple images of the same object. The effect may be subtle initially, appearing as slight image ghosting or shadowing, but can progress to distinct double images that significantly interfere with visual tasks.
Monocular diplopia particularly affects:
- Reading, causing text to appear doubled or overlapped
- Driving, creating multiple images of traffic signs or vehicles
- Computer work, making screen content difficult to interpret
- Fine detailed tasks requiring precise visual focus
Common Causes and Risk Factors

Age-Related Changes: The Primary Culprit
The natural aging process represents the most significant risk factor for cataract development, with over 90% of cases classified as age-related cataracts. Beginning around age 40, the lens proteins start to undergo gradual changes that increase their susceptibility to aggregation and clouding.
Several age-related factors contribute to cataract formation:
- Decreased antioxidant levels within the lens
- Accumulated oxidative damage from ultraviolet radiation
- Reduced lens fiber flexibility and transparency
- Changes in lens metabolism and protein synthesis
- Gradual dehydration of lens tissues
By age 80, virtually everyone has some degree of cataract formation, though not all require surgical intervention. The timing and severity of cataract development vary significantly based on genetic factors, lifestyle choices, and overall health status.
Associated Health Conditions
Multiple medical conditions significantly increase cataract risk and can accelerate their progression:
Diabetes Mellitus: Elevated blood glucose levels cause proteins to undergo glycation, making them more likely to clump together. Diabetic patients often develop cataracts at younger ages and experience more rapid progression.
Corticosteroid Use: Prolonged use of corticosteroid medications, whether oral, topical, or inhaled, substantially increases cataract risk. These medications alter lens metabolism and accelerate protein changes.
Previous Eye Trauma: Blunt force injuries, penetrating wounds, or severe chemical burns can damage lens fibers and trigger premature cataract formation.
Chronic Eye Inflammation: Conditions like uveitis create an inflammatory environment that promotes lens protein denaturation and clouding.
Previous Eye Surgery: Certain ocular procedures, particularly retinal surgeries, can accelerate cataract development in affected eyes.
Lifestyle Risk Factors
Several modifiable lifestyle factors significantly influence cataract development:
Ultraviolet Radiation Exposure: Chronic exposure to UV-A and UV-B radiation without adequate eye protection causes cumulative damage to lens proteins. Individuals with outdoor occupations or those living in high-altitude or equatorial regions face elevated risks.
Tobacco Use: Smoking introduces numerous toxic compounds into the bloodstream that can accumulate in ocular tissues. Smokers face approximately double the risk of cataract development compared to non-smokers.
Excessive Alcohol Consumption: Heavy alcohol use may contribute to nutritional deficiencies and oxidative stress that promote cataract formation.
Poor Nutrition: Diets lacking in antioxidants, vitamins C and E, lutein, and zeaxanthin may fail to provide adequate protection against oxidative lens damage.
table 2: Risk Factors and Their Impact on Cataract Development
| Risk Factor | Relative Risk Increase | Age of Typical Onset | Prevention Strategies |
|---|---|---|---|
| Advanced Age (>70) | 5-10x normal | 60-80 years | Regular eye exams |
| Diabetes | 2-5x normal | 40-60 years | Blood sugar control |
| Smoking | 2-3x normal | 50-70 years | Smoking cessation |
| UV Exposure | 1.5-3x normal | 50-75 years | UV-blocking sunglasses |
| Steroid Use | 3-10x normal | Any age | Minimize use when possible |
| Eye Trauma | Variable | Any age | Eye protection |
| Family History | 1.5-2x normal | Similar to relatives | Regular monitoring |
Genetic Predisposition
Family history plays an important role in cataract susceptibility, with genetic factors influencing both the timing of onset and progression rate. Individuals with parents or siblings who developed cataracts often experience similar patterns of lens changes.
Several genes have been identified that affect lens protein structure and function, making some individuals more susceptible to cataract formation. While genetic predisposition cannot be modified, awareness of family history allows for more vigilant monitoring and earlier intervention when appropriate.
When to Seek Professional Eye Care
Critical Warning Signs Requiring Immediate Attention
While most cataracts develop gradually over months or years, certain symptoms warrant urgent ophthalmologic evaluation:
- Sudden, severe vision loss in one or both eyes
- Acute eye pain accompanied by vision changes
- Seeing flashing lights or new floating spots
- Curtain-like shadow across the visual field
- Significant reduction in peripheral vision
- Double vision that doesn’t resolve when covering one eye
These symptoms may indicate serious complications such as retinal detachment, acute glaucoma, or other sight-threatening conditions that require immediate medical intervention.
Progressive Symptoms Indicating Professional Evaluation
Schedule an eye examination when experiencing:
- Gradual vision decline interfering with daily activities
- Increasing difficulty reading or performing close work
- Problems with night driving or bright light sensitivity
- Frequent changes in eyeglass prescription requirements
- Colors appearing faded or yellowed
- Halos around lights becoming more prominent
Early professional evaluation allows for proper diagnosis, monitoring of progression, and timely intervention planning. Many patients benefit from non-surgical management strategies during early cataract stages.
Comprehensive Eye Examination Process
A thorough cataract evaluation involves several specialized tests and procedures:
Visual Acuity Assessment: Standard eye chart testing measures the sharpness of vision at various distances, providing baseline measurements for monitoring progression.
Slit-Lamp Examination: This microscopic evaluation allows detailed visualization of the lens structure, identifying the type, location, and density of cataracts present.
Dilated Fundus Examination: Pupil dilation enables comprehensive evaluation of the retina and optic nerve, ruling out other conditions that might contribute to vision problems.
Tonometry: Measurement of intraocular pressure helps detect glaucoma, which commonly coexists with cataracts in older adults.
Contrast Sensitivity Testing: This assessment evaluates the ability to distinguish objects from backgrounds, often affected early in cataract development.
Glare Testing: Specialized equipment measures how bright lights affect vision quality, helping determine functional impairment levels.
Brief Overview of Cataract Management
Early Stage Management Strategies
Before surgical intervention becomes necessary, several approaches can help manage mild cataract symptoms:
Optimized Corrective Lenses: Updated eyeglass prescriptions with anti-reflective coatings can improve visual clarity and reduce glare sensitivity.
Enhanced Lighting: Brighter reading lights, task-specific illumination, and reduced ambient lighting can compensate for decreased light transmission.
Lifestyle Modifications: Avoiding challenging visual situations like night driving, using magnification aids, and organizing living spaces for better visibility.
UV Protection: Consistent use of high-quality sunglasses can slow cataract progression by reducing ongoing ultraviolet damage.
Surgical Intervention: The Definitive Treatment
Cataract surgery remains the only definitive treatment for advanced cataracts, involving removal of the clouded natural lens and replacement with an artificial intraocular lens (IOL). This procedure boasts over 95% success rates and typically results in significant vision improvement.
Modern cataract surgery utilizes advanced techniques including:
- Phacoemulsification with ultrasonic lens fragmentation
- Small-incision procedures requiring no sutures
- Premium IOL options correcting astigmatism and presbyopia
- Laser-assisted surgical techniques for enhanced precision
The decision for surgical timing depends on symptom severity, functional impairment, and patient preferences rather than arbitrary visual acuity measurements.
Patient Experience and Coping Strategies
Individual Variation in Symptom Presentation
Cataract symptoms manifest differently among individuals, influenced by factors including cataract type, location, lifestyle demands, and personal visual needs. Some patients experience primarily distance vision problems, while others struggle mainly with near tasks or light sensitivity.
Professional drivers, artists, or individuals with demanding visual occupations may notice functional impairment earlier than those with less visually demanding lifestyles. Understanding these individual differences helps healthcare providers tailor management recommendations appropriately.
Initial Coping Mechanisms
Many patients unconsciously develop compensatory strategies as cataracts progress:
- Increasing lighting levels throughout their homes
- Avoiding challenging visual situations like night driving
- Using magnification aids for reading and detailed tasks
- Positioning themselves closer to television screens or computer monitors
- Relying more heavily on other senses for navigation and identification
While these adaptations can temporarily maintain independence, they often indicate advancing cataract development requiring professional evaluation.
Myth vs. Fact: Addressing Common Misconceptions
list 1: Common Cataract Myths Debunked
Myth: Cataracts are removed with laser surgery Fact: Most cataract surgery uses ultrasonic energy (phacoemulsification) to break up the clouded lens, though laser-assisted techniques are available for certain steps
Myth: Cataracts grow back after surgery Fact: Cataracts cannot recur because the natural lens is permanently removed; however, the lens capsule may become cloudy (posterior capsule opacification) requiring simple laser treatment
Myth: Cataract surgery should be delayed as long as possible Fact: Modern surgery is highly safe and effective; delaying can increase risks and reduce quality of life unnecessarily
Myth: Reading in dim light causes cataracts Fact: While poor lighting can strain eyes, it doesn’t cause cataracts; UV exposure and aging are primary risk factors
Myth: Eye drops can dissolve cataracts Fact: No medications currently available can reverse established cataracts; surgery remains the only effective treatment
Preventive Measures and Risk Mitigation
UV Protection Strategies
Consistent ultraviolet radiation protection represents one of the most effective preventive measures against cataract development:
- Wear high-quality sunglasses blocking 99-100% of UV-A and UV-B radiation
- Choose wraparound styles providing peripheral coverage
- Use wide-brimmed hats for additional protection
- Avoid prolonged sun exposure during peak hours (10 AM – 4 PM)
- Consider UV-blocking contact lenses for additional protection
Nutritional Approaches
Research suggests certain nutrients may help protect against cataract formation:
- Antioxidants: Vitamins C and E combat oxidative damage
- Carotenoids: Lutein and zeaxanthin concentrate in ocular tissues
- Omega-3 Fatty Acids: Support overall eye health and reduce inflammation
- Zinc: Essential for maintaining lens clarity and function
A diet rich in colorful fruits, vegetables, fish, and nuts provides these protective compounds naturally.
Health Management
Optimal management of underlying health conditions significantly reduces cataract risk:
- Maintain tight blood glucose control in diabetes
- Use corticosteroids only when medically necessary
- Protect eyes from trauma with appropriate safety equipment
- Manage blood pressure and cardiovascular health
- Avoid tobacco use and limit alcohol consumption
list 2: Daily Activities Most Affected by Cataracts
Driving-Related Challenges:
- Night driving becomes increasingly dangerous
- Glare from oncoming headlights creates temporary blindness
- Traffic signs and signals become difficult to read
- Depth perception problems affect parking and lane changes
Reading and Close Work:
- Fine print becomes illegible despite magnification
- Computer screens appear washed out or unclear
- Medication labels and important documents become unreadable
- Hobbies requiring detailed vision become frustrating
Social and Recreational Activities:
- Facial recognition becomes difficult at moderate distances
- Television viewing requires closer seating positions
- Playing cards or board games becomes challenging
- Cooking and food preparation safety concerns arise
Mobility and Safety Concerns:
- Stair navigation, especially in dim lighting
- Identifying obstacles or changes in surface elevation
- Reading street signs and house numbers
- Distinguishing between similar objects or colors
Early Detection Benefits and Long-term Outcomes
Advantages of Prompt Recognition
Identifying cataract symptoms early provides numerous benefits for maintaining visual function and quality of life:
- Optimized Non-surgical Management: Early detection allows for effective use of stronger lighting, anti-glare coatings, and updated prescriptions
- Informed Lifestyle Planning: Patients can make appropriate modifications to maintain independence and safety
- Timely Surgical Planning: Early diagnosis enables optimal timing for surgical intervention before severe functional impairment occurs
- Monitoring Progression: Regular follow-up appointments track changes and guide treatment decisions
- Prevention of Secondary Problems: Early intervention reduces risks of falls, accidents, and social isolation
Long-term Visual Prognosis
The long-term outlook for cataract patients remains excellent with appropriate management. Modern surgical techniques achieve outstanding results, with most patients experiencing significant vision improvement and enhanced quality of life. Success rates exceed 95%, with complications occurring in fewer than 2% of cases.
Post-surgical visual outcomes typically include:
- Restoration of clear, sharp vision
- Elimination of glare and light sensitivity problems
- Improved color perception and contrast sensitivity
- Enhanced ability to perform daily activities independently
- Reduced dependence on corrective lenses (with premium IOLs)
table 3: Timeline of Cataract Progression and Management
| Stage | Duration | Visual Symptoms | Management Options | Surgical Consideration |
|---|---|---|---|---|
| Early | 1-3 years | Mild blurring, slight glare | Updated glasses, better lighting | Not typically recommended |
| Moderate | 2-5 years | Noticeable vision loss, color changes | Stronger prescriptions, lifestyle modifications | Consider if affecting daily activities |
| Advanced | 3-7 years | Significant impairment, safety concerns | Limited non-surgical options | Strongly recommended |
| Mature | Variable | Severe vision loss, possible complications | Surgical intervention urgent | Essential for vision restoration |
Understanding the typical progression timeline helps patients and healthcare providers make informed decisions about treatment timing and intervention strategies.
Conclusion: Taking Control of Your Eye Health
Cataracts represent a manageable condition when properly understood and addressed through appropriate medical care. Recognizing the early warning signs—cloudy vision, light sensitivity, poor night vision, color changes, frequent prescription changes, and monocular double vision—enables prompt intervention and optimal outcomes.
While cataract development often accompanies natural aging, understanding risk factors allows for preventive measures that may delay onset or slow progression. Regular comprehensive eye examinations remain essential for early detection and appropriate management planning.
Modern cataract treatment offers excellent results, with surgical intervention providing safe, effective restoration of clear vision for millions of patients annually. By staying informed about symptoms, maintaining regular eye care, and working closely with qualified eye care professionals, individuals can preserve their vision and maintain their quality of life throughout the aging process.
The key to successful cataract management lies in education, early recognition, and timely professional intervention. Don’t let vision changes go unaddressed—your eyes deserve the best possible care to keep you seeing clearly for years to come.
5 frequently asked questions
What are the first signs of cataracts?
The earliest signs often include difficulty with night vision and glare from headlights while driving at night. Other early symptoms are mild blurring of vision, halos around lights, glare in sunlight, and trouble reading small print. People may also notice cloudy or foggy vision, colors appearing faded or less vibrant, and increased sensitivity to bright lightHow do cataracts affect vision?
Cataracts cause the lens of the eye to become cloudy, which blurs and dulls vision. This can make it hard to see faces, read, or recognize objects clearly. Colors may look faded or have a yellowish tint. People with cataracts often experience glare, halos around lights, double vision in one eye, and difficulty seeing in low light or at nightAt what age do cataracts usually develop?
Cataracts most commonly develop as people age, typically starting in their 50s or 60s. By age 80, about 85% of people have some degree of cataract. However, cataracts can occur at any age due to other causes such as eye injury, certain medications, or congenital conditionsAre cataracts painful?
Cataracts themselves do not cause pain or discomfort. They usually do not cause redness or irritation of the eyes. However, some symptoms like glare or double vision can be uncomfortable and interfere with daily activitiesHow quickly do cataracts progress and when should surgery be considered?
The progression of cataracts varies widely among individuals and cannot be precisely predicted. Some cataracts develop slowly over many years, while others progress more rapidly. Surgery is typically recommended when vision loss from cataracts interferes with daily activities or quality of life, such as difficulty driving, reading, or recognizing faces
Scientific Evidence
1. Blurry, Cloudy, or Dim Vision
This is the most reported symptom of cataracts. The clouding of the lens scatters and blocks the light that passes through it, preventing a sharply defined image from reaching the retina.
Description: Patients often describe their vision as looking through a “foggy” or “frosty” window. The effect is constant and cannot be cleared by blinking.
Evidence/Source: This is universally cited as the primary symptom by all major health organizations. The National Eye Institute (NEI), part of the U.S. National Institutes of Health, provides a clear, authoritative overview.
Source: National Eye Institute (NEI), U.S. Department of Health and Human Services.
Author: The information is published by the institution itself, representing a consensus of medical experts.
2. Increased Difficulty with Vision at Night
As the cataract worsens, it significantly reduces the amount of light reaching the retina, making vision in low-light conditions particularly challenging.
Description: Needing brighter light for reading or other close activities, and experiencing poor vision while driving at night.
Evidence/Source: The American Academy of Ophthalmology (AAO), the world’s largest association of eye physicians and surgeons, details this in its comprehensive patient guide.
Source: American Academy of Ophthalmology (AAO).
Author: The content is reviewed by ophthalmologists who are members of the Academy.
Link: AAO – Cataract Symptoms
3. Sensitivity to Light and Glare (Photophobia)
Light scattering caused by the opacities in the lens leads to significant issues with glare.
Description: Oncoming headlights, bright sunlight, or even indoor lamps may seem excessively bright or cause halos to appear around them. This can be debilitating, especially for drivers.
Scientific Study: A foundational study explored the functional disability caused by glare in cataract patients. It measured how glare sources degraded visual performance, scientifically validating this common complaint.
Study Title: “Glare and Contrast Sensitivity in Cataract and After Cataract Surgery”
Author(s): P. Artal, M. C. Nalda, S. G. Marcos, and D. G. Green.
Source: Investigative Ophthalmology & Visual Science (IOVS), Vol. 34, 1993.
Summary: The research demonstrated that light scattering within the eye is significantly higher in cataract patients, which directly correlates with their complaints of glare and reduced contrast sensitivity.
Link: IOVS Study Abstract
4. Fading or Yellowing of Colors
The lens itself can turn yellowish or brownish as a nuclear cataract develops. This acts like a filter, changing the way the patient perceives color.
Description: Colors may appear less vibrant, and patients may have difficulty distinguishing between certain shades, particularly blues and purples.
Evidence/Source: The Cleveland Clinic explains this phenomenon clearly, noting that the world may begin to take on a “brownish or yellowish tint.”
Source: Cleveland Clinic.
Author: Published and medically reviewed by the institution’s experts.
Scientific Study: Research has quantified this color vision loss using standardized tests.
Study Title: “Evaluation of colour vision in patients with cataracts”
Author(s): M. A. del Buey, L. E. Pablo, J. A. Cristóbal, et al.
Source: Archivos de la Sociedad Española de Oftalmología, Vol. 81, 2006.
Summary: The study used the Farnsworth-Munsell 100 hue test and found a significant blue-yellow color vision defect in patients with nuclear and cortical cataracts, which improved after surgery.
Link: PubMed Link to Study
5. Monocular Diplopia (Double Vision in a Single Eye)
This is a very specific symptom where a patient sees multiple images from just one eye.
Description: Seeing a “ghost” or “double” image, especially when looking at high-contrast objects like text on a screen. This is caused by light splitting into two or more paths as it passes through different parts of the clouded lens.
Evidence/Source: The Mayo Clinic lists this as a key symptom, distinguishing it from binocular double vision (which occurs when the eyes are misaligned).
Source: Mayo Clinic.
Author: Staff of the Mayo Clinic.
6. Myopic Shift or “Second Sight”
In the early stages of a nuclear cataract, the center of the lens can become denser, increasing its focusing power.
Description: Individuals who were previously farsighted (hyperopic) or needed reading glasses may find that their near vision temporarily improves. This phenomenon is often called “second sight.” However, this improvement is short-lived, as the cataract will eventually worsen and cloud vision at all distances.
Scientific Explanation: This is a well-documented clinical sign. The increased refractive index of the lens nucleus causes a “myopic shift,” making the eye more nearsighted.
Source: Kanski’s Clinical Ophthalmology: A Systematic Approach – a leading international textbook for ophthalmologists.
Author(s): Brad Bowling (formerly Jack J. Kanski).
Summary: Chapter 6 on “Lens” details the pathophysiology of different cataract types, including the myopic shift associated with nuclear sclerosis. While a direct link to a free version of the textbook is not available, this principle is foundational in ophthalmology education and is referenced in clinical practice guidelines. The AAO also mentions this phenomenon.
Link (Reference): AAO – Preferred Practice Pattern for Adult Cataract
7. Frequent Changes in Eyeglass or Contact Lens Prescription
As the cataract progresses, it continuously changes the refractive error of the eye.
Description: A patient may find that their glasses or contact lenses no longer seem to work well and that their prescription needs to be updated frequently.
Evidence/Source: This is a logical consequence of the progressive nature of cataracts and is cited as a symptom by virtually all major eye care organizations, including the ones listed above (NEI, AAO).
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.