A herniated disc can transform your daily life into a constant battle against debilitating pain, numbness, and restricted movement. Understanding the recovery process becomes crucial for maintaining hope and adhering to treatment protocols during this challenging journey. Recognizing the subtle yet significant signs that indicate your herniated disc is healing empowers you to track progress, make informed decisions about your care, and maintain motivation throughout the recovery timeline.
Signs a Herniated Disc Is Healing – This comprehensive guide explores the physiological healing mechanisms, patient-reported improvements, objective medical confirmations, and long-term recovery strategies for herniated disc rehabilitation. We’ll examine pain reduction patterns, mobility restoration, neurological symptom improvement, quality of life enhancement, and medical assessment techniques. Additionally, we’ll address the psychological aspects of recovery, warning signs requiring immediate attention, and prevention strategies to maintain spinal health.
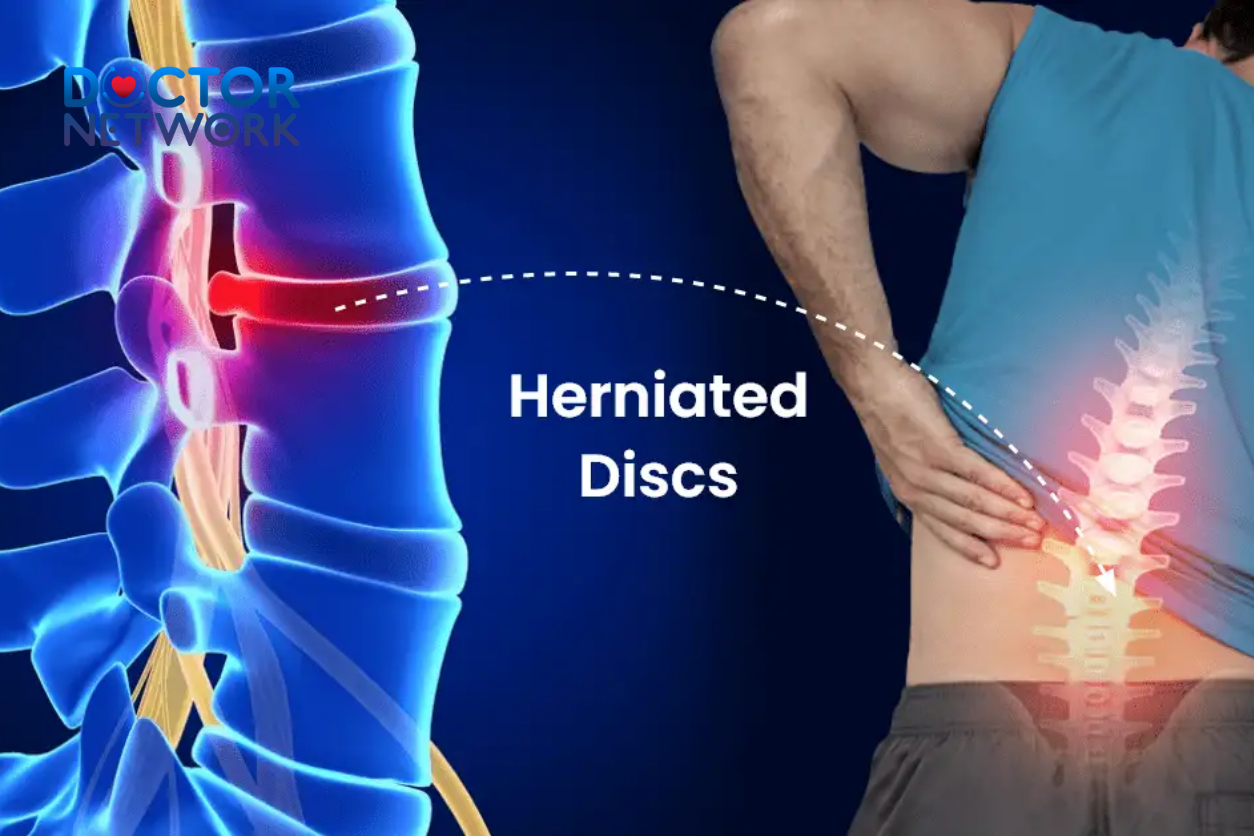
A herniated disc occurs when the soft, gel-like nucleus pulposus pushes through a tear in the outer annulus fibrosus of an intervertebral disc. This protrusion can compress or irritate nearby nerve roots, causing localized back pain and radiating symptoms like sciatica or cervical radiculopathy.
Understanding the Healing Process: The Body’s Natural Recovery Mechanism
Physiological Mechanisms of Healing
Your body possesses remarkable self-healing capabilities that work continuously to repair herniated disc damage through multiple interconnected processes. The primary healing mechanism involves natural resorption, where specialized immune cells called macrophages gradually break down and absorb the extruded disc material that’s pressing against nerve structures. This biological process typically occurs over 6-12 months, with the herniated portion often shrinking by 60-80% of its original size.
Inflammation reduction represents another critical component of disc healing, as your body’s initial inflammatory response gradually subsides. During acute injury, inflammatory mediators like cytokines and prostaglandins flood the affected area, causing pain, swelling, and nerve irritation. As healing progresses, anti-inflammatory mechanisms activate, reducing these chemical irritants and allowing nerve tissues to recover their normal function.
Tissue regeneration and remodeling complete the healing triad, with collagen fibers reorganizing to strengthen the damaged annulus fibrosus. While complete restoration of original disc architecture rarely occurs, the body creates stable scar tissue that can effectively contain the nucleus pulposus and prevent further herniation.
Key Subjective Signs of Healing (Patient-Reported)
A. Significant Pain Reduction
Decreased pain intensity serves as the most noticeable indicator that your herniated disc is beginning to heal. Patients typically experience a gradual reduction in pain severity, measured on a scale from 10 (excruciating) to 0 (pain-free). This improvement often follows a fluctuating pattern rather than a steady decline, with good days becoming more frequent than bad days.
The frequency of pain episodes also diminishes as healing progresses. Instead of constant, unrelenting discomfort, you may notice pain-free intervals that gradually extend in duration. These respites from pain allow your nervous system to reset and reduce central sensitization, creating a positive feedback loop that supports continued recovery.
Radiating pain reduction represents one of the most significant healing milestones for herniated disc patients. Sciatica symptoms, including shooting pain down the leg, typically improve before localized back pain subsides. This occurs because nerve decompression allows proper signal transmission, reducing the abnormal pain messages traveling along affected nerve pathways.
Pain centralization, where discomfort moves from the extremities back toward the spine, indicates reduced nerve impingement and improved disc positioning. This phenomenon suggests that pressure on nerve roots is decreasing, allowing normal neurological function to resume.
| Pain Reduction Timeline | Typical Symptoms | Recovery Significance |
|---|---|---|
| Weeks 1-2 | Slight reduction in radiating pain intensity | Early inflammation resolution |
| Weeks 3-6 | Decreased frequency of severe pain episodes | Nerve decompression beginning |
| Weeks 6-12 | Pain centralization toward spine | Significant structural improvement |
| 3-6 Months | Consistent pain-free periods | Advanced healing and tissue repair |
B. Improved Mobility and Physical Function
Enhanced range of motion signals that your spine is regaining its normal mechanical function. Initially restricted movements like forward bending, rotation, or extension become less painful and more fluid. This improvement reflects reduced muscle guarding, decreased inflammation around spinal joints, and restoration of normal biomechanics.
Daily activities that once triggered severe pain become manageable again. Simple tasks like getting dressed, climbing stairs, lifting groceries, or sitting at a desk for extended periods gradually return to your normal routine. These functional improvements often occur in stages, with less demanding activities improving first, followed by more complex movements.
Postural improvements accompany mobility gains as your body stops compensating for pain through protective positioning. The characteristic lean or tilt that many herniated disc patients develop begins to normalize, indicating that underlying nerve irritation is subsiding and muscle balance is being restored.
C. Reduction in Neurological Symptoms
Diminishing numbness and tingling sensations indicate that compressed nerves are recovering their normal function. These paresthesias, often described as “pins and needles,” typically improve gradually as nerve conduction pathways heal. The restoration of normal sensation follows specific dermatome patterns, allowing healthcare providers to track recovery progress objectively.
Strength restoration in affected muscle groups represents another crucial healing indicator. Weakness in specific muscles supplied by compressed nerve roots begins to improve as the nerve regains its ability to transmit motor signals effectively. This recovery often follows a predictable pattern, with larger muscle groups recovering before fine motor control returns.
Recovery Timeline for Neurological Symptoms:
- Immediate (0-2 weeks): Acute inflammation peaks, symptoms may fluctuate
- Early recovery (2-6 weeks): Gradual reduction in radiating pain and tingling
- Progressive healing (6-12 weeks): Strength improvements become noticeable
- Advanced recovery (3-6 months): Fine motor control and full sensation return
- Maintenance phase (6+ months): Continued strengthening and functional optimization
D. Improved General Well-being and Quality of Life
Better sleep quality emerges as pain levels decrease and comfortable positioning becomes possible again. Chronic pain disrupts normal sleep architecture, preventing restorative deep sleep phases. As healing progresses, patients report fewer nighttime awakenings, easier sleep initiation, and more refreshing rest patterns.
Mood improvements and decreased irritability naturally follow pain reduction and improved sleep. Chronic pain affects neurotransmitter balance, particularly serotonin and dopamine levels, contributing to depression and anxiety. The restoration of normal pain processing allows these chemical systems to rebalance, supporting emotional well-being.
The ratio of good days to bad days shifts progressively in favor of better functioning. This non-linear healing pattern means that while setbacks may occur, the overall trend shows increasing numbers of pain-free or low-pain days compared to high-pain episodes.
Objective Medical Confirmation of Healing
The Clinician’s Assessment Perspective
Healthcare providers use standardized examination techniques to objectively measure your recovery progress beyond subjective symptom reports. These assessments provide quantifiable data about neurological function, structural improvements, and functional capacity that complement your personal healing experience.
Physical examination findings change systematically as healing occurs. Straight leg raise tests become less painful, deep tendon reflexes normalize, and muscle strength measurements improve. These objective markers help healthcare providers distinguish between actual healing and temporary symptom fluctuation.
Neurological examinations reveal specific patterns of recovery that correlate with anatomical healing. Sensory testing using light touch, pinprick, and vibration assessment demonstrates nerve function restoration. Motor testing through manual muscle testing and functional movement screens quantifies strength improvements and movement quality enhancement.
Follow-up Imaging and Diagnostic Confirmation
Advanced imaging studies, while not always necessary for confirming clinical healing, can provide objective evidence of structural improvement. MRI scans may reveal reduction in disc herniation size, decreased nerve root compression, and resolution of surrounding inflammation. These findings offer compelling visual confirmation of the healing process.
Electromyography (EMG) and nerve conduction studies can demonstrate improved nerve function by measuring electrical activity in affected muscles and nerve transmission speeds. These tests are particularly valuable when neurological symptoms were prominent initially.
| Assessment Method | What It Measures | Healing Indicators |
|---|---|---|
| Physical Exam | Range of motion, strength, reflexes | Improved flexibility, normal reflexes, increased strength |
| MRI Imaging | Disc size, nerve compression | Reduced herniation, less nerve impingement |
| EMG/NCS | Nerve and muscle function | Normal electrical activity, improved conduction |
| Functional Testing | Real-world movement capacity | Better lifting, walking, and daily activity performance |
Factors Influencing Healing and What to Expect
Non-Linear Healing Journey
Recovery from herniated disc injury rarely follows a predictable, straight-line improvement pattern. Instead, expect fluctuations in symptoms, with periods of improvement followed by temporary setbacks. This variability occurs due to multiple factors including activity levels, weather changes, stress, sleep quality, and the complex nature of tissue healing processes.
Understanding this non-linear pattern helps prevent discouragement during temporary symptom flare-ups. These setbacks don’t indicate treatment failure or worsening injury; they represent normal healing variations. Maintaining perspective during difficult days becomes easier when you recognize the overall trend toward improvement.
Progress tracking through symptom journals, pain scales, and functional assessments reveals the underlying positive trajectory despite day-to-day fluctuations. Many patients find that graphing their symptoms over time clearly demonstrates improvement that might not be apparent from daily experience alone.
Adherence to Treatment Plan
Consistent compliance with prescribed therapies significantly influences healing outcomes and recovery timelines. Physical therapy exercises maintain joint mobility, strengthen supporting muscles, and promote proper movement patterns that prevent re-injury. Skipping sessions or performing exercises incorrectly can delay healing and increase recurrence risk.
Medication protocols serve specific purposes during different healing phases. Anti-inflammatory drugs reduce tissue swelling and pain during acute phases, while muscle relaxants prevent protective spasms that can worsen symptoms. Following prescribed dosing schedules optimizes therapeutic benefits while minimizing side effects.
Activity modification guidelines protect healing tissues while maintaining necessary movement for recovery. Complete bed rest is rarely recommended, but avoiding activities that exacerbate symptoms allows damaged structures to heal without additional trauma.
Individual Variability Factors
Age significantly impacts healing speed and completeness, with younger patients typically experiencing faster recovery due to more robust cellular repair mechanisms and better circulation. However, older adults can achieve excellent outcomes with appropriate treatment and realistic expectations.
Overall health status affects healing capacity through multiple pathways. Cardiovascular fitness influences tissue oxygenation and nutrient delivery to healing structures. Diabetes, smoking, and other systemic conditions can impair the healing process by affecting circulation and cellular metabolism.
Key Factors Affecting Healing Speed:
- Age and fitness level: Younger, fitter individuals typically heal faster
- Severity of initial injury: Larger herniations may require longer recovery periods
- Treatment compliance: Consistent therapy adherence accelerates healing
- Lifestyle factors: Smoking, poor nutrition, and stress can delay recovery
- Comorbid conditions: Diabetes, arthritis, and other health issues affect healing
- Occupational demands: Physical job requirements may slow return to full function
Empowering Your Recovery: Patient Self-Assessment & Psychosocial Support
A. Structured Patient Self-Assessment

Systematic symptom tracking provides valuable insights into your healing progress and helps identify patterns that might otherwise go unnoticed. A daily pain journal documenting pain levels, triggers, activities, and medications creates a comprehensive record that both you and your healthcare team can use to optimize treatment strategies.
Mobility assessments performed at home offer objective measures of functional improvement. Simple tests like forward bending distance, walking duration without pain, or ability to put on socks can be measured weekly to track progress. These functional markers often show improvement before pain scores change significantly.
Sleep quality monitoring reveals important healing indicators, as restorative sleep is essential for tissue repair and pain processing. Tracking sleep duration, quality ratings, and nighttime pain interruptions helps identify improvements that support overall recovery.
| Self-Assessment Tool | How to Use | Frequency | What It Reveals |
|---|---|---|---|
| Pain Scale Rating | Rate pain 0-10 daily at same time | Daily | Overall pain trend and trigger identification |
| Activity Log | Record daily activities and pain response | Daily | Functional capacity improvements |
| Sleep Journal | Track hours slept and quality rating | Daily | Recovery quality and pain impact on rest |
| Mobility Tests | Measure specific movements weekly | Weekly | Objective functional improvements |
B. Managing the Psychosocial Impact
The connection between mental health and physical healing becomes particularly important during herniated disc recovery. Chronic pain affects brain chemistry, stress hormone levels, and immune function, all of which influence healing speed and completeness. Addressing psychological aspects of recovery often accelerates physical improvements.
Stress management techniques like deep breathing, meditation, or progressive muscle relaxation can reduce cortisol levels that interfere with healing processes. These practices also help break the pain-stress-tension cycle that perpetuates symptoms and delays recovery.
Social support systems play crucial roles in maintaining motivation and adherence to treatment plans. Family members, friends, and support groups provide emotional encouragement during difficult periods and practical assistance with daily activities when needed.
Effective Coping Strategies:
- Mindfulness meditation: Reduces pain perception and stress response
- Cognitive behavioral techniques: Helps reframe negative thoughts about pain
- Gradual activity pacing: Prevents overexertion while maintaining progress
- Social engagement: Maintains relationships and prevents isolation
- Professional counseling: Addresses anxiety, depression, or trauma related to injury
- Relaxation techniques: Reduces muscle tension and improves sleep quality
When to Seek Immediate Medical Attention (Warning Signs/Red Flags)
Worsening Symptoms
Rapidly increasing pain intensity, especially when accompanied by new neurological symptoms, requires immediate medical evaluation. This pattern suggests possible complications like disc re-herniation, spinal infection, or other serious conditions that need prompt treatment to prevent permanent damage.
Progressive weakness in arms or legs, particularly if affecting both sides of the body, may indicate cauda equina syndrome or other serious spinal cord problems. These symptoms require emergency intervention to prevent permanent neurological damage.
New Neurological Deficits
Sudden loss of bladder or bowel control represents a medical emergency requiring immediate hospital evaluation. These symptoms suggest possible cauda equina syndrome, a rare but serious condition where multiple nerve roots at the base of the spinal cord become severely compressed.
Foot drop, where you cannot lift the front part of your foot, indicates significant nerve damage that may require surgical intervention. Similarly, sudden onset of severe weakness in specific muscle groups suggests acute nerve compression that needs immediate attention.
Critical Warning Signs Requiring Emergency Care
Cauda Equina Syndrome Indicators:
- Saddle anesthesia (numbness in groin, buttocks, or genitals)
- Bilateral leg weakness or numbness
- Loss of bladder or bowel control
- Severe, sudden onset back pain with neurological symptoms
- Progressive weakness in both legs
Other Emergency Situations:
- Fever with back pain (possible spinal infection)
- Severe headache with neck stiffness
- Sudden, severe pain after trauma or fall
- Progressive paralysis or profound weakness
- Signs of blood clot (swelling, warmth, redness in leg)
Long-Term Spinal Health & Prevention of Recurrence
Sustaining Recovery
Maintaining the gains achieved during initial healing requires ongoing commitment to spinal health practices. Recovery from herniated disc injury represents the beginning of a lifelong approach to spine care rather than a temporary treatment period. Developing sustainable habits prevents recurrence and optimizes long-term function.
Core strengthening exercises specifically targeting deep stabilizing muscles provide essential support for the spine during daily activities. These muscles, including the transversus abdominis, multifidus, and pelvic floor muscles, work together to maintain spinal stability and reduce stress on intervertebral discs.
Flexibility maintenance through regular stretching prevents muscle imbalances and joint stiffness that can predispose to future injuries. Hip flexor stretches, hamstring flexibility, and spinal mobility exercises should become part of your daily routine.
Ergonomics and Posture
Proper workplace ergonomics significantly reduces the risk of disc re-injury and supports long-term spinal health. Monitor positioning, chair height, keyboard placement, and lighting all contribute to maintaining neutral spinal curves during extended work periods. Regular position changes prevent static loading that can stress healing disc structures.
Home environment modifications include mattress selection, pillow positioning, and furniture arrangement that supports good posture. Sleep positions that maintain spinal alignment, particularly side-lying with pillow support, reduce nighttime stress on healing discs.
Regular Exercise and Core Strength
A comprehensive exercise program addressing strength, flexibility, and cardiovascular fitness provides the foundation for long-term spine health. Low-impact activities like walking, swimming, or cycling maintain fitness without excessive spinal loading. Gradually progressing intensity and duration prevents overuse injuries while building endurance.
Resistance training targeting core muscles, back extensors, and hip stabilizers creates a natural “muscular corset” that protects the spine during daily activities. Professional guidance from physical therapists or certified trainers ensures proper form and appropriate progression.
Lifestyle Adjustments
Weight management reduces mechanical stress on spinal structures, as excess body weight increases compressive forces on intervertebral discs. Even modest weight loss can significantly reduce symptoms and recurrence risk in overweight individuals.
Nutrition optimization supports tissue healing and reduces inflammation through anti-inflammatory foods and adequate protein intake. Hydration maintenance keeps disc tissues healthy, as these structures depend on proper fluid balance for shock absorption and nutrient transport.
Long-Term Success Strategies:
- Daily movement: Avoid prolonged sitting or static positions
- Weight management: Maintain healthy BMI to reduce spinal stress
- Stress reduction: Practice relaxation techniques regularly
- Sleep hygiene: Prioritize 7-9 hours of quality sleep nightly
- Regular check-ups: Monitor spinal health with healthcare providers
- Activity modification: Adapt activities to prevent re-injury
Conclusion – Signs a Herniated Disc Is Healing
Recap of Key Healing Signs
Recognizing the signs that your herniated disc is healing empowers you to track progress and maintain motivation throughout the recovery journey. The most reliable indicators include progressive pain reduction, improved mobility and function, restoration of neurological symptoms, and enhanced quality of life. These improvements often occur gradually and may fluctuate, but the overall trend should show consistent progress over weeks and months.
Objective medical assessments complement your subjective experience by providing measurable evidence of healing through physical examinations, imaging studies, and functional testing. These professional evaluations help distinguish between actual healing and temporary symptom relief, ensuring that your recovery is on track.
Patience and Persistence
Healing from herniated disc injury requires patience with the body’s natural recovery timeline and persistence in following treatment recommendations. The temptation to rush back to normal activities or abandon therapy during symptom improvements can lead to setbacks and prolonged recovery. Trusting the healing process while maintaining consistent self-care practices optimizes outcomes.
Understanding that recovery is rarely linear helps maintain realistic expectations and prevents discouragement during temporary setbacks. Each person’s healing journey is unique, influenced by multiple factors including age, overall health, injury severity, and treatment compliance.
Empowerment Through Knowledge
Knowledge about the healing process transforms you from a passive patient into an active participant in your recovery. Understanding what to expect, how to recognize progress, and when to seek help enables informed decision-making and better communication with your healthcare team. This partnership approach often leads to better outcomes and greater satisfaction with treatment results.
Regular monitoring of your progress through symptom tracking, functional assessments, and professional evaluations provides the feedback necessary to adjust treatment strategies and maintain motivation. Remember that working closely with qualified healthcare providers throughout your recovery journey ensures the safest and most effective path to lasting relief from herniated disc symptoms.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.

























