Fecal-smelling breath, medically termed severe halitosis, affects millions worldwide and signals underlying oral or systemic health issues requiring immediate attention. This malodorous condition stems from volatile sulfur compounds (VSCs) like hydrogen sulfide and methyl mercaptan produced by anaerobic bacteria colonizing the oral cavity, creating embarrassing social situations and potential health complications.
Why Does My Breath Smell Like Poop? This comprehensive guide examines the multifaceted causes of putrid breath odor, from poor oral hygiene and periodontal disease to systemic conditions like diabetes and xerostomia. We’ll explore evidence-based treatment protocols, professional diagnostic methods, and preventive strategies that restore oral freshness while addressing underlying pathology. Understanding these mechanisms empowers patients to seek appropriate intervention and maintain optimal oral health.
Understanding Foul-Smelling Breath: The Medical Perspective

Severe halitosis manifesting as feces-like odor represents a complex interplay between bacterial metabolism, oral environment, and systemic health factors. The condition significantly impacts psychological well-being, causing social anxiety, communication avoidance, and reduced quality of life. Beyond embarrassment, persistent malodor indicates active oral pathology that threatens dental integrity and overall health.
The psychological ramifications extend beyond mere self-consciousness. Chronic bad breath triggers anxiety disorders, depression, and social isolation as individuals withdraw from intimate conversations and professional interactions. This behavioral adaptation creates a cycle where reduced social engagement further impacts mental health and self-esteem.
From an oral health perspective, foul breath signals bacterial overgrowth that weakens tooth enamel, inflames gingival tissues, and increases tooth loss risk. The pathogenic microorganisms responsible for odor production simultaneously release toxins that destroy periodontal ligaments and alveolar bone, compromising the structural foundation supporting teeth.
Detailed Causes of Fecal-Smelling Breath
Oral Hygiene Deficiencies and Bacterial Accumulation
Inadequate plaque removal serves as the primary catalyst for malodorous breath, creating anaerobic environments where sulfur-producing bacteria thrive. Food debris trapped in interdental spaces and gingival sulci provides substrate for bacterial fermentation, generating offensive compounds that characterize fecal-like breath odor.
The mechanism involves specific bacterial species, particularly Porphyromonas gingivalis, Prevotella intermedia, and Fusobacterium nucleatum, which metabolize protein remnants into volatile sulfur compounds. These anaerobic pathogens flourish in oxygen-depleted environments created by poor oral hygiene, producing hydrogen sulfide, methyl mercaptan, and dimethyl sulfide—the primary molecules responsible for putrid odors.
Lingual surfaces harbor the highest concentration of odor-producing bacteria, with the posterior tongue’s papillae creating ideal retention sites for debris and microorganisms. The dorsal tongue’s rough topography traps proteins from desquamated epithelial cells, food particles, and bacterial biofilms, necessitating dedicated tongue cleaning protocols.
| Bacterial Species | Primary Metabolic Product | Odor Characteristic | Clinical Significance |
|---|---|---|---|
| Porphyromonas gingivalis | Hydrogen sulfide | Rotten egg smell | Periodontal disease marker |
| Prevotella intermedia | Methyl mercaptan | Fecal-like odor | Aggressive periodontitis |
| Fusobacterium nucleatum | Dimethyl sulfide | Cabbage-like smell | Necrotizing ulcerative gingivitis |
| Treponema denticola | Indole compounds | Sweet, fecal odor | Advanced periodontal destruction |
Dietary Contributors to Malodorous Breath
Specific foods create temporary but intense breath malodor through direct absorption into bloodstream circulation and pulmonary excretion. Allium vegetables (onions, garlic), cruciferous vegetables, spiced foods, and fermented beverages contain sulfur compounds that persist hours after consumption, exacerbating existing halitosis conditions.
Beyond immediate effects, dietary patterns influence oral pH and bacterial composition. High-sugar diets, particularly sucrose and fructose consumption before sleep, create acidic environments favoring pathogenic bacterial growth. These conditions promote enamel demineralization while providing substrate for volatile sulfur compound production.
Beneficial foods counteract malodorous breath through various mechanisms:
- Fibrous fruits and vegetables: Stimulate saliva production and mechanically cleanse oral surfaces
- Probiotic foods: Introduce beneficial bacteria that compete with pathogenic species
- Polyphenol-rich foods: Exhibit antimicrobial properties against odor-producing bacteria
- High-water content foods: Maintain oral hydration and dilute bacterial concentrations
Lifestyle Factors and Behavioral Influences
Tobacco use creates multifaceted breath problems through direct chemical deposition, xerostomia induction, and periodontal tissue damage. Nicotine and tar compounds adhere to oral tissues while reducing saliva production, creating ideal conditions for bacterial proliferation and volatile compound accumulation.
Alcohol consumption similarly compromises oral health through dehydration and bacterial growth promotion. Ethanol metabolism produces acetaldehyde, contributing to offensive breath odor while simultaneously reducing saliva’s natural cleansing action. Chronic alcohol use exacerbates periodontal disease and increases oral cancer risk.
Mouth breathing, whether due to nasal obstruction or habitual patterns, significantly impacts oral moisture levels. The constant airflow desiccates oral tissues, reducing saliva’s protective effects and concentrating bacterial metabolites. This condition particularly affects sleep-time oral health when saliva production naturally decreases.
Medication-Induced Xerostomia
Numerous pharmaceutical agents cause dry mouth as an adverse effect, indirectly contributing to halitosis through reduced saliva production. Saliva serves multiple protective functions: mechanical cleansing, pH buffering, antimicrobial activity, and volatile compound dilution.
Common medication classes causing xerostomia:
- Antihistamines (diphenhydramine, loratadine)
- Tricyclic antidepressants (amitriptyline, nortriptyline)
- Diuretics (hydrochlorothiazide, furosemide)
- Anticholinergics (atropine, scopolamine)
- Antihypertensives (ACE inhibitors, beta-blockers)
- Anticonvulsants (phenytoin, carbamazepine)
Oral Pathological Conditions
Periodontal disease represents the most significant oral cause of fecal-smelling breath, creating deep pockets where anaerobic bacteria flourish undisturbed. Periodontitis involves progressive destruction of periodontal ligaments and alveolar bone, creating spaces for bacterial colonization and toxic metabolite accumulation.
Dental caries provide additional bacterial reservoirs through cavitated tooth structure. The necrotic pulp tissue within infected teeth releases particularly offensive odors as bacterial enzymes break down organic matter. Root canal infections similarly produce putrid smells from decomposing neural and vascular tissues.
Dental abscesses create pus-filled cavities containing concentrated bacterial populations and inflammatory exudate. These infections release volatile compounds directly into the oral cavity while creating systemic inflammatory responses that can affect overall health status.
| Condition | Primary Symptoms | Odor Characteristics | Treatment Priority |
|---|---|---|---|
| Chronic Periodontitis | Bleeding gums, pocket formation | Persistent fecal-like smell | High – prevents tooth loss |
| Periapical Abscess | Severe pain, facial swelling | Intense putrid odor | Urgent – systemic infection risk |
| Necrotizing Gingivitis | Ulcerated gums, fever | Metallic, fecal smell | Urgent – tissue necrosis |
| Advanced Caries | Tooth sensitivity, visible cavities | Sweet, putrid odor | Moderate – prevents progression |
Systemic Disease Manifestations
Diabetes mellitus creates oral complications through multiple pathways affecting breath quality. Hyperglycemia alters saliva composition, reduces immune function, and promotes bacterial growth. Diabetic ketoacidosis produces acetone breath, while poor glycemic control increases periodontal disease severity and associated malodor.
Sjögren’s syndrome, an autoimmune condition affecting salivary and lacrimal glands, causes severe xerostomia leading to bacterial overgrowth and intense halitosis. The reduced saliva production eliminates natural oral cleansing mechanisms, allowing pathogenic bacteria to establish persistent colonies.
Respiratory tract infections, including chronic sinusitis, post-nasal drip, and bronchial infections, contribute to breath malodor through bacterial colonization of upper respiratory tissues. These conditions create additional sources of volatile compounds that mix with oral breath during exhalation.
Gastrointestinal disorders, particularly gastroesophageal reflux disease (GERD), introduce stomach acid and partially digested food particles into the oral cavity. The acidic environment promotes bacterial growth while providing substrate for volatile compound production. Helicobacter pylori infections may also contribute to systemic halitosis through metabolic byproduct circulation.
Recognition of Warning Signs: When to Seek Professional Help

Persistent halitosis lasting beyond 24-48 hours despite improved oral hygiene indicates underlying pathology requiring professional evaluation. The severity and character of breath odor provide diagnostic clues about potential causes and appropriate treatment approaches.
Associated symptoms warrant immediate dental consultation:
- Taste alterations: Metallic, bitter, or persistent bad taste
- Oral pain: Tooth sensitivity, gum tenderness, or jaw discomfort
- Bleeding gums: Spontaneous or induced gingival hemorrhage
- Tooth mobility: Loosening or shifting of dental structures
- Gum recession: Exposure of root surfaces and increased tooth length
- Oral lesions: Ulcers, white patches, or suspicious tissue changes
Communication difficulties arising from breath concerns significantly impact quality of life and professional relationships. When patients avoid close interpersonal contact or experience anxiety about speaking, the condition requires comprehensive evaluation addressing both medical and psychological aspects.
Underlying health concerns manifest through breath changes, making halitosis a potential diagnostic indicator for systemic diseases. Fruity breath suggests diabetic ketoacidosis, while ammonia-like odors indicate kidney dysfunction. These presentations require coordinated medical and dental care.
Comprehensive Treatment and Prevention Strategies

Advanced Oral Hygiene Protocols
Effective halitosis management begins with mechanical plaque removal using evidence-based techniques that disrupt bacterial biofilms and eliminate substrate for volatile compound production. Proper brushing technique involves gentle circular motions applied for minimum two-minute durations, ensuring complete coverage of all tooth surfaces and gingival margins.
Fluoride toothpaste selection should prioritize antimicrobial ingredients like stannous fluoride or triclosan that provide additional bacterial control beyond caries prevention. Electric toothbrushes demonstrate superior plaque removal compared to manual brushing, particularly benefiting patients with limited dexterity or motivation challenges.
Interdental cleaning represents the most critical component of halitosis prevention, addressing bacterial accumulation in spaces inaccessible to toothbrush bristles. Daily flossing removes food debris and disrupts bacterial biofilms between teeth, while water flossers provide gentler alternatives for patients with sensitive gums or orthodontic appliances.
Tongue cleaning protocol:
- Use dedicated tongue scrapers rather than toothbrush bristles
- Apply gentle pressure from posterior to anterior tongue surfaces
- Perform 5-7 strokes covering entire dorsal tongue area
- Rinse scraper between passes to remove accumulated debris
- Complete tongue cleaning before brushing to prevent bacterial redistribution
Therapeutic mouthwashes containing antimicrobial agents like cetylpyridinium chloride or chlorhexidine provide adjunctive bacterial control. However, alcohol-containing formulations may exacerbate xerostomia, requiring careful product selection based on individual patient needs.
Evidence-Based Home Remedies
Traditional remedies offer scientifically-supported alternatives for halitosis management when combined with proper oral hygiene. Saltwater rinses create hypertonic environments that reduce bacterial populations while promoting tissue healing through osmotic effects and pH neutralization.
Fresh ginger contains 6-gingerol compounds demonstrating antimicrobial activity against oral pathogens while stimulating saliva production. The mechanical action of chewing fresh ginger releases active compounds directly into the oral cavity, providing immediate odor neutralization and sustained bacterial inhibition.
Lemon juice provides ascorbic acid and citric acid that exhibit broad-spectrum antimicrobial effects against bacteria, fungi, and viruses. The acidic pH temporarily reduces bacterial populations, while vitamin C supports immune function and tissue repair. However, frequent acid exposure may contribute to enamel erosion, requiring moderation in use.
Apple cider vinegar’s acetic acid content creates unfavorable environments for pathogenic bacteria while promoting beneficial microbial balance. Diluted vinegar rinses (1 tablespoon per cup of water) provide antimicrobial benefits without excessive acid exposure to dental structures.
Comparative effectiveness of home remedies:
| Remedy | Active Compounds | Mechanism | Duration of Effect | Evidence Level |
|---|---|---|---|---|
| Saltwater rinse | Sodium chloride | Osmotic bacterial reduction | 2-4 hours | Strong clinical evidence |
| Fresh ginger | 6-gingerol, zingiberene | Antimicrobial, saliva stimulation | 3-6 hours | Moderate research support |
| Lemon juice | Ascorbic acid, citric acid | pH reduction, antimicrobial | 1-3 hours | Limited clinical trials |
| Apple cider vinegar | Acetic acid | Bacterial inhibition | 2-5 hours | Preliminary evidence |
| Mint leaves | Menthol, essential oils | Antimicrobial, aromatic masking | 1-2 hours | Traditional use, limited studies |
Professional Dental Interventions
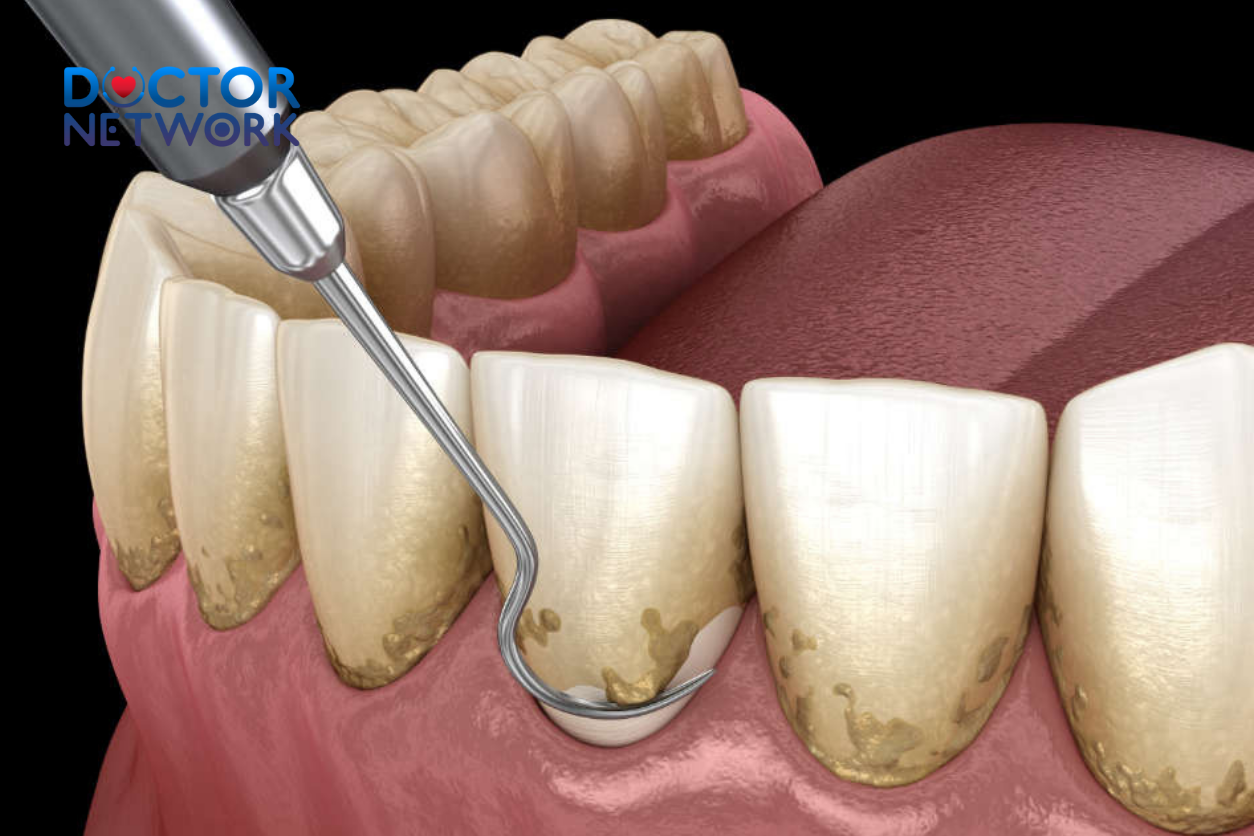
Regular dental prophylaxis every six months removes calcified deposits (calculus) that harbor bacterial biofilms resistant to home care efforts. Professional scaling instruments access subgingival areas where pathogenic bacteria concentrate, eliminating primary sources of volatile sulfur compound production.
Root planing procedures smooth root surfaces to prevent bacterial reattachment while promoting gingival reattachment and pocket depth reduction. This therapy specifically targets periodontal pathogens responsible for severe halitosis, addressing the underlying disease process rather than merely masking symptoms.
Restorative treatments eliminate bacterial reservoirs within cavitated teeth through complete caries removal and placement of biocompatible filling materials. Endodontic therapy addresses infected pulp tissues that contribute significantly to breath malodor, while maintaining tooth structure and function.
Specialized diagnostic methods:
- Halimeter testing: Quantifies volatile sulfur compound concentrations for objective assessment
- Oral pH monitoring: Identifies acidic conditions promoting bacterial growth
- Bacterial culture analysis: Determines specific pathogenic species requiring targeted therapy
- Salivary flow assessment: Evaluates xerostomia severity and treatment needs
Periodontal surgical interventions may be necessary for advanced disease cases where non-surgical therapy proves insufficient. Procedures like guided tissue regeneration and bone grafting restore periodontal architecture while eliminating deep bacterial reservoirs contributing to persistent halitosis.
Lifestyle Modifications for Long-Term Success
Adequate hydration maintains optimal saliva production and dilutes bacterial concentrations throughout the day. Water consumption should target 8-10 glasses daily, with increased intake during periods of physical activity, illness, or medication use affecting saliva production.
Dietary modifications emphasize foods that naturally cleanse the oral cavity and inhibit bacterial growth. Crunchy fruits and vegetables provide mechanical cleaning action while stimulating saliva flow. Probiotic foods introduce beneficial bacteria that compete with pathogenic species for oral colonization sites.
Foods promoting oral health:
- Apples: Polyphenols with antimicrobial properties
- Celery: High water content and fibrous texture for mechanical cleansing
- Yogurt: Probiotics that improve oral microbial balance
- Green tea: Catechins with anti-inflammatory and antimicrobial effects
- Parsley: Chlorophyll compounds that neutralize sulfur compounds
Smoking cessation eliminates direct chemical contributions to breath malodor while improving periodontal health and immune function. Professional cessation programs provide behavioral support and pharmacological aids to overcome nicotine dependence and restore oral health.
Managing Chronic and Unexplained Halitosis
Persistent halitosis despite comprehensive oral care requires multidisciplinary evaluation involving dental, medical, and potentially psychological specialists. Otolaryngologists assess upper respiratory tract contributions, while gastroenterologists evaluate digestive system factors affecting breath quality.
Collaboration between healthcare providers ensures comprehensive evaluation of systemic diseases that manifest through oral symptoms. Endocrinologists manage diabetes-related complications, while rheumatologists address autoimmune conditions affecting salivary function.
Special population considerations:
- Elderly patients: Higher medication use and reduced saliva production require modified approaches
- Denture wearers: Prosthetic cleaning protocols and tissue health maintenance
- Pediatric patients: Age-appropriate techniques and parental education for habit establishment
- Immunocompromised individuals: Enhanced infection control and specialized therapeutic protocols
Conclusion
Fecal-smelling breath represents a treatable condition with identifiable causes and effective interventions when approached systematically. Understanding the complex interplay between oral hygiene, systemic health, and bacterial metabolism empowers patients to take proactive steps toward resolution while recognizing when professional intervention becomes necessary.
The multifaceted nature of severe halitosis requires comprehensive evaluation addressing oral pathology, systemic diseases, and lifestyle factors simultaneously. Success depends on patient commitment to consistent oral care combined with professional guidance tailored to individual circumstances and underlying causes.
Early intervention prevents progression from simple halitosis to complex oral health problems requiring extensive treatment. Regular dental examinations, proper home care techniques, and attention to systemic health factors provide the foundation for long-term breath freshness and optimal oral health.
For persistent symptoms or concerning associated signs, consultation with qualified dental professionals ensures appropriate diagnosis and treatment planning. Comprehensive oral health contributes significantly to overall well-being, self-confidence, and quality of life, making investment in proper care both medically and personally rewarding.
5 COMMON QUESTIONS
1. Why does my breath smell like poop?
Bad breath that smells like feces is usually caused by the presence of sulfur-containing compounds produced by bacteria in the mouth or digestive system. Common causes include poor oral hygiene, gum disease, infections, or digestive issues such as constipation or bowel obstruction, which can cause odor to be released through the mouth.
2. Can digestive problems cause poop-like breath odor?
Yes, digestive problems such as constipation, gastroesophageal reflux disease (GERD), or small intestinal bacterial overgrowth (SIBO) can cause foul-smelling breath. When stool remains in the intestines too long or digestive processes are impaired, gases and toxins can enter the bloodstream or stomach, leading to bad breath that smells like feces.
3. Could poor oral hygiene be the reason for poop-smelling breath?
Absolutely. Inadequate brushing and flossing allow bacteria to accumulate on the tongue, teeth, and gums, producing foul-smelling sulfur compounds. Food particles trapped in the mouth can rot and cause a bad odor similar to feces. Regular dental care and tongue cleaning are essential to prevent this.
4. When should I see a doctor about bad breath that smells like poop?
You should see a healthcare professional if:
The bad breath persists despite good oral hygiene.
You have other symptoms like abdominal pain, constipation, diarrhea, or unexplained weight loss.
You notice a sudden change in breath odor.
You have signs of infection or gum disease.
A doctor or dentist can help diagnose underlying causes and recommend appropriate treatment.
5. How can I get rid of breath that smells like poop?
To improve breath odor:
Maintain excellent oral hygiene: brush teeth twice daily, floss, and clean your tongue.
Stay hydrated and avoid tobacco products.
Address digestive issues by eating a balanced diet, managing constipation, and consulting a doctor if needed.
Use mouthwash with antibacterial properties.
Regular dental check-ups and professional cleanings.
If the problem persists, medical evaluation is necessary to rule out infections or gastrointestinal conditions.
REFERENCES
1. Gastrointestinal (GI) Issues
This is the most common category of causes for a fecal breath odor.
A. Bowel Obstruction
Mechanism: A physical blockage in the small or large intestine prevents the normal passage of stool. This leads to a backup of fecal matter, fluids, and gas. The trapped material undergoes prolonged bacterial fermentation, producing large amounts of foul-smelling compounds. These compounds can be absorbed through the intestinal wall into the bloodstream and are then exhaled via the lungs. In severe cases, it can lead to vomiting of fecal matter (feculent vomiting or copremesis).
Evidence and Sources:
Source: Merck Manual Professional Version (a widely respected medical textbook).
Author/Editor: Parswa Ansari, MD.
Topic: The clinical overview of “Intestinal Obstruction” explicitly lists vomiting that may become feculent as a key symptom, especially in distal small-bowel or large-bowel obstruction. This directly links the smell of feces to the condition.
Source: Cleveland Clinic
Topic: Patient-facing information on Bowel Obstruction. They describe the symptoms, including “foul-smelling breath,” as a result of the backup of food and stool in the intestines.
B. Severe Constipation and Fecal Impaction
Mechanism: Similar to a bowel obstruction but less acute. When stool remains in the colon for an extended period, it becomes a breeding ground for bacteria that produce odorous gases. These gases, including indole and skatole, can be absorbed into the circulation and exhaled.
Evidence and Sources:
Source: A research review in the Journal of Natural Science, Biology and Medicine.
Author(s): Kapoor, U., Sharma, G., Juneja, M., & Nagpal, A.
Study/Topic: “Halitosis: Current concepts on etiology, diagnosis and management.” This review discusses extra-oral causes of halitosis, mentioning that gastrointestinal diseases, including stasis (like severe constipation), can lead to bad breath as byproducts of digestion are absorbed into the blood and released in the lungs.
Link: JNSBM – Halitosis Review
C. Gastrocolic Fistula
Mechanism: This is a rare but very serious condition where an abnormal channel (fistula) forms between the stomach and the colon. This allows fecal matter from the colon to enter the stomach directly. The contents can then be regurgitated or the odors can travel up the esophagus, causing breath that smells strongly of feces.
Evidence and Sources:
Source: Case report in the BMJ Case Reports journal.
Author(s): Al-Haddad, M., et al.
Study/Topic: “Gastrocolic fistula: a rare complication of a forgotten disease.” Case reports like this one document patients presenting with symptoms such as fecal vomiting (copremesis) and foul-smelling eructation (belching), which directly confirms the connection.
Link (Example Case Report): BMJ Case Reports – Gastrocolic Fistula
D. Small Intestinal Bacterial Overgrowth (SIBO)
Mechanism: SIBO is a condition where excessive bacteria are present in the small intestine. These bacteria ferment carbohydrates that are not properly absorbed, producing gases like hydrogen, methane, and hydrogen sulfide. While not always fecal, the type and volume of gas can produce a very foul, sulfurous, or stool-like odor on the breath.
Evidence and Sources:
Source: A review article in the World Journal of Gastroenterology.
Author(s): Ghoshal, U. C., & Shukla, R.
Study/Topic: “Small intestinal bacterial overgrowth and irritable bowel syndrome: a bridge between functional organic divide.” This study discusses the pathophysiology of SIBO, including the production of gases by bacterial fermentation, which are measured by breath tests for diagnosis. These are the same gases that can cause halitosis.
Link: WJG – SIBO Review
2. Systemic Diseases
Sometimes, the cause is not in the GI tract itself but is a result of a whole-body disease where the body cannot properly filter toxins from the blood.
A. Liver Failure (Fetor Hepaticus)
Mechanism: In severe liver disease (cirrhosis or liver failure), the liver cannot detoxify the blood effectively. Substances like mercaptans (which are also found in flatus and feces) and dimethyl sulfide build up in the bloodstream, travel to the lungs, and are exhaled. The resulting breath odor is called fetor hepaticus, often described as a musty, sweet, and slightly fecal smell.
Evidence and Sources:
Source: A scientific study in the Journal of Chromatography B.
Author(s): Van den Velde, S., Nevens, F., Van Hee, K., van Steenberghe, D., & Quirynen, M.
Study/Topic: “The chemical and clinical basis of fetor hepaticus.” This research specifically identifies the volatile organic compounds (VOCs) responsible for the distinct smell, including dimethyl sulfide, confirming the link between liver failure and specific odorous compounds.
Link: PubMed – The chemical and clinical basis of fetor hepaticus
B. Kidney Failure (Uremic Fetor)
Mechanism: When the kidneys fail, they can no longer filter waste products like urea from the blood. The urea is converted into ammonia in the saliva and exhaled, causing a fishy or ammonia-like smell known as uremic fetor. While typically not described as “fecal,” a very severe or complex case could be perceived as such by some individuals.
Evidence and Sources:
Source: National Kidney Foundation
Topic: Educational materials on Chronic Kidney Disease (CKD) symptoms describe “ammonia breath” or a metallic taste in the mouth as common signs of uremia (build-up of wastes in the blood).
3. Oral and Nasal Issues (Less Common for Fecal Smell)
While less likely to cause a distinctly “fecal” smell, severe infections in the oral or nasal cavities can produce extremely foul odors.
Mechanism: Deep pockets from severe periodontal (gum) disease, large tonsil stones (tonsilloliths), or a chronic sinus infection can harbor anaerobic bacteria. These bacteria break down proteins in trapped food debris, mucus, and dead cells, releasing potent volatile sulfur compounds that can be overwhelmingly strong.
Evidence and Sources:
Source: American Dental Association (ADA)
Topic: Patient information on “Bad Breath (Halitosis)”. The ADA explains that most persistent bad breath is due to oral sources, primarily the bacteria on the tongue and in gum pockets.
Link: ADA – Bad Breath
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.