Root canal treatment represents one of modern dentistry’s most misunderstood procedures, saving millions of natural teeth annually while simultaneously generating widespread concern about potential health risks. This endodontic procedure involves removing infected or inflamed pulp tissue from inside a tooth’s root canals, disinfecting the chamber, and sealing it to prevent reinfection—a process that conventional dentistry considers both safe and highly effective.
Despite mainstream dental medicine’s endorsement of root canal therapy as a routine, pain-free procedure, persistent myths and conflicting information continue to circulate. Alternative approaches within biological dentistry raise serious questions about systemic health implications, challenging traditional orthodoxy with concerns about bacterial persistence, chronic inflammation, and potential links to autoimmune disorders.
“Are root canals bad for you? ” – This comprehensive analysis examines opposing viewpoints from traditional endodontics and holistic dental medicine, evaluating scientific evidence, addressing common misconceptions, and exploring the biological dentistry perspective on “silent” systemic effects. We’ll investigate when root canal treatment becomes necessary, debunk prevalent myths, analyze potential risks from both conventional and alternative perspectives, and provide guidance for making informed decisions about your oral and systemic health.
What Is Root Canal Treatment and Why Is It Necessary?
Root canal therapy becomes essential when dental decay penetrates the tooth’s innermost layer, reaching the pulpal tissue that contains nerves, blood vessels, and connective tissues. This endodontic intervention aims to eliminate infection while preserving the natural tooth structure, preventing extraction and maintaining proper dental function.
When Root Canal Treatment Becomes Unavoidable
Several clinical indicators necessitate endodontic intervention:
- Severe dental caries that has breached the pulp chamber
- Prolonged sensitivity to hot or cold temperatures lasting beyond normal stimuli removal
- Intense, throbbing pain particularly during nighttime hours
- Gingival swelling accompanied by tender, enlarged lymph nodes
- Periapical abscesses manifesting as “gum boils” near the affected tooth
- Dental trauma resulting in pulpal necrosis even without visible damage
- Asymptomatic pulpal death detectable only through radiographic examination and vitality testing
Importantly, pulpal necrosis can occur without obvious symptoms. Endodontists and general dentists employ specialized diagnostic techniques including electric pulp testing, thermal testing, and digital radiography to identify non-vital teeth requiring intervention.
The Root Canal Procedure: Step-by-Step Process
Modern endodontic treatment follows strict protocols ensuring optimal outcomes:
Initial Assessment and Anesthesia
- Comprehensive radiographic evaluation using digital imaging
- Administration of local anesthetic (typically lidocaine with epinephrine)
- Placement of rubber dam isolation for contamination control
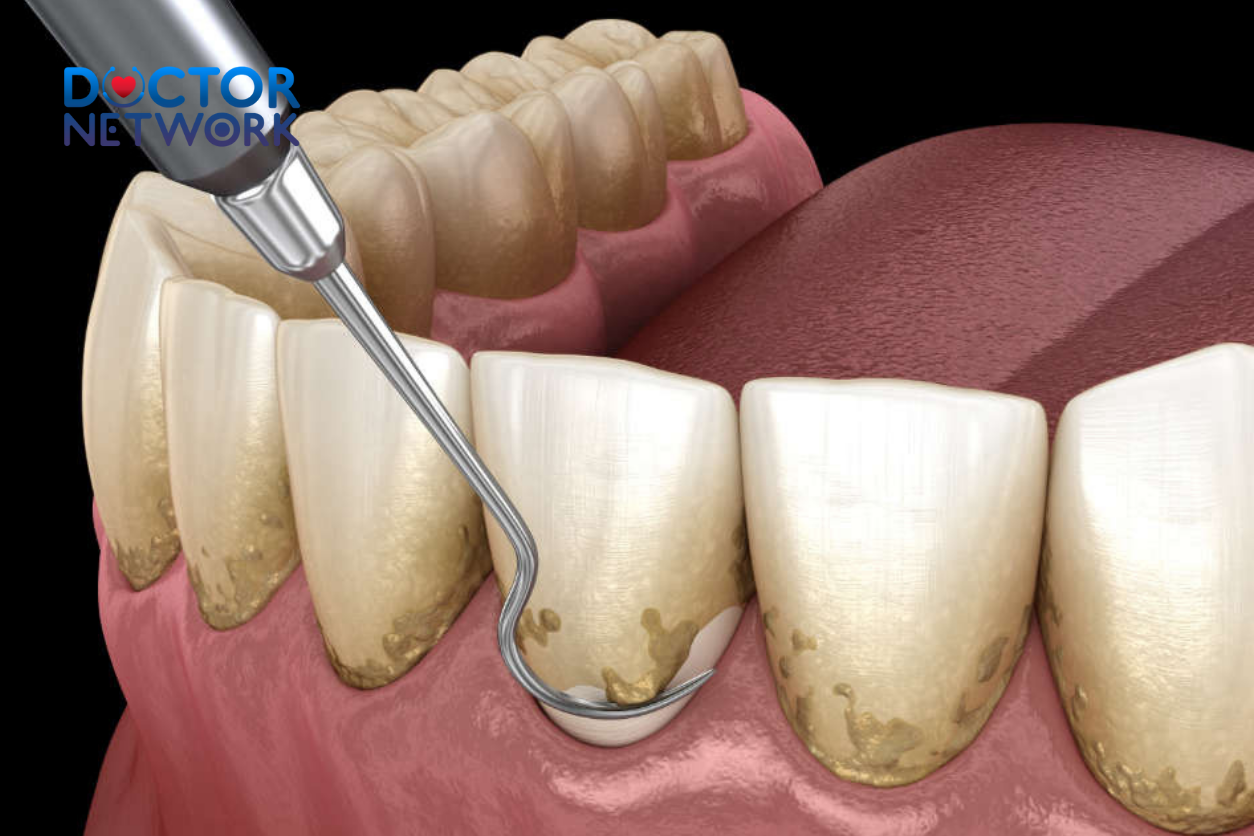
Access and Cleaning Phase
- Creation of access cavity through the tooth’s crown
- Location and negotiation of all root canal systems using specialized endodontic files
- Mechanical debridement of necrotic pulpal tissue and bacterial biofilms
- Chemical disinfection using sodium hypochlorite irrigation solutions
- Ultrasonic activation to enhance antimicrobial efficacy
Obturation and Restoration
- Complete drying of the canal system
- Three-dimensional filling using thermoplasticized gutta-percha and sealer
- Immediate temporary restoration or permanent composite filling
- Crown placement recommendation for structural reinforcement
Risks of Avoiding Root Canal Treatment
Untreated pulpal infections can lead to serious complications:
| Complication | Timeline | Severity Level |
|---|---|---|
| Acute periapical abscess | Days to weeks | Moderate to severe |
| Cellulitis and facial swelling | 1-2 weeks | Severe |
| Osteomyelitis | Weeks to months | Life-threatening |
| Ludwig’s angina | Rapid progression | Emergency |
| Septicemia | Variable | Critical |
Delayed treatment may result in tooth loss, alveolar bone destruction, and potentially life-threatening systemic infections. The financial cost of tooth replacement through dental implants, bridges, or partial dentures typically exceeds initial endodontic treatment expenses.
The Role of Endodontic Specialists
Board-certified endodontists complete additional specialized training beyond dental school, focusing exclusively on root canal therapy, retreatment procedures, and surgical endodontics. These specialists utilize advanced technology including:
- Dental operating microscopes for enhanced visualization
- Rotary instrumentation systems for efficient canal preparation
- Cone-beam computed tomography for three-dimensional diagnosis
- Ultrasonic devices for improved cleaning and disinfection
Endodontists demonstrate superior success rates compared to general dentists, particularly in complex cases involving calcified canals, retreatments, or unusual anatomical variations.

Debunking Common Root Canal Myths
Several persistent misconceptions about endodontic treatment continue to influence patient decisions despite contradicting modern scientific evidence.
Myth 1: Root Canal Treatment Is Extremely Painful
Reality: Contemporary root canal therapy produces minimal discomfort when performed with proper anesthetic technique. Advanced local anesthetic formulations, including articaine and prilocaine, provide profound pulpal anesthesia lasting several hours. Most patients report that the discomfort from anesthetic injection exceeds any sensation during the actual procedure.
Post-operative pain typically ranges from mild to moderate, easily managed with over-the-counter analgesics like ibuprofen or acetaminophen. Severe post-treatment pain occurs in fewer than 5% of cases and usually indicates incomplete disinfection or anatomical complications requiring additional treatment.
Myth 2: Root Canals Cause Systemic Disease
Reality: This misconception stems from flawed research conducted by Dr. Weston A. Price in the 1920s, which has been thoroughly debunked by modern medical science. Price’s experiments involved extracting teeth from patients with various medical conditions and implanting them under rabbit skin—a methodology that violates current research standards and bears no relevance to human physiology.
Extensive epidemiological studies have found no credible scientific evidence linking endodontic treatment to:
- Cardiovascular disease or heart attacks
- Arthritis or joint inflammation
- Cancer development or progression
- Autoimmune disorders or immunological dysfunction
- Alzheimer’s disease or cognitive decline
Conversely, a large-scale study published in JAMA Otolaryngology-Head & Neck Surgery demonstrated that patients with multiple endodontic treatments showed a 45% reduced cancer risk compared to controls, suggesting possible protective effects rather than harmful outcomes.
Myth 3: Tooth Extraction Is Always Superior and More Cost-Effective
Reality: Preserving natural tooth structure provides optimal function, aesthetics, and long-term oral health outcomes. Natural teeth possess proprioceptive feedback mechanisms through periodontal ligament receptors, allowing precise bite force modulation and enhanced chewing efficiency.
Tooth extraction consequences include:
- Adjacent tooth migration leading to malocclusion
- Alveolar bone resorption reducing facial height and support
- Opposing tooth super-eruption causing bite irregularities
- Temporomandibular joint dysfunction from altered occlusal relationships
Replacement options carry significant disadvantages:
| Replacement Type | Initial Cost | Maintenance | Longevity | Complications |
|---|---|---|---|---|
| Dental Implant | $3,000-5,000 | Low | 15-25 years | Implantitis, failure |
| Fixed Bridge | $2,500-4,500 | Moderate | 10-15 years | Abutment decay |
| Removable Partial | $1,500-3,000 | High | 5-10 years | Bone loss, instability |
| Root Canal + Crown | $2,000-3,500 | Low | 15-30 years | Minimal |
Myth 4: Root Canal Treatment Removes the Tooth Root
Reality: Endodontic therapy preserves the entire root structure while removing only the pulpal contents. The tooth root, including cementum, dentin, and periodontal ligament attachment, remains completely intact. This preservation maintains normal tooth mobility, proprioception, and integration with surrounding alveolar bone.
The procedure specifically targets:
- Pulpal tissue (nerves, blood vessels, connective tissue)
- Bacterial biofilms within the root canal system
- Necrotic debris and inflammatory byproducts
- Infected dentin in severe cases
Myth 5: Root Canal Success Is Temporary
Reality: Properly performed endodontic treatment achieves high long-term success rates. Clinical studies demonstrate:
- Initial success rates: 85-97% depending on case complexity
- 5-year survival: 93-98% for uncomplicated cases
- 10-year survival: 87-93% with appropriate restoration
- Lifetime retention: Many treated teeth function normally for decades
Success depends on several critical factors:
- Immediate placement of permanent restoration
- Crown coverage for posterior teeth
- Regular professional maintenance
- Patient compliance with oral hygiene protocols
However, endodontically treated teeth become more brittle due to moisture loss and structural changes following pulp removal. Cuspal coverage through crown placement significantly reduces fracture risk and enhances long-term prognosis.
The Biological Dentistry Perspective: Hidden Systemic Effects
Biological dentistry challenges conventional endodontic philosophy by questioning whether complete bacterial elimination is achievable and examining potential long-term systemic consequences of retaining treated teeth.
Origins of Biological Dental Concerns
Holistic dental practitioners argue that many health problems develop gradually over time, similar to environmental toxin exposure or processed food consumption effects. They contend this principle applies equally to endodontically treated teeth, where subtle, chronic bacterial presence may contribute to systemic inflammation and disease development.
This perspective emphasizes the interconnection between oral health and systemic wellness, viewing the mouth as a gateway to overall health rather than an isolated anatomical region. Biological dentists prioritize biocompatible materials, minimally invasive techniques, and consideration of each patient’s total toxic burden when making treatment recommendations.
Anatomical Challenges to Complete Disinfection
The complex internal architecture of teeth presents significant obstacles to complete bacterial elimination:
Microscopic Tubular Network Human dentin contains approximately 45,000 microscopic tubules per square millimeter, creating miles of interconnected channels within each tooth. These dentinal tubules provide ideal sanctuary for anaerobic bacteria, which can survive despite thorough mechanical and chemical disinfection attempts.
Accessory Canal Systems Beyond main root canals, teeth commonly contain:
- Lateral canals branching horizontally from main canals
- Apical deltas creating complex networks near root tips
- Isthmuses connecting parallel canals in multi-rooted teeth
- Fins and webs extending from main canal walls
Standard endodontic instrumentation addresses primary canals but may miss these auxiliary pathways, potentially leaving infected tissue and bacterial colonies undisturbed.
Biofilm Persistence Bacterial biofilms demonstrate remarkable resistance to antimicrobial agents, forming protective matrices that shield microorganisms from disinfecting solutions. Even after thorough irrigation with sodium hypochlorite and other endodontic medicaments, viable bacteria may persist within biofilm structures throughout the root canal system.
Theoretical Mechanisms of Systemic Impact
Biological dentistry proposes several pathways through which endodontically treated teeth might influence systemic health:
Chronic Low-Grade Infection Residual bacteria within treated teeth may continue metabolic activity, producing inflammatory mediators and toxic metabolites. These substances could theoretically leak through the apical foramen into periapical tissues and enter systemic circulation, contributing to chronic inflammatory burden.
Immune System Dysregulation Persistent antigenic stimulation from bacterial proteins and endotoxins might trigger chronic immune activation, potentially leading to:
- Autoimmune cross-reactivity
- Cytokine dysregulation
- Complement system activation
- Molecular mimicry phenomena
Meridian System Interference Some biological practitioners incorporate traditional Chinese medicine concepts, suggesting that infected teeth may disrupt acupuncture meridian flow, affecting organ systems connected through these energetic pathways.
Clinical Observations and Case Studies
Biological dentists report clinical improvements in various conditions following extraction of endodontically treated teeth:
Autoimmune Conditions
- Rheumatoid arthritis symptom reduction
- Multiple sclerosis progression slowing
- Chronic fatigue syndrome improvement
- Fibromyalgia pain decrease
Cardiovascular Health
- Blood pressure normalization
- Reduced inflammatory markers
- Improved circulation parameters
- Decreased cardiac arrhythmias
Neurological Symptoms
- Migraine frequency reduction
- Memory and cognitive enhancement
- Mood stability improvement
- Sleep quality restoration
Research and Documentation
Several researchers and clinicians have documented these observations:
Dr. Boyd Haley’s Toxicology Research Former University of Kentucky chemistry professor Dr. Boyd Haley investigated mercury toxicity and its interaction with other dental materials. His research suggested that certain combinations of dental materials, including those used in endodontic treatment, might produce toxic effects greater than individual components.
Dr. Josef Issels’ Cancer Research German oncologist Dr. Josef Issels reported that 98% of his cancer patients had infections in endodontically treated teeth. While this observation lacks controlled study validation, it has influenced biological dental thinking about potential cancer connections.
Historical Literature Several books and documentaries have popularized biological dental concerns:
- “Root Canal Cover-Up” by Dr. George Meinig (founding member of the American Association of Endodontists who later changed his position)
- “Death by Root Canal” by Dr. Ron Carlson
- “Let the Tooth Be Known” by Dr. Dawn Ewing
- Documentary films “Root Cause” and “Rooted”
These publications present anecdotal evidence and theoretical frameworks supporting biological dental perspectives, though they lack peer-reviewed scientific validation according to conventional medical standards.
Making Informed Decisions with Conflicting Information
The stark contrast between conventional endodontic medicine and biological dental philosophy creates genuine confusion for patients seeking optimal oral health care. Understanding how to navigate these opposing viewpoints requires careful consideration of evidence quality, risk-benefit analysis, and individual health priorities.
Addressing the Fundamental Disagreement
Conventional Position: Mainstream dentistry views biological concerns as unfounded fears based on outdated, debunked research. Professional organizations like the American Association of Endodontists maintain that decades of clinical experience and scientific research demonstrate root canal safety and efficacy.
Biological Position: Holistic practitioners argue that conventional research fails to account for long-term, subtle systemic effects that may take years or decades to manifest. They contend that absence of evidence is not evidence of absence, particularly for complex, multifactorial chronic diseases.
Framework for Patient Decision-Making
Seek Multiple Expert Opinions Consulting both conventional endodontists and biological dentists provides comprehensive perspective on available options. Each approach offers unique insights based on different philosophical frameworks and clinical experience.
Questions for conventional endodontists:
- What are the specific success rates for my case complexity?
- How do you ensure complete disinfection?
- What follow-up monitoring is recommended?
- When would you recommend extraction instead?
Questions for biological dentists:
- What specific tests assess systemic impact from treated teeth?
- How do you evaluate individual susceptibility to complications?
- What biocompatible replacement options are available?
- How do you support detoxification during treatment?
Comparative Risk-Benefit Analysis
| Treatment Approach | Potential Benefits | Potential Risks | Cost Considerations |
|---|---|---|---|
| Root Canal Treatment | Preserve natural tooth<br>Maintain proper occlusion<br>Cost-effective initially<br>High success rates<br>Minimal recovery time | Potential bacterial persistence<br>Possible systemic effects<br>Crown requirement<br>Retreatment possibility | $2,000-3,500 total<br>Insurance coverage typical |
| Extraction + Implant | Complete infection removal<br>Biocompatible materials<br>No bacterial concerns<br>Long-term stability | Surgical complications<br>Bone loss<br>Extended treatment time<br>Implant failure risk | $4,000-6,000 total<br>Limited insurance coverage |
| Extraction + Bridge | Infection elimination<br>Faster than implant<br>Good aesthetics<br>Established technique | Adjacent tooth preparation<br>Increased caries risk<br>Difficult hygiene maintenance<br>Limited lifespan | $3,000-5,000 total<br>Moderate insurance coverage |
Biological Assessment Considerations
Patients concerned about systemic effects might consider:
Comprehensive Health Evaluation
- Complete blood chemistry panels
- Inflammatory marker testing (CRP, ESR, cytokines)
- Immune function assessment
- Heavy metal analysis
- Oxidative stress markers
Energetic Testing Methods Some biological practitioners utilize:
- Electrodermal screening (EDS)
- Applied kinesiology
- Thermography
- Meridian stress assessment
Note: These testing methods lack scientific validation but may provide useful clinical information within biological dental frameworks.
Individual Risk Factors Consider personal susceptibility:
- Existing autoimmune conditions
- Chronic inflammatory diseases
- Multiple chemical sensitivities
- Previous dental infection complications
- Family history of systemic diseases
Alternative Treatment Approaches
Biocompatible Tooth Replacement Biological dentists prefer:
- Zirconia implants: Metal-free, ceramic construction
- Non-metal partial dentures: Flexible, biocompatible materials
- Maryland bridges: Conservative preparation requirements
- Traditional bridges: Using biocompatible materials
Conservative Management When possible, biological approaches emphasize:
- Ozone therapy: Antimicrobial treatment without chemicals
- Laser disinfection: Photodynamic therapy applications
- Herbal antimicrobials: Natural infection control methods
- Nutritional support: Immune system enhancement
Preventive Strategies Both approaches agree on prevention importance:
- Regular professional cleanings
- Optimal nutrition for immune function
- Stress management techniques
- Avoiding refined sugar consumption
- Proper oral hygiene protocols
5 common questions people often ask about “Are root canals bad for you?”
1. Are root canals bad for you?
Root canals are generally not bad for you. They are a safe and effective treatment to remove infected or damaged pulp inside a tooth, preventing the spread of infection and saving the natural tooth. Modern root canal treatments are similar to routine fillings and are designed to relieve pain and restore oral health.
2. Does a root canal procedure hurt?
Thanks to modern anesthesia, root canals are usually no more painful than getting a filling or tooth extraction. Patients may feel numb during the procedure and experience mild soreness or discomfort for a few days afterward, which can be managed with over-the-counter painkillers.
3. What are the risks or complications of root canals?
Possible risks include undetected cracks in the tooth root, missed canals or bacteria leading to reinfection, defective sealing materials, and inadequate filling. These complications are rare but can cause further infection or tooth failure, sometimes requiring additional treatment or tooth removal.
4. Can root canals cause systemic health problems?
Scientific studies, including those by the American Association of Endodontists, show no evidence that root canals cause chronic or systemic health issues. Concerns about root canals causing fatigue, joint pain, or other systemic effects are not supported by research.
5. How long is the recovery after a root canal?
Most patients can return to normal activities immediately after the procedure, although numbness lasts for a few hours. Mild pain or soreness may persist for a few days but usually resolves quickly. It is important to follow up with your dentist for permanent restoration like a crown to protect the tooth.
Conclusion: Navigating Root Canal Decisions
Root canal treatment represents a highly successful, scientifically validated procedure that has preserved millions of natural teeth and prevented countless serious infections according to conventional dental medicine. Modern endodontic techniques, advanced materials, and improved understanding of root canal anatomy have significantly enhanced treatment outcomes and patient comfort.
However, biological dentistry raises legitimate questions about long-term systemic health implications that conventional research may not adequately address. The complex anatomical structure of teeth, challenges in achieving complete bacterial elimination, and anecdotal reports of health improvements following extraction of treated teeth deserve thoughtful consideration.
The decision between root canal treatment and extraction ultimately depends on individual circumstances, health priorities, and risk tolerance. Patients with compromised immune systems, existing chronic inflammatory conditions, or strong concerns about systemic health effects might reasonably choose extraction despite higher initial costs and treatment complexity.
Conversely, individuals prioritizing tooth preservation, seeking cost-effective treatment, or comfortable with conventional dental approaches may find root canal therapy optimal for their needs. The key lies in thorough education, consultation with qualified practitioners from both perspectives, and careful consideration of personal health goals.
Final Recommendations:
- Gather comprehensive information from multiple professional sources
- Consider your overall health status and individual risk factors
- Evaluate financial implications of all treatment options
- Discuss follow-up monitoring regardless of chosen treatment
- Prioritize prevention through excellent oral hygiene and regular care
Informed decision-making empowers patients to choose treatments aligned with their values, health objectives, and personal circumstances. Whether pursuing conventional endodontic treatment or biological alternatives, maintaining open communication with trusted healthcare providers ensures optimal outcomes for both oral and systemic health.
References
1. The American Association of Endodontists (AAE) – The Leading Authority
The AAE is the primary resource for scientific information on endodontic (root canal) treatment. They have extensively addressed and debunked the myths surrounding root canal safety.
Evidence: Position Statement & Myth vs. Fact Sheets.
Content Summary: The AAE explains that the focal infection theory is outdated and was based on flawed research methods from the 1920s (e.g., poor sanitation, no control groups, inducing massive doses of bacteria in animals). They emphasize that there is no valid scientific evidence linking root canal-treated teeth to systemic diseases. In fact, treating an infected tooth removes a source of inflammation that could potentially harm the body.
Source: American Association of Endodontists (AAE)
Author: The organization itself.
Link:
Root Canal Safety Page: https://www.aae.org/patients/root-canal-treatment/myths-about-root-canals/root-canal-safety/
Myths About Root Canals: https://www.aae.org/patients/root-canal-treatment/myths-about-root-canals/
2. Large-Scale Epidemiological Studies on Root Canals and Cancer Risk
Opponents of root canals often claim they can cause cancer. Large, modern, case-control studies have investigated this claim and found no evidence to support it. In fact, some studies have found the opposite.
Study Title: “Dental Caries and Head and Neck Cancers”
Content Summary: This study, published in a reputable medical journal, investigated the association between dental health and head and neck cancers. It found that patients with a history of multiple root canal treatments had a 45% reduced risk of developing these cancers. The authors suggest that root canal treatment reduces the total burden of oral inflammation, which is a known risk factor for cancer.
Author(s): Tezal, M., et al.
Source: JAMA Otolaryngology–Head & Neck Surgery (2013)
Link: https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/1681273
3. Studies on Root Canals and Systemic Health (e.g., Heart Disease)
Another common claim is that root canals cause heart disease. Again, scientific research does not support this.
Study Title: “Endodontic Treatment and Risk of Coronary Artery Disease”
Content Summary: This large-scale study followed over 87,000 patients and found no significant association between having a root canal and an increased risk of coronary artery disease. It directly contradicts the focal infection theory’s claims about bacteria from treated teeth causing heart problems.
Author(s): Caplan, D.J., et al.
Source: Journal of Dental Research (2009)
Link: https://journals.sagepub.com/doi/abs/10.1177/0022034509343355
4. The Success Rate and Longevity of Root Canal Treatment
Modern endodontics has a very high success rate, allowing patients to keep their natural teeth for a lifetime.
Study Title: “Outcome of Primary Root Canal Treatment: Systematic Review of the Literature — Part 1. A Meta-analysis of the Survival of Root Canal Treated Teeth”
Content Summary: This comprehensive meta-analysis reviewed numerous studies and found that the survival rate of teeth after root canal treatment is very high, ranging from 86% to 98% over periods of 2 to 10 years. This demonstrates the procedure’s effectiveness in preserving the natural dentition.
Author(s): Ng, Y.L., et al.
Source: International Endodontic Journal (2007)
Link: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2591.2007.01322.x
Part 2: The Origin of the Controversy (The “Root Canals are Bad” Argument)
The claims that root canals are harmful are almost exclusively based on the “Focal Infection Theory” from the early 20th century. It’s crucial to understand the historical context and why this research is no longer considered valid.
1. Dr. Weston A. Price and the Focal Infection Theory
Origin: In the 1920s, Dr. Weston A. Price, a dentist, conducted a series of experiments. He claimed that bacteria trapped in root canal-treated teeth could “leak” and cause systemic diseases elsewhere in the body, such as heart and kidney disease. He reported transferring diseases from humans to rabbits by implanting fragments of root canal-treated teeth.
Why it is debunked:
Lack of Proper Scientific Controls: Price’s research lacked many standards of modern science. He did not use control groups, his experiments were conducted in non-sterile environments, and the doses of bacteria introduced to the animals were massive and unnatural.
Inability to be Replicated: Other researchers have been unable to replicate his findings using modern, sterile techniques.
Outdated Understanding of Microbiology: We now understand that bacteria are everywhere in the human body (the microbiome) and that the presence of bacteria does not automatically equal disease. The key is controlling infection and inflammation. Modern root canal procedures are designed to do exactly that by thoroughly cleaning, disinfecting, and sealing the root canal system.
Source of the Theory: “Dental Infections, Oral and Systemic” (Book)
Author: Weston A. Price (published in 1923)
Link: While the book is historically significant, it’s not a valid scientific source by today’s standards. It is often cited by holistic health websites that oppose root canals. A critical review of Price’s work is available from the AAE link provided in Part 1.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.