Does a bone density test show cancer? No, a bone density test (DEXA/DXA scan) cannot directly diagnose bone cancer. This specialized imaging procedure measures bone mineral density and strength to detect osteoporosis, not malignancies. While DEXA scans may occasionally reveal abnormalities that warrant further investigation, they are not designed as cancer screening tools and lack the diagnostic precision required for oncological assessment.
This comprehensive guide will examine the relationship between bone density testing and cancer detection, explore what DEXA scans actually measure, discuss proper cancer diagnostic procedures, and explain when bone density testing becomes relevant in cancer care. We’ll also cover result interpretation, treatment options for low bone density, and important patient considerations to help you make informed healthcare decisions.
Understanding Bone Density Testing (DEXA/DXA Scan)
DEXA (dual-energy X-ray absorptiometry) scans measure bone mineral content and skeletal strength using low-dose X-ray radiation. This non-invasive diagnostic tool represents the gold standard for osteoporosis screening and fracture risk assessment in clinical practice.
Definition and Primary Purpose
The DEXA scanner employs dual-energy X-ray beams to quantify calcium and other bone minerals within specific skeletal segments. Healthcare providers primarily utilize this technology to:
- Diagnose osteoporosis – a systemic skeletal disorder characterized by compromised bone strength and increased fracture susceptibility
- Detect osteopenia – preliminary bone loss that precedes osteoporosis development
- Assess fracture risk – calculate probability of future bone breaks based on current density measurements
- Monitor treatment effectiveness – track therapeutic responses in patients receiving osteoporosis medications
How DEXA Technology Works
The dual-energy X-ray system differentiates between bone tissue and soft tissue by utilizing two distinct radiation energy levels. Bone appears as bright white regions on the resulting images, while soft tissues create darker shadows. This contrast allows precise measurement of bone mineral density (BMD) at specific anatomical sites.
Key technical features include:
- Low radiation exposure (less than a chest X-ray)
- High precision and reproducibility
- Standardized measurement protocols
- Computer-assisted analysis and reporting
Common Examination Sites
DEXA scans typically focus on weight-bearing bones most susceptible to osteoporotic fractures:
| Primary Sites | Clinical Significance | Fracture Risk Prediction |
|---|---|---|
| Lumbar spine (L1-L4) | Central skeletal assessment | High correlation with vertebral fractures |
| Hip (femoral neck, total hip) | Weight-bearing joint evaluation | Strong predictor of hip fractures |
| Forearm (radius) | Peripheral bone assessment | Useful when spine/hip cannot be measured |
Peripheral devices may scan finger bones, wrist, or heel, but these locations provide less accurate fracture risk predictions compared to central measurements.
Procedure Timeline and Patient Experience
DEXA scanning typically requires 10-30 minutes depending on the number of skeletal sites examined. The procedure involves:
- Patient positioning – lying supine on a padded examination table
- Mechanical arm movement – scanner passes over target areas
- Minimal patient cooperation – remaining still during image acquisition
- No contrast agents – unlike other imaging modalities
- Immediate ambulation – patients can resume normal activities immediately
Terminology Evolution
Healthcare terminology has evolved from “DEXA scan” to “DXA scan” in recent years, though both terms remain clinically acceptable. This linguistic shift reflects standardization efforts within the medical imaging community, yet many practitioners and patients continue using both designations interchangeably.

Can DEXA Scans Detect Cancer?
DEXA scans are not designed to diagnose bone cancer and should never be used as primary cancer screening tools. These specialized bone density measurements focus exclusively on mineral content and skeletal strength rather than tumor detection or malignancy assessment.
Why DEXA Cannot Diagnose Cancer
The fundamental limitation lies in DEXA technology’s specific imaging capabilities. While bone density scans may occasionally reveal abnormalities suggesting further investigation, several factors prevent reliable cancer detection:
- Limited image resolution – DEXA cannot visualize tumor morphology or cellular characteristics
- Density-focused measurements – the technology measures mineral content, not tissue composition
- Lack of soft tissue detail – surrounding muscle, ligaments, and other structures appear poorly defined
- No contrast enhancement – unlike cancer-specific imaging that highlights abnormal blood flow
DEXA’s Role in Cancer Care Context
When patients undergo cancer treatment, oncologists may recommend DEXA scanning to monitor bone health rather than detect malignancies. Certain cancer therapies can significantly impact skeletal integrity:
Chemotherapy effects on bone density:
- Aromatase inhibitors for breast cancer reduce estrogen levels, accelerating bone loss in women
- Androgen deprivation therapy for prostate cancer decreases testosterone, weakening male skeletal structure
- Corticosteroids used in various cancer protocols directly inhibit bone formation
- Radiation therapy to skeletal areas can damage bone-producing cells (osteoblasts)
Post-Treatment Bone Health Monitoring
Cancer survivors often require long-term bone density surveillance because:
- Treatment-induced osteoporosis develops gradually over months to years
- Fracture risk increases substantially in cancer patients compared to healthy individuals
- Early intervention with bone-protecting medications can prevent serious complications
- Baseline measurements establish reference points for future comparisons
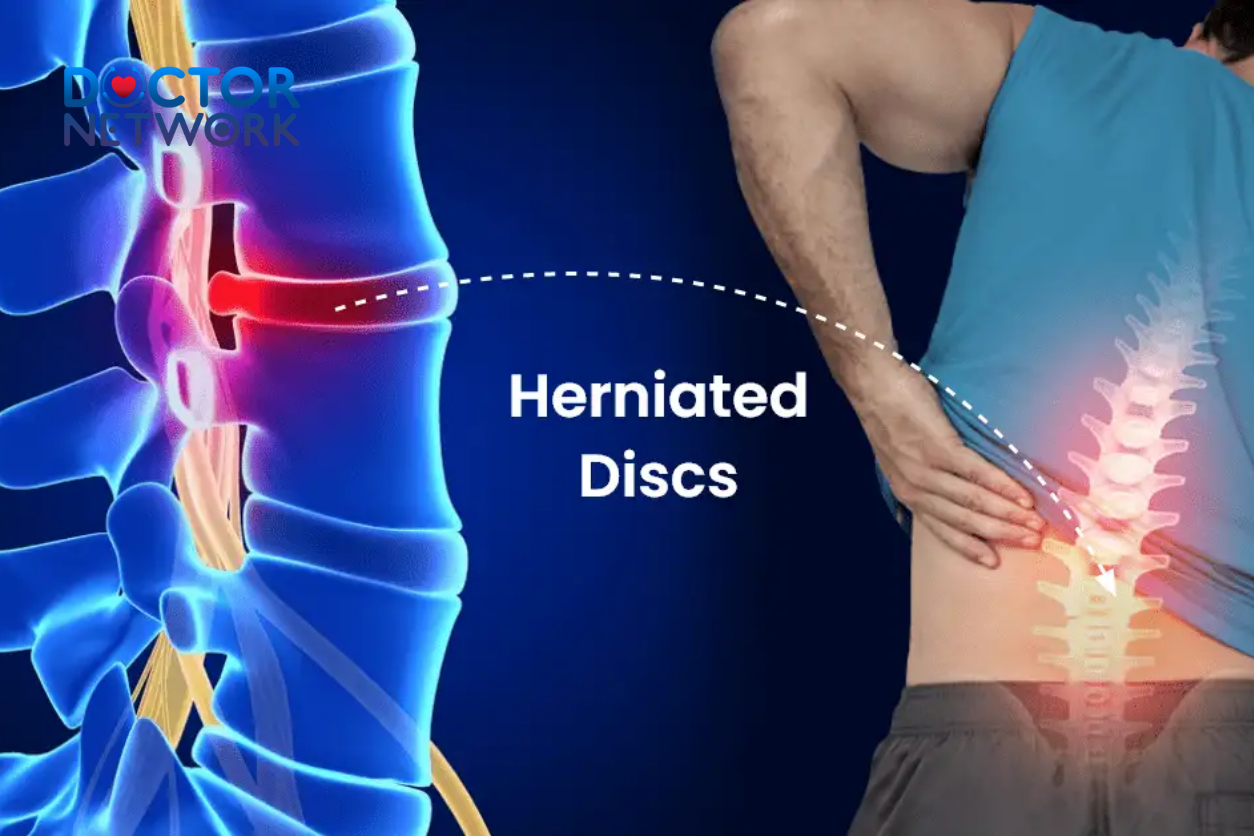
Understanding Bone Cancer
Primary bone cancer (bone sarcoma) originates from skeletal cells, while secondary bone cancer represents metastatic spread from other body regions. This distinction carries significant implications for diagnosis, treatment, and prognosis.
Primary vs. Secondary Bone Cancer
Primary bone cancers develop directly from bone, cartilage, or connective tissue cells. Common types include:
- Osteosarcoma – most frequent primary bone tumor in children and adolescents
- Ewing sarcoma – aggressive tumor affecting long bones and pelvis
- Chondrosarcoma – cartilage-based malignancy more common in adults
Secondary (metastatic) bone cancer occurs when malignant cells spread from primary tumors in other organs. Cancers that commonly metastasize to bone include:
- Breast cancer
- Prostate cancer
- Lung cancer
- Kidney cancer
- Thyroid cancer
Epidemiology and Age Distribution
Bone cancer remains relatively rare, accounting for less than 1% of all malignancies. However, age distribution patterns vary significantly:
- Children and adolescents (ages 10-20) experience higher primary bone cancer rates
- Adults over 40 more commonly develop secondary bone cancers
- Peak incidence for osteosarcoma occurs during teenage growth spurts
- Gender differences exist, with slight male predominance in certain tumor types
Clinical Symptoms and Warning Signs
Persistent bone pain that worsens over time represents the most common initial symptom of bone cancer. Additional warning signs include:
Progressive symptoms:
- Deep, aching bone pain (especially at night)
- Swelling or tenderness near affected bones
- Joint stiffness and reduced range of motion
- Unexplained limping or gait changes
Systemic manifestations:
- Unexplained fatigue and weakness
- Fever without obvious infection
- Unintentional weight loss
- Pathological fractures through weakened bone
Less common presentations:
- Palpable mass near bone surface
- Neurological symptoms if spine involvement
- Breathing difficulties with rib cage tumors
Diagnostic Tests for Bone Cancer
Bone cancer diagnosis requires multiple complementary imaging studies and tissue sampling procedures. No single test can definitively confirm malignancy; instead, oncologists combine various diagnostic modalities to establish accurate diagnoses and staging.
X-Ray Imaging
Plain radiographs serve as the initial imaging study for suspected bone cancer, revealing structural abnormalities and destructive bone changes. X-rays demonstrate:
- Osteolytic lesions – areas where cancer has destroyed normal bone tissue
- Osteoblastic changes – regions of abnormal bone formation in response to tumor
- Cortical disruption – breaks in the outer bone shell
- Soft tissue masses – visible swelling around affected bones
Limitations of X-ray diagnosis:
- Early-stage tumors may not appear on radiographs
- Small lesions can escape detection
- Soft tissue involvement poorly visualized
- Cannot differentiate between benign and malignant lesions
Bone Scan (Skeletal Scintigraphy)
Bone scans differ fundamentally from DEXA scans by using radioactive tracers to identify areas of abnormal bone metabolism. This nuclear medicine procedure involves:
- Radiotracer injection – small amounts of technetium-99m methylene diphosphonate (MDP)
- Uptake period – 2-3 hours for tracer distribution throughout skeleton
- Whole-body imaging – gamma camera detects radioactive emissions
- Hot spot identification – areas of increased tracer uptake suggest abnormal activity
Bone scan interpretation:
- Hot spots appear as dark, intense areas indicating increased bone turnover
- Cold spots may represent areas of decreased blood flow or bone destruction
- Symmetric uptake typically suggests benign conditions
- Asymmetric patterns raise suspicion for malignancy
Computed Tomography (CT) Scan
CT imaging provides detailed cross-sectional views of bone structure and surrounding soft tissues. Advanced CT technology offers several diagnostic advantages:
Technical capabilities:
- High-resolution bone detail – superior to conventional X-rays
- Soft tissue visualization – identifies tumor extension beyond bone
- 3D reconstruction – comprehensive tumor mapping for surgical planning
- Contrast enhancement – highlights areas of increased blood flow
CT findings in bone cancer:
- Bone destruction patterns (lytic, sclerotic, or mixed)
- Cortical breakthrough and soft tissue extension
- Calcification patterns within tumors
- Relationship to adjacent structures
Magnetic Resonance Imaging (MRI)
MRI represents the gold standard for bone tumor evaluation, providing unparalleled soft tissue contrast and tumor characterization. This imaging modality excels in:
Superior diagnostic features:
- Multiplanar imaging – axial, sagittal, and coronal views
- Excellent soft tissue contrast – differentiates tumor from normal tissue
- Bone marrow evaluation – detects early tumor infiltration
- Vascular assessment – identifies tumor blood supply
MRI advantages over other imaging:
- No ionizing radiation exposure
- Superior soft tissue detail
- Excellent for surgical planning
- Can differentiate between benign and malignant lesions
| Imaging Modality | Primary Advantage | Bone Cancer Detection | Radiation Exposure |
|---|---|---|---|
| X-ray | Initial screening | Moderate | Low |
| Bone Scan | Whole-body assessment | High sensitivity | Moderate |
| CT Scan | Bone detail | High specificity | Moderate-High |
| MRI | Soft tissue contrast | Excellent characterization | None |
| DEXA | Bone density only | Not applicable | Very low |
Bone Biopsy Procedures
Tissue sampling through bone biopsy provides definitive cancer diagnosis and tumor classification. Two primary biopsy approaches exist:
Needle biopsy (percutaneous):
- Core needle technique – obtains tissue samples through skin
- Image guidance – CT or MRI-directed for precise targeting
- Outpatient procedure – typically performed under local anesthesia
- Minimal invasiveness – small incision and rapid recovery
Surgical biopsy (open):
- Incisional biopsy – removes tissue sample through surgical incision
- Excisional biopsy – removes entire lesion when technically feasible
- General anesthesia – required for most procedures
- Larger tissue samples – provides more material for comprehensive analysis
Blood Tests and Tumor Markers
Laboratory studies can support bone cancer diagnosis but cannot provide definitive confirmation. Relevant blood tests include:
Bone metabolism markers:
- Alkaline phosphatase – elevated in bone-forming tumors
- Lactate dehydrogenase (LDH) – increased in rapidly growing tumors
- Osteocalcin – reflects bone formation activity
- C-telopeptide – indicates bone breakdown
Additional laboratory considerations:
- Complete blood count may show anemia or elevated white cell count
- Erythrocyte sedimentation rate (ESR) often increases with malignancy
- Calcium levels may be elevated in bone-destructive tumors
- Protein electrophoresis helps exclude multiple myeloma
Interpreting Bone Density Test Results
DEXA scan results utilize standardized scoring systems comparing individual measurements to reference populations. Understanding these scores helps patients and healthcare providers assess fracture risk and treatment needs.
T-Score Interpretation
The T-score compares your bone density to that of a healthy 30-year-old adult of the same gender. This comparison uses the peak bone mass typically achieved in early adulthood as the reference standard.
T-score categories and clinical significance:
| T-Score Range | Bone Density Classification | Clinical Interpretation | Fracture Risk |
|---|---|---|---|
| -1.0 and above | Normal bone density | Optimal bone health | Low risk |
| -1.0 to -2.5 | Osteopenia (low bone density) | Below normal, increased concern | Moderate risk |
| -2.5 and below | Osteoporosis | Significantly compromised bone strength | High risk |
| -2.5 with fracture | Severe osteoporosis | Advanced disease with complications | Very high risk |
Each unit decrease in T-score represents:
- Approximately 10-12% reduction in bone density
- Roughly 2-fold increase in fracture risk
- One standard deviation from the young adult mean
Z-Score Significance
Z-scores compare your bone density to age-matched peers of the same gender, weight, and ethnicity. This comparison helps identify whether bone loss exceeds normal aging expectations.
Z-score interpretation guidelines:
- Above -2.0 – bone density within expected range for age
- Below -2.0 – bone density significantly lower than age-matched peers
- Requires investigation – abnormally low Z-scores suggest underlying medical conditions
Conditions associated with low Z-scores:
- Hormonal disorders (hyperparathyroidism, hyperthyroidism)
- Malabsorption syndromes (celiac disease, inflammatory bowel disease)
- Chronic kidney or liver disease
- Certain medications (corticosteroids, anticonvulsants)
- Nutritional deficiencies (vitamin D, calcium)
- Malignancy – including bone cancers or metastatic disease
When Additional Testing Becomes Necessary
Significantly abnormal Z-scores may warrant comprehensive medical evaluation to identify underlying causes. Healthcare providers typically investigate when:
- Z-score falls below -2.0 in premenopausal women or men under 50
- Unexplained bone loss occurs despite adequate treatment
- Fractures occur with minimal trauma
- Multiple risk factors suggest secondary osteoporosis
Potential follow-up investigations:
- Comprehensive metabolic panel
- Vitamin D and parathyroid hormone levels
- Thyroid function tests
- Inflammatory markers
- Cancer screening – if clinically indicated by symptoms or risk factors
Managing Low Bone Density
Patients with osteopenia or osteoporosis require comprehensive treatment strategies combining lifestyle modifications, nutritional interventions, and targeted medications. Early intervention can significantly reduce fracture risk and maintain skeletal health.
Exercise and Physical Activity
Weight-bearing exercise stimulates bone formation and improves overall skeletal strength. Effective exercise programs should include:
Weight-bearing activities:
- Walking, jogging, or running
- Dancing and aerobic exercise
- Stair climbing
- Tennis and racquet sports
Resistance training benefits:
- Increases muscle strength and bone density
- Improves balance and coordination
- Reduces fall risk
- Enhances overall physical function
Balance and flexibility exercises:
- Tai chi and yoga
- Proprioceptive training
- Core strengthening
- Fall prevention programs
Nutritional Interventions
Adequate calcium and vitamin D intake forms the foundation of bone health management. Recommended daily allowances vary by age and gender:
Calcium requirements:
- Adults 19-50 years: 1,000 mg daily
- Women over 50: 1,200 mg daily
- Men over 70: 1,200 mg daily
Vitamin D recommendations:
- Adults 19-70 years: 600 IU daily
- Adults over 70: 800 IU daily
- Higher doses may be needed for deficiency correction
Food sources rich in bone-building nutrients:
- Calcium – dairy products, leafy greens, sardines, almonds
- Vitamin D – fatty fish, fortified milk, egg yolks
- Magnesium – nuts, seeds, whole grains
- Vitamin K – dark leafy vegetables, broccoli
Pharmacological Treatments
Multiple medication classes effectively treat osteoporosis by reducing bone loss or promoting bone formation. Treatment selection depends on individual patient factors:
Bisphosphonates (first-line therapy):
- Alendronate (Fosamax)
- Risedronate (Actonel)
- Ibandronate (Boniva)
- Zoledronic acid (Reclast)
Alternative medications:
- Denosumab (Prolia) – monoclonal antibody reducing bone resorption
- Teriparatide (Forteo) – parathyroid hormone analog stimulating bone formation
- Raloxifene (Evista) – selective estrogen receptor modulator
- Hormone replacement therapy – for postmenopausal women with specific indications
Monitoring Treatment Effectiveness
Regular DEXA scanning helps assess treatment response and guide therapeutic decisions. Monitoring schedules typically involve:
- Baseline scan – before treatment initiation
- Follow-up scanning – every 1-2 years during treatment
- Medication holidays – considered after 3-5 years of bisphosphonate therapy
- Treatment adjustments – based on bone density changes and fracture risk
DEXA Scan Limitations and Considerations
While DEXA scanning provides valuable bone health information, several limitations affect result accuracy and clinical interpretation. Understanding these constraints helps patients and providers make informed decisions.
Radiation Exposure Concerns
DEXA scans expose patients to minimal radiation, typically less than a chest X-ray. However, certain precautions apply:
- Pregnancy considerations – pregnant women should avoid unnecessary radiation exposure
- Risk-benefit analysis – diagnostic benefits generally outweigh minimal radiation risks
- Cumulative exposure – multiple scans over time represent negligible cumulative risk
- Alternative timing – non-urgent scans can be postponed until after pregnancy
Technical Limitations and Accuracy Issues
Several factors can affect DEXA scan accuracy and result interpretation:
Equipment variations:
- Different manufacturers may produce varying results
- Calibration differences between machines
- Software updates can affect measurements
- Cross-calibration protocols help minimize variations
Patient factors affecting accuracy:
- Spinal abnormalities – arthritis, previous surgery, scoliosis
- Body habitus – very thin or obese patients may have less accurate results
- Positioning variations – slight changes can affect measurements
- Movement artifacts – patient motion during scanning
Previous Medical Procedures
Recent medical interventions can interfere with DEXA scan accuracy:
Contrast agents:
- Barium studies within 7-10 days
- Intravenous contrast for CT scans
- Nuclear medicine procedures using radioactive tracers
Recommended preparation:
- Avoid calcium supplements 24 hours before scanning
- Remove metal objects (jewelry, belts, buttons)
- Wear comfortable, loose-fitting clothing
- Inform technologist of recent procedures
Insurance Coverage Limitations
Health insurance coverage for DEXA scanning varies significantly among providers and plans:
Medicare coverage criteria:
- Women over 65 years
- Men over 70 years
- Younger patients with specific risk factors
- Monitoring intervals typically every 2 years
Private insurance considerations:
- Coverage policies vary by carrier
- Prior authorization may be required
- Out-of-pocket costs vary significantly
- Appeal processes available for denied claims
Patient Experience and Practical Considerations
DEXA scanning provides a straightforward, painless diagnostic experience for most patients. Understanding the process helps reduce anxiety and ensures optimal results.
Pre-Scan Preparation
Minimal preparation requirements make DEXA scanning convenient for most patients:
Dietary considerations:
- Discontinue calcium supplements 24 hours prior
- No fasting requirements
- Regular medications can continue
- Adequate hydration recommended
Clothing recommendations:
- Loose, comfortable garments without metal
- Avoid clothing with zippers, buttons, or underwire bras
- Athletic wear often ideal
- Hospital gowns available if needed
During the Examination
The scanning process involves minimal patient discomfort and cooperation:
Positioning requirements:
- Lying flat on padded examination table
- Proper positioning for optimal image quality
- Remaining still during image acquisition (typically 10-30 seconds per site)
- Technologist guidance throughout procedure
Communication with staff:
- Questions encouraged before and during procedure
- Explanation of each step
- Immediate feedback about image quality
- Scheduling follow-up appointments if needed
Results and Follow-Up
Most patients receive DEXA results within 1-2 weeks through various communication methods:
Result delivery options:
- Telephone consultation with healthcare provider
- Written reports mailed to patient
- Electronic health portal access
- In-person appointment for complex cases
Managing anxiety during waiting period:
- Understanding that DEXA measures bone density, not cancer
- Discussing concerns with healthcare team
- Connecting with support groups if appropriate
- Maintaining normal activities while awaiting results
Special Considerations for Children
Pediatric DEXA scanning requires additional preparation and consideration:
Age-appropriate explanations:
- Simple, non-frightening descriptions of the procedure
- Demonstration with dolls or models
- Parent or caregiver presence during scanning
- Distraction techniques (music, videos) if available
Technical modifications:
- Specialized pediatric reference databases
- Age-appropriate positioning techniques
- Shorter scanning protocols when possible
- Sedation rarely necessary
5 frequently asked questions about “Does a bone density test show cancer?”
1. Does a bone density test detect cancer directly?
No, a bone density test (such as a DEXA scan) is not designed to diagnose cancer. It measures bone mineral density to assess bone health but cannot visualize tumors or cancerous lesions directly.
2. Can a bone density test suggest the presence of cancer indirectly?
Yes, sometimes a sudden or localized drop in bone density may raise suspicion of bone metastasis or other cancer-related bone abnormalities, prompting further diagnostic tests. However, these findings are not definitive for cancer and require additional imaging or biopsy.
3. What imaging tests are better for detecting bone cancer or metastasis?
X-rays, CT scans, MRI, and bone scans are more effective than bone density tests for detecting bone cancers or metastatic lesions. A biopsy may also be necessary to confirm cancer diagnosis.
4. Can cancer treatments affect bone density test results?
Yes, treatments like chemotherapy, hormone therapy, or medications such as bisphosphonates can impact bone density. Bone density tests help monitor bone health during and after cancer treatment to manage risks of osteoporosis or fractures.
5. Does a normal bone density test rule out bone cancer?
No, a normal bone density test does not exclude cancer. Early-stage bone cancer or small metastases may not affect bone density enough to be detected. Persistent symptoms require further evaluation regardless of bone density results.
Conclusion
DEXA scans serve as essential tools for bone health assessment but cannot diagnose bone cancer. These specialized imaging studies excel at measuring bone mineral density and predicting fracture risk, while cancer detection requires different diagnostic approaches including CT scans, MRI, bone scans, and tissue biopsy procedures.
Understanding the distinct roles of various imaging modalities helps patients make informed healthcare decisions. DEXA scanning provides valuable information about osteoporosis and fracture risk, particularly important for cancer survivors whose treatments may compromise bone health. However, patients experiencing persistent bone pain, unexplained fractures, or other concerning symptoms should discuss appropriate cancer screening options with their healthcare providers.
The comprehensive evaluation of bone health requires consideration of multiple factors including age, gender, medical history, medications, and risk factors. By combining DEXA results with clinical assessment and appropriate additional testing when indicated, healthcare providers can develop personalized treatment plans to optimize skeletal health and prevent complications.
Regular consultation with qualified healthcare professionals ensures appropriate use of bone density testing and timely referral for specialized cancer evaluation when clinically warranted. This collaborative approach maximizes the benefits of available diagnostic technologies while addressing patient concerns and maintaining optimal bone health throughout life.
References
1. DXA is for Osteoporosis, Not Cancer Detection
Các nghiên cứu và bài viết tổng quan luôn nhấn mạnh vai trò của DXA trong việc đánh giá loãng xương, không phải phát hiện ung thư.
Title: The Role of DXA in the Assessment of Bone Health
Author(s): John T. Schousboe, Leslie R. Harms.
Source: Current Osteoporosis Reports, 2021.
Link: https://link.springer.com/article/10.1007/s11914-021-00693-4
Key Findings: This review article provides a comprehensive overview of DXA technology. It details its application in diagnosing osteoporosis, predicting fracture risk, and monitoring response to therapy. The article does not mention cancer detection as a primary or secondary use, reinforcing that its design and sensitivity are tailored for measuring overall mineral density, not identifying focal malignant lesions.
2. The Impact of Cancer Treatments on Bone Health (Where DXA becomes relevant)
Đây là lĩnh vực mà DXA được sử dụng rộng rãi nhất trong ung thư học – để quản lý các tác dụng phụ của việc điều trị.
A. Breast Cancer Treatment (Aromatase Inhibitors)
Title: Recommendations for Bone Health in Patients With Breast Cancer
Author(s): Catherine Van Poznak, et al. (ASCO – American Society of Clinical Oncology)
Source: Journal of Clinical Oncology, 2022.
Key Findings: This is a major clinical practice guideline. It states that Aromatase Inhibitors (AIs), a common hormone therapy for postmenopausal women with hormone-receptor-positive breast cancer, are known to cause significant bone loss and increase fracture risk. The guideline explicitly recommends a baseline DXA scan for all women starting AI therapy to assess their bone health. Follow-up DXA scans are recommended every 1-2 years to monitor for treatment-induced bone loss.
Conclusion: This shows DXA is a standard of care in the context of breast cancer, but its purpose is to manage a side effect of treatment (bone loss), not to detect the cancer itself.
B. Prostate Cancer Treatment (Androgen Deprivation Therapy)
Title: Bone Health in Men With Prostate Cancer
Author(s): V.S. Gralow, et al. (A comprehensive review paper summarizing multiple studies)
Source: ESMO Open: Cancer Horizons, 2018.
Link: https://www.esmoopen.com/article/S2059-7029(18)30048-X/fulltext
Key Findings: Androgen Deprivation Therapy (ADT) is a cornerstone of treatment for advanced prostate cancer. This therapy drastically lowers testosterone, which is crucial for maintaining bone mass in men. The paper highlights that ADT leads to a rapid decrease in BMD and a significantly increased risk of fractures. It emphasizes the importance of baseline and serial DXA scans to monitor bone density in these patients and to guide interventions like calcium/vitamin D supplementation or bone-strengthening drugs (e.g., bisphosphonates).
3. Cancer Metastases to Bone and Appropriate Imaging
Các nghiên cứu so sánh cho thấy DXA không phải là công cụ phù hợp để tìm kiếm di căn xương.
Title: Imaging of Bone Metastases: An Update
Author(s): Frédéric E. Lecouvet
Source: Cancer Imaging, 2019.
Key Findings: This review article details the best imaging techniques for detecting bone metastases. The primary tools discussed are:
Nuclear Bone Scintigraphy (Bone Scan): Very sensitive for detecting areas of high bone turnover caused by metastases.
PET/CT (Positron Emission Tomography/Computed Tomography): Highly sensitive for detecting metabolically active cancer cells throughout the body, including in bone.
MRI (Magnetic Resonance Imaging): Excellent for evaluating bone marrow and soft tissue involvement, especially in the spine.
The article does not list DXA as a modality for detecting metastases because it measures average density over a large area (like the entire hip or a lumbar vertebra) and lacks the sensitivity to detect small, focal lesions typical of early metastases.
4. Multiple Myeloma and Bone Disease
Multiple Myeloma là một loại ung thư máu ảnh hưởng trực tiếp đến tủy xương và gây ra tổn thương xương lan tỏa.
Title: The Role of Dual-energy X-ray Absorptiometry in the Diagnosis of Osteoporosis in Multiple Myeloma
Author(s): Abildgaard, N., et al.
Source: Haematologica, 2000.
Key Findings: This study investigated the use of DXA in patients with multiple myeloma. It found that DXA is effective at quantifying the degree of bone loss (osteoporosis) caused by the disease. However, the diagnosis of multiple myeloma itself relies on other criteria (blood tests, bone marrow biopsy, and imaging that shows lytic lesions). Therefore, a DXA scan might show very low bone density, prompting a doctor to investigate further for underlying causes, which could include multiple myeloma, but the scan itself is not the diagnostic tool for the cancer.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.