Stage 4 chronic kidney disease represents a critical juncture where kidney function deteriorates severely, with estimated glomerular filtration rate (eGFR) dropping to 15-29 mL/min/1.73m². At this advanced stage, patients face complex complications requiring aggressive treatment strategies to maintain quality of life and extend survival. Life expectancy varies significantly based on age at diagnosis, overall health status, treatment adherence, and access to specialized nephrology care.
Stage 4 Kidney Failure Life Expectancy – This comprehensive guide examines the symptoms and complications of stage 4 CKD, factors influencing prognosis, effective management strategies, and multifaceted perspectives on living with advanced kidney disease. We will explore current research developments, emerging therapies, and ethical considerations in end-stage renal care, providing essential information for patients, families, and caregivers navigating this challenging journey.

Defining Chronic Kidney Disease (CKD)
Chronic kidney disease constitutes a progressive, irreversible condition characterized by sustained kidney damage that impairs the organs’ filtration capacity over months or years. The kidneys gradually lose their ability to remove waste products, excess fluid, and toxins from the bloodstream, leading to accumulation of harmful substances throughout the body.
CKD Progression Through Five Stages
CKD advances through five distinct stages based on kidney function measurements:
| Stage | eGFR (mL/min/1.73m²) | Description | Kidney Function |
|---|---|---|---|
| 1 | ≥90 | Normal or high function with kidney damage | 90-100% |
| 2 | 60-89 | Mild decrease in function | 60-89% |
| 3a | 45-59 | Mild to moderate decrease | 45-59% |
| 3b | 30-44 | Moderate to severe decrease | 30-44% |
| 4 | 15-29 | Severe decrease in function | 15-29% |
| 5 | <15 | Kidney failure (ESRD) | <15% |
Characteristics of Stage 4 CKD
Stage 4 CKD represents the penultimate phase before end-stage renal disease (ESRD), characterized by severe kidney impairment requiring immediate intervention. The kidneys retain only 15-29% of normal function, triggering systemic complications affecting cardiovascular health, bone metabolism, and blood chemistry. Early diagnosis and aggressive treatment at this stage remain crucial for preventing further deterioration and optimizing patient outcomes.
The significance of prompt intervention cannot be overstated, as stage 4 CKD patients face imminent progression to dialysis or transplantation within months to years. Healthcare providers emphasize comprehensive care coordination involving nephrologists, dietitians, social workers, and other specialists to address the multifaceted challenges patients encounter.
Symptoms and Complications of Stage 4 CKD
Common Symptoms Experienced
Stage 4 CKD manifests through increasingly severe symptoms that significantly impact daily functioning and quality of life. Patients typically experience profound fatigue and weakness due to uremic toxin accumulation, anemia, and metabolic acidosis. Fluid retention becomes prominent, causing edema in the legs, ankles, hands, and face, while breathing difficulties may develop from pulmonary congestion.
Gastrointestinal symptoms intensify, including persistent nausea, vomiting, and appetite loss leading to unintentional weight loss and malnutrition. Neurological manifestations emerge, such as difficulty concentrating, memory problems, sleep disturbances, and restless leg syndrome. Skin complications include severe itching (pruritus), dryness, and discoloration due to uremic toxin deposition and phosphorus retention.
Additional symptoms encompass:
- Muscle cramps and bone pain
- Metallic taste in mouth
- Persistent headaches
- Shortness of breath during minimal exertion
- Changes in urination patterns (frequency, color, foaming)
- Sexual dysfunction
- Depression and anxiety
Serious Health Complications
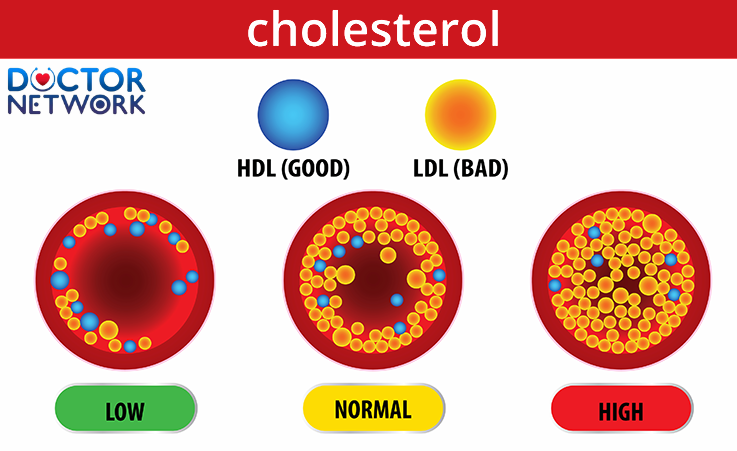
Stage 4 CKD triggers multiple serious complications that increase morbidity and mortality risk. Cardiovascular disease emerges as the leading cause of death, with patients facing elevated risks of heart attack, stroke, and sudden cardiac death due to hypertension, fluid overload, and mineral bone disorders.
Cardiovascular Complications:
- Hypertension affecting 85-95% of patients
- Left ventricular hypertrophy
- Coronary artery disease
- Heart failure
- Arrhythmias
Hematological Issues:
- Anemia due to decreased erythropoietin production
- Iron deficiency
- Bleeding tendencies from platelet dysfunction
Mineral and Bone Disorders (CKD-MBD):
- Secondary hyperparathyroidism
- Bone pain and fractures
- Vascular calcification
- Phosphorus and calcium imbalances
Metabolic Disturbances:
- Metabolic acidosis
- Hyperkalemia (elevated potassium)
- Uremic toxin accumulation
- Protein-energy wasting syndrome
Factors Influencing Life Expectancy and Prognosis
Age at Diagnosis Impact
Age at diagnosis significantly influences life expectancy in stage 4 CKD patients, with younger individuals facing greater relative mortality risk compared to age-matched peers without kidney disease. However, absolute survival times often favor younger patients due to fewer comorbidities and better physiological reserve.
Statistical data reveals notable patterns:
| Age Group | Stage 3a CKD | Stage 4 CKD | General Population |
|---|---|---|---|
| 40 years | >24 years remaining | 15-20 years remaining | 40+ years remaining |
| 60 years | 10-15 years remaining | 6-10 years remaining | 25+ years remaining |
| 70 years | 4-8 years remaining | 3-5 years remaining | 15+ years remaining |
Overall Health Status and Comorbidities
Underlying conditions dramatically influence prognosis, with diabetes mellitus and hypertension representing the most common causes of CKD progression. Cardiovascular disease, particularly coronary artery disease and heart failure, substantially reduces life expectancy and increases hospitalization rates.
High-Risk Comorbidities:
- Diabetes mellitus (types 1 and 2)
- Uncontrolled hypertension
- Coronary artery disease
- Systemic lupus erythematosus
- Polycystic kidney disease
- Glomerulonephritis
- Chronic infections
- Heavy metal toxicity
Treatment Adherence and Lifestyle Factors
Medication compliance and lifestyle modifications significantly impact disease progression and survival outcomes. Patients who consistently take prescribed medications, follow dietary restrictions, and maintain regular medical appointments demonstrate slower CKD progression and improved quality of life measures.
Key Adherence Factors:
- Medication compliance rates >80%
- Regular nephrology follow-up appointments
- Blood pressure monitoring and control
- Dietary phosphorus and potassium restrictions
- Fluid intake management
- Smoking cessation
- Regular physical activity within limitations
Healthcare Disparities and Access
Healthcare disparities profoundly affect CKD outcomes, with racial, ethnic, and socioeconomic factors influencing disease progression, treatment access, and survival rates. African American and Hispanic populations experience higher CKD incidence rates and faster progression to end-stage renal disease compared to Caucasian patients.
Contributing Factors to Disparities:
- Socioeconomic status affecting treatment access
- Geographic barriers to specialized care
- Insurance coverage limitations
- Cultural and linguistic barriers
- Implicit bias in healthcare delivery
- Delayed referral to nephrology specialists
Efforts to Address Disparities:
- Community outreach programs
- Culturally competent care initiatives
- Telemedicine expansion
- Patient navigation services
- Enhanced interpreter services
- Provider bias training programs
Management and Treatment of Stage 4 CKD to Extend Life Expectancy
Treatment Objectives
The primary goals in managing stage 4 CKD focus on slowing disease progression, preventing complications, optimizing quality of life, and preparing for renal replacement therapy. Treatment strategies emphasize comprehensive care coordination addressing medical, nutritional, psychological, and social needs while maintaining patient autonomy and dignity.
Healthcare teams work to achieve specific targets including blood pressure control (<130/80 mmHg), hemoglobin maintenance (10-12 g/dL), phosphorus regulation (3.5-5.5 mg/dL), and parathyroid hormone management. Early preparation for dialysis or transplantation becomes paramount, requiring extensive patient education and vascular access planning.
Medical Monitoring and Specialist Care
Regular nephrology consultation forms the cornerstone of stage 4 CKD management, with the American Kidney Fund recommending appointments every 3 months or more frequently as needed. Comprehensive monitoring involves multiple laboratory parameters, physical assessments, and medication adjustments to optimize outcomes.
Essential Laboratory Tests:
- eGFR calculations using creatinine and cystatin C
- Urine albumin-to-creatinine ratio (UACR)
- Complete metabolic panel including electrolytes
- Complete blood count with differential
- Parathyroid hormone (PTH) levels
- Vitamin D metabolites (25-OH and 1,25-OH)
- Iron studies and ferritin levels
Comprehensive Health Assessments:
- Cardiovascular risk stratification
- Vaccination status review
- Medication reconciliation and safety evaluation
- Blood pressure monitoring and management
- Nutritional status evaluation
- Bone health assessment
Managing Comorbidities and Complications
Blood Pressure Control
Hypertension management remains critical in slowing CKD progression and reducing cardiovascular risk. Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) serve as first-line agents, providing both antihypertensive and renoprotective effects.
Diabetes Management
Glycemic control in diabetic CKD patients requires careful balance between preventing complications and avoiding hypoglycemia. Target HbA1c levels typically range from 7-8%, with adjustments based on individual patient factors and life expectancy.
Anemia Treatment
CKD-related anemia management involves iron supplementation and erythropoiesis-stimulating agents (ESAs) when indicated. Iron studies guide supplementation strategies, while ESA therapy aims for hemoglobin targets of 10-12 g/dL to reduce transfusion requirements and improve quality of life.
Bone and Mineral Disorders
Managing CKD-mineral and bone disorder (CKD-MBD) requires phosphate binders, vitamin D analogs, and calcimimetics to control parathyroid hormone levels and prevent vascular calcification. Dietary phosphorus restriction and calcium supplementation support bone health while minimizing cardiovascular risks.
Fluid Management
Diuretic therapy helps control fluid overload and hypertension, though careful monitoring prevents dehydration and acute kidney injury. Loop diuretics (furosemide, bumetanide) represent first-line agents for volume management.
Lifestyle Modifications for Kidney Health
Kidney-Friendly Nutrition
Implementing a kidney-friendly diet constitutes a fundamental component of CKD management, requiring individualized approaches based on laboratory values, nutritional status, and personal preferences. Collaboration with registered dietitians ensures optimal nutritional support while managing mineral imbalances.
Dietary Principles:
- Protein restriction (0.8-1.0 g/kg/day for non-dialysis patients)
- Phosphorus limitation (800-1000 mg/day)
- Potassium management based on serum levels
- Sodium restriction (<2300 mg/day)
- Fluid intake monitoring when indicated
Foods to Limit or Avoid:
High-Phosphorus Foods:
- Dairy products (milk, cheese, yogurt)
- Nuts and seeds
- Whole grain breads and cereals
- Beans and lentils
- Dark colas and beer
- Processed meats with phosphate additives
High-Potassium Foods (when levels are elevated):
- Bananas, oranges, and melons
- Potatoes and sweet potatoes
- Tomatoes and tomato products
- Spinach and other dark leafy greens
- Avocados
- Salt substitutes containing potassium
Recommended Foods:
- Fresh fruits (apples, berries, grapes)
- Vegetables (cauliflower, cabbage, bell peppers)
- Lean proteins (fish, poultry, eggs)
- Rice and pasta (in moderation)
- Healthy fats (olive oil, small amounts of nuts if phosphorus permits)
Exercise and Physical Activity
Regular physical activity provides numerous benefits for CKD patients, including improved cardiovascular health, better blood pressure control, enhanced mood, and increased functional capacity. Exercise prescriptions should be individualized based on patient fitness levels, comorbidities, and limitations.
Recommended Exercise Program:
- Aerobic activity: 30 minutes, 5 days per week
- Resistance training: 2-3 times weekly
- Flexibility exercises: Daily stretching
- Balance training for fall prevention
Smoking Cessation and Substance Use
Tobacco use accelerates CKD progression by damaging blood vessels, increasing blood pressure, and promoting inflammation. Smoking cessation programs, nicotine replacement therapy, and counseling support improve outcomes and reduce cardiovascular risk.
Alcohol consumption should be limited, as excessive intake can worsen hypertension, interact with medications, and contribute to poor nutritional status. Healthcare providers should screen for substance use disorders and provide appropriate interventions.
Sleep Quality and Stress Management
Sleep disorders are common in CKD patients, affecting up to 80% of individuals with advanced disease. Sleep apnea, restless leg syndrome, and insomnia require evaluation and treatment to improve quality of life and potentially slow disease progression.
Stress management techniques, including meditation, deep breathing exercises, and counseling, help patients cope with the psychological burden of chronic illness while potentially providing physiological benefits through blood pressure reduction and improved medication adherence.
Preparing for End-Stage Renal Disease
Dialysis Education and Planning
As CKD progresses toward stage 5, patients require comprehensive education about renal replacement therapy options. Dialysis typically begins when kidney function drops below 15% (eGFR <15 mL/min/1.73m²) or when uremic symptoms become severe despite optimal medical management.
Hemodialysis Considerations:
- Requires vascular access creation (arteriovenous fistula, graft, or catheter)
- Performed 3 times weekly for 3-4 hours per session
- Requires transportation to dialysis center
- Dietary and fluid restrictions necessary
- Social and lifestyle impacts significant
Peritoneal Dialysis Options:
- Uses peritoneal membrane as filter
- Performed at home with greater flexibility
- Continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis (APD)
- Requires abdominal catheter placement
- Lower infection risk compared to hemodialysis access
Kidney Transplantation Evaluation
Kidney transplantation represents the optimal treatment for eligible patients with end-stage renal disease, offering improved survival rates and quality of life compared to long-term dialysis. The evaluation process involves comprehensive medical, psychological, and social assessments to determine candidacy.
Transplant Evaluation Components:
- Cardiovascular risk assessment
- Cancer screening appropriate for age
- Infectious disease evaluation
- Psychological and social work assessments
- Financial counseling and insurance verification
- Living donor evaluation when applicable
Benefits of Transplantation:
- Improved long-term survival
- Enhanced quality of life
- Freedom from dialysis restrictions
- Better cardiovascular outcomes
- Potential for normal or near-normal kidney function
Palliative and Supportive Care
Palliative care represents an important option for patients who choose not to pursue dialysis or transplantation, focusing on symptom management, comfort, and quality of life. This approach emphasizes comprehensive supportive measures while respecting patient values and preferences.
Palliative Care Components:
- Symptom management (pain, nausea, dyspnea)
- Psychological and spiritual support
- Family counseling and support
- Advanced care planning
- Coordination with hospice services when appropriate
Multifaceted Perspectives on Living with Stage 4 CKD
Impact on Daily Life and Patient Experiences
Living with stage 4 CKD profoundly affects multiple aspects of daily functioning, requiring significant adaptations in work, social activities, and personal relationships. Patients often struggle with fatigue that limits their ability to maintain employment or participate in previously enjoyed activities.
Work and Career Challenges:
- Reduced energy levels affecting job performance
- Frequent medical appointments requiring time off
- Physical limitations impacting certain occupations
- Potential need for workplace accommodations
- Disability considerations and financial implications
Social and Recreational Impact:
- Dietary restrictions affecting social dining
- Travel limitations due to medical needs
- Reduced participation in physical activities
- Impact on family dynamics and relationships
- Financial strain from medical expenses
Patient Voices and Testimonials
Real-world experiences from patients living with advanced CKD provide valuable insights into the challenges and coping strategies that statistical data cannot capture. Jennifer Gowans, a CKD advocate, shares her journey of managing stage 4 kidney disease while maintaining an active lifestyle through careful planning and strong support systems.
Patients consistently emphasize the importance of:
- Building strong relationships with healthcare teams
- Maintaining open communication with family and friends
- Finding meaning and purpose despite health limitations
- Adapting goals and expectations while maintaining hope
- Seeking support from patient communities and advocacy groups
Caregiver Perspectives and Support
Family members and caregivers face significant challenges when supporting loved ones with advanced CKD, experiencing physical, emotional, and financial burdens that require attention and support. Caregivers often struggle with their own health and well-being while managing the complex needs of CKD patients.
Caregiver Challenges:
- Learning complex medical information and procedures
- Managing multiple medications and appointments
- Providing emotional support while dealing with their own fears
- Balancing caregiving with work and other responsibilities
- Financial stress from medical expenses and lost income
Support Resources for Caregivers:
- Caregiver support groups and online communities
- Respite care services
- Educational programs and resources
- Financial assistance programs
- Mental health counseling services
Interdisciplinary Team Approach
Effective management of stage 4 CKD requires coordinated care from multiple healthcare professionals, each contributing specialized expertise to address the complex needs of patients and families.
Key Team Members:
Nephrologist: Serves as the primary specialist managing CKD progression, medication adjustments, and preparation for renal replacement therapy. Nephrologists coordinate overall care and make critical decisions about treatment timing and options.
Registered Dietitian: Provides specialized nutritional counseling to help patients navigate complex dietary restrictions while maintaining adequate nutrition. Dietitians create personalized meal plans and educate patients about food choices that support kidney health.
Social Worker: Addresses psychosocial needs, financial concerns, insurance issues, and community resource connections. Social workers help patients access services, complete disability applications, and navigate healthcare systems.
Dialysis Nurses and Technicians: Provide specialized care during dialysis treatments, monitor patient responses, and educate patients about self-care techniques. These professionals serve as primary contacts for patients receiving dialysis therapy.
Clinical Psychologist: Offers mental health support to help patients and families cope with the emotional challenges of chronic illness, depression, anxiety, and adjustment disorders common in CKD populations.
Primary Care Physician: Continues to manage general health needs, preventive care, and coordination with specialists while supporting overall well-being and addressing comorbid conditions.
Mental Health and Coping Strategies
The psychological impact of stage 4 CKD cannot be underestimated, with depression and anxiety rates significantly higher than in the general population. Patients face multiple stressors including uncertain prognosis, treatment burden, lifestyle limitations, and financial concerns.
Common Mental Health Challenges:
- Depression affecting 20-30% of CKD patients
- Anxiety related to uncertain future and treatment decisions
- Grief and loss related to lifestyle changes
- Fear about dialysis, transplantation, or death
- Social isolation and loneliness
Effective Coping Strategies:
- Professional counseling and therapy
- Peer support groups and patient communities
- Mindfulness and meditation practices
- Maintaining social connections and relationships
- Finding meaning through volunteering or advocacy
- Setting realistic goals and celebrating small achievements
Building Support Systems: Strong support networks prove essential for patients navigating advanced CKD, encompassing family members, friends, healthcare providers, and peer communities. Support groups, both in-person and online, provide opportunities to share experiences, learn coping strategies, and reduce feelings of isolation.
Religious and spiritual communities often provide additional support, helping patients find meaning and hope while dealing with serious illness. Healthcare teams should inquire about spiritual needs and connect patients with appropriate resources when desired.
Prognosis and Future Research Directions
Overall Life Expectancy Outlook
With appropriate management, many individuals with stage 4 CKD can live several years while maintaining reasonable quality of life. Some patients may live more than 10 years before requiring dialysis or transplantation, particularly when diagnosed at older ages with slower disease progression.
Important Prognostic Considerations:
- Individual variation in disease progression rates
- Impact of comorbid conditions on survival
- Effectiveness of treatment interventions
- Access to specialized care and resources
- Patient adherence to treatment recommendations
Data Limitations: Current survival statistics often rely on historical data that may not reflect improvements in modern CKD management. Advances in medications, dialysis techniques, transplantation outcomes, and supportive care continue to improve patient outcomes over time.
Emerging Research and Future Therapies
Current clinical trials investigate novel therapeutic approaches that may slow CKD progression and improve patient outcomes. Research focuses on addressing underlying disease mechanisms, reducing inflammation, protecting residual kidney function, and developing innovative treatment modalities.
Promising Research Areas:
- Novel medications targeting inflammation and fibrosis
- Artificial kidney development and bioengineering approaches
- Regenerative medicine and stem cell therapies
- Improved dialysis technologies and techniques
- Enhanced immunosuppressive protocols for transplantation
- Precision medicine approaches based on genetic factors
Clinical Trial Participation: Patients may benefit from participating in clinical trials, gaining access to experimental treatments while contributing to medical advancement. Healthcare providers can help identify appropriate trial opportunities based on individual patient characteristics and preferences.
Ethical Considerations and Shared Decision-Making
Advanced CKD care involves complex ethical decisions requiring careful consideration of patient values, preferences, and goals of care. Shared decision-making between patients, families, and healthcare teams ensures that treatment choices align with individual priorities and circumstances.
Common Ethical Dilemmas:
- Decisions about initiating or continuing dialysis
- End-of-life care planning and advance directives
- Resource allocation and treatment access
- Quality versus quantity of life considerations
- Family involvement in decision-making processes
Shared Decision-Making Principles:
- Respect for patient autonomy and values
- Transparent communication about prognosis and options
- Consideration of family perspectives and cultural factors
- Regular reassessment of goals and preferences
- Support for difficult decisions through counseling and resources
Healthcare providers should initiate advance care planning discussions early in the disease course, allowing patients and families time to consider options without the pressure of immediate decisions. These conversations should be ongoing, revisited regularly as circumstances change.
Conclusion – Stage 4 Kidney Failure Life Expectancy
Stage 4 chronic kidney disease represents a serious medical condition requiring comprehensive management, but early diagnosis, aggressive treatment, and lifestyle modifications can significantly improve both life expectancy and quality of life. Patients benefit most from working closely with multidisciplinary healthcare teams, adhering to treatment plans, and implementing healthy lifestyle changes to optimize outcomes.
The journey with advanced CKD involves multiple challenges, but numerous resources and support systems exist to help patients and families navigate this difficult path. Advances in medical care, dialysis technologies, and transplantation continue to improve outcomes for individuals with kidney disease.
Most importantly, patients should prepare for alternative treatment options including dialysis and transplantation while disease progression continues. Early preparation, education, and planning provide the best opportunities for successful transitions to renal replacement therapy when needed, ultimately supporting longer, healthier lives despite advanced kidney disease.
5 frequently asked questions about stage 4 kidney failure life expectancy
1. What is stage 4 kidney failure, and how severe is it?
Stage 4 kidney failure, also known as stage 4 chronic kidney disease (CKD), is characterized by severe kidney damage with a glomerular filtration rate (GFR) between 15 and 29 mL/min/1.73 m². At this stage, kidney function is significantly impaired, leading to symptoms like fatigue, swelling, nausea, and complications such as anemia and high blood pressure. It is the last stage before kidney failure (stage 5), where dialysis or transplant becomes necessary.
2. What symptoms are common in stage 4 kidney failure?
Common symptoms include fatigue, weakness, swelling in legs and ankles, shortness of breath, poor appetite, nausea, itching, muscle cramps, sleep disturbances, and cognitive difficulties. These symptoms result from the buildup of waste products and fluid in the body due to impaired kidney function.
3. When will dialysis or kidney transplant be needed?
Dialysis or kidney transplant is usually required when kidney function declines further, typically when GFR falls below 15 mL/min/1.73 m² or when symptoms of kidney failure (such as severe fluid overload or uremia) become unmanageable. Stage 4 is a critical period for preparing for these treatments to avoid emergency situations.
4. What factors affect life expectancy in stage 4 kidney failure?
Life expectancy varies widely and depends on age, presence of other conditions (such as diabetes or heart disease), adherence to treatment, and whether dialysis or transplant is available. Many patients live 5 to 10 years or more after entering stage 4, especially if they follow medical advice and lifestyle changes.
5. How can patients improve their outlook and quality of life?
Managing stage 4 CKD involves close medical monitoring, medications to control blood pressure and anemia, a kidney-friendly diet low in sodium, potassium, and phosphorus, fluid management, and avoiding harmful habits like smoking. Regular exercise and addressing symptoms promptly also help slow progression and improve well-being.
References
1. Understanding Stage 4 Kidney Failure
First, it is crucial to define Stage 4 CKD:
Definition: Stage 4 CKD is characterized by a severe decrease in the estimated Glomerular Filtration Rate (eGFR).
eGFR Range: 15-29 mL/min/1.73m². This means the kidneys are functioning at only 15-29% of their normal capacity.
Clinical State: At this stage, complications such as anemia, bone disease, high blood pressure, and malnutrition are common and require active management. It is the last stage before kidney failure (Stage 5, or End-Stage Renal Disease – ESRD), where dialysis or a transplant is necessary for survival.
2. Key Scientific Studies and Evidence
Life expectancy in CKD is not a simple number. It is derived from large-scale observational (cohort) studies that track thousands of patients over many years.
A. The Impact of eGFR and Age
Age is the single most important predictor of life expectancy in patients with CKD. Studies consistently show that the remaining years of life decrease as both age increases and eGFR decreases.
Key Study: O’Hare, A. M., Choi, A. I., Bertenthal, D., et al. (2007). “Age Affects the Association between Kidney Function and Mortality.” Journal of the American Society of Nephrology (JASN), 18(10), 2758–2765.
Methodology: This influential study analyzed data from a large cohort of U.S. veterans. It calculated the estimated remaining life expectancy for men at different ages and different levels of kidney function.
Key Findings:
A 40-year-old man with normal kidney function (eGFR >60) has a life expectancy of about 38 more years. With Stage 4 CKD (eGFR 15-29), this drops to approximately 12-15 more years.
An 80-year-old man with normal kidney function has a life expectancy of about 8 more years. With Stage 4 CKD, this drops to about 3-4 more years.
Conclusion: This study powerfully illustrates that while CKD shortens life at all ages, the absolute number of years lost is much greater for younger individuals.
B. The Combined Role of eGFR and Albuminuria (Protein in Urine)
Modern prognosis models use both eGFR and the amount of protein (specifically albumin) in the urine to predict risk. Higher levels of albuminuria are associated with a worse prognosis at any given eGFR level.
Key Research Group: The Chronic Kidney Disease Prognosis Consortium (CKD-PC). This is a global collaboration that pools data from dozens of studies involving millions of participants.
Source: Matsushita, K., van der Velde, M., Astor, B. C., et al. for the Chronic Kidney Disease Prognosis Consortium. (2010). “Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis.” The Lancet, 375(9731), 2073–2081.
Methodology: A meta-analysis of over 1.5 million participants from various general population and high-risk cohorts. They created a “heat map” of risk for mortality, cardiovascular events, and kidney failure based on both eGFR and albuminuria categories.
Key Findings: For a patient in Stage 4 CKD (eGFR 15-29), the risk of all-cause mortality is already very high. However, if that patient also has severe albuminuria (over 300 mg/g), their risk is substantially higher than a patient in Stage 4 with little or no albuminuria.
Conclusion: This work established that albuminuria is an independent and powerful risk multiplier. Doctors now use both markers to assess a patient’s prognosis more accurately.
C. Cardiovascular Disease as the Primary Cause of Death
It is a critical point that most patients with Stage 4 CKD do not die from kidney failure itself. They are more likely to die from cardiovascular complications.
Key Study: Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E., & Hsu, C. Y. (2004). “Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization.” New England Journal of Medicine (NEJM), 351(13), 1296–1305.
Methodology: A very large cohort study of over 1.1 million adults within the Kaiser Permanente health system. It was one of the first and most definitive studies to link specific CKD stages to outcomes.
Key Findings: The study found a “graded” relationship: as eGFR declined, the risk for death, cardiovascular events (like heart attack and stroke), and hospitalization increased progressively. For patients with an eGFR of <45 (which includes Stage 4), the risk for death and cardiovascular events was several times higher than for those with normal kidney function, even after adjusting for other risk factors.
Conclusion: This study cemented the understanding that CKD is a major cardiovascular risk factor. The inflammation, anemia, and mineral imbalances associated with CKD put immense strain on the heart and blood vessels.
3. Table of Estimated Life Expectancy (Based on a Combination of Studies)
This table provides estimates to illustrate the impact of age. These are averages and not individual predictions.
| Age at Diagnosis | Gender | eGFR Level (CKD Stage) | Estimated Remaining Lifespan (Years) | Reference Population (General) Lifespan (Years) |
| 40 | Male | Stage 4 (15-29) | ~14 | ~38 |
| 60 | Male | Stage 4 (15-29) | ~6 | ~20 |
| 75 | Male | Stage 4 (15-29) | ~4 | ~10 |
| 40 | Female | Stage 4 (15-29) | ~16 | ~42 |
| 60 | Female | Stage 4 (15-29) | ~8 | ~24 |
| 75 | Female | Stage 4 (15-29) | ~5 | ~12 |
Source: Adapted from data in the JASN (2007) and AJKD studies, representing typical findings in large cohort analyses. Female life expectancy is generally slightly higher.
4. Factors that Improve Life Expectancy in Stage 4 CKD
Statistics are based on populations, but individual outcomes can be improved. Proactive management under the care of a nephrologist (kidney specialist) is critical.
Blood Pressure Control: Using medications like ACE inhibitors or ARBs to protect the kidneys and heart.
Diabetes Management: Strict control of blood sugar (HbA1c) for diabetic patients.
Dietary Management: Following a renal diet (low in sodium, potassium, and phosphorus) and sometimes protein, as guided by a dietitian.
Anemia Management: Treating anemia with iron supplements and/or erythropoiesis-stimulating agents (ESAs).
Managing Bone and Mineral Disease: Using phosphate binders and vitamin D supplements.
Avoiding Nephrotoxins: Avoiding medications harmful to the kidneys, such as NSAIDs (e.g., ibuprofen, naproxen) and certain antibiotics or imaging dyes.
Planning for the Future: Proactively preparing for Stage 5, including education about dialysis and assessing eligibility for a pre-emptive kidney transplant (a transplant before needing dialysis), which offers the best long-term survival.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.