Can High Cholesterol Cause Headaches? Wondering if high cholesterol can cause headaches? Learn the connection and what it means for your health.
The Symptoms of High Cholesterol
Addressing the Core Question
High cholesterol typically does not directly trigger headaches, but the cardiovascular complications it creates can significantly impact cerebral blood flow and contribute to various types of head pain. While hypercholesterolemia itself remains largely asymptomatic—earning its reputation as a “silent killer”—the cascade of vascular changes it initiates may establish pathways to headache development through atherosclerotic processes, hypertension, and inflammatory responses.
This comprehensive analysis examines the intricate relationship between elevated cholesterol levels and headache occurrence. We’ll explore the biological mechanisms linking lipid disorders to cranial pain, investigate specific headache patterns associated with cardiovascular complications, and provide evidence-based diagnostic and treatment approaches. The article covers cholesterol metabolism, headache classification, vascular pathophysiology, clinical presentation, diagnostic protocols, therapeutic interventions, and preventive strategies to deliver a complete understanding of this complex medical relationship.
Understanding High Cholesterol
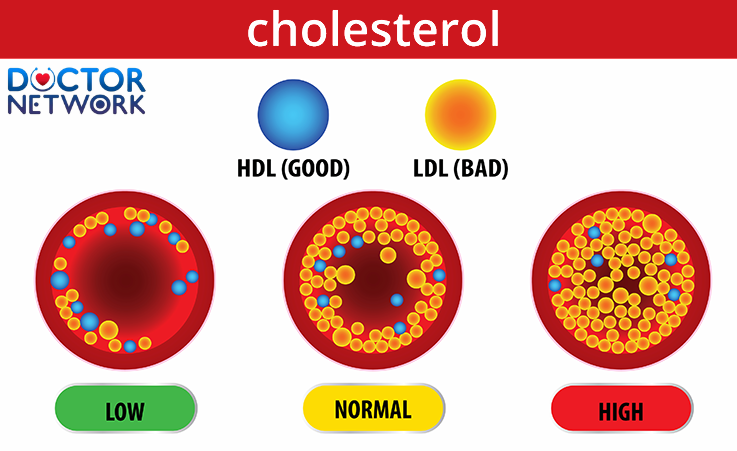
This picture shows what it looks like if you have low, normal, and harmful cholesterol levels.
Cholesterol dysfunction encompasses abnormal levels of lipoproteins circulating in your bloodstream, with low-density lipoprotein (LDL) cholesterol serving as the primary atherogenic particle. High-density lipoprotein (HDL) cholesterol functions as a protective factor by transporting cholesterol from peripheral tissues back to the liver for metabolism and excretion. Triglycerides represent another crucial lipid component that, when elevated, compounds cardiovascular risk factors.
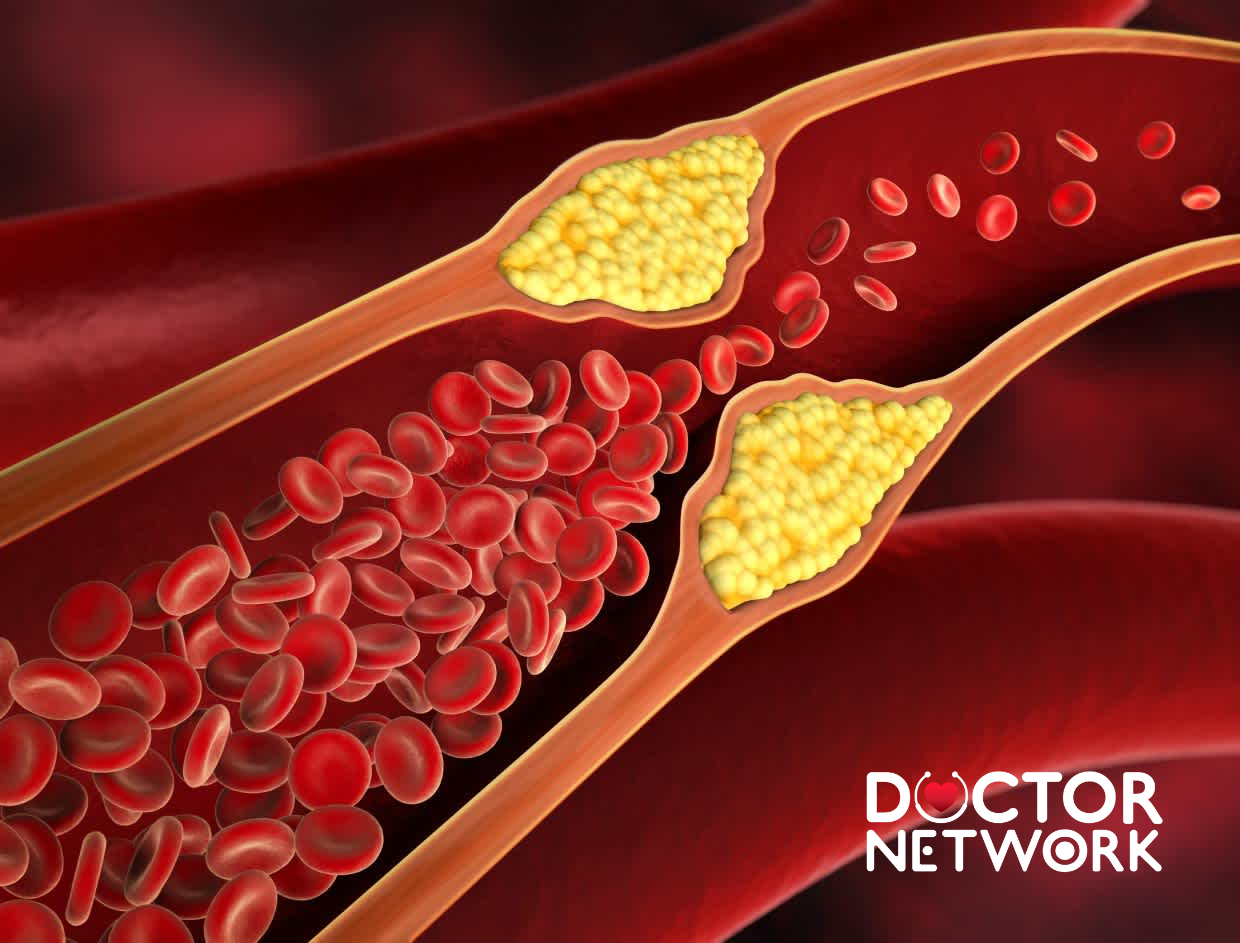
Hyperlipidemia creates substantial risks for cardiovascular disease through atherosclerotic plaque formation within arterial walls. This process begins with endothelial dysfunction, where cholesterol particles infiltrate vessel walls and undergo oxidation. Macrophages attempt to clear these oxidized lipids, transforming into foam cells that accumulate and form fatty streaks. Over time, these lesions progress into complex plaques containing lipid cores, smooth muscle cells, and fibrous caps.
The “silent killer” designation stems from hypercholesterolemia’s typically asymptomatic nature during early stages. Unlike hypertension or diabetes, which may produce noticeable symptoms, elevated cholesterol levels rarely generate immediate physical discomfort. Patients often remain unaware of their condition until routine blood work reveals abnormal lipid profiles or cardiovascular events occur.
From a medical perspective, cholesterol’s impact on the body occurs gradually through systemic vascular changes. These modifications affect blood flow dynamics, vessel elasticity, and inflammatory processes throughout the circulatory system, including cerebral vasculature that supplies the brain with oxygen and nutrients.
Understanding Headaches
Types of Headaches
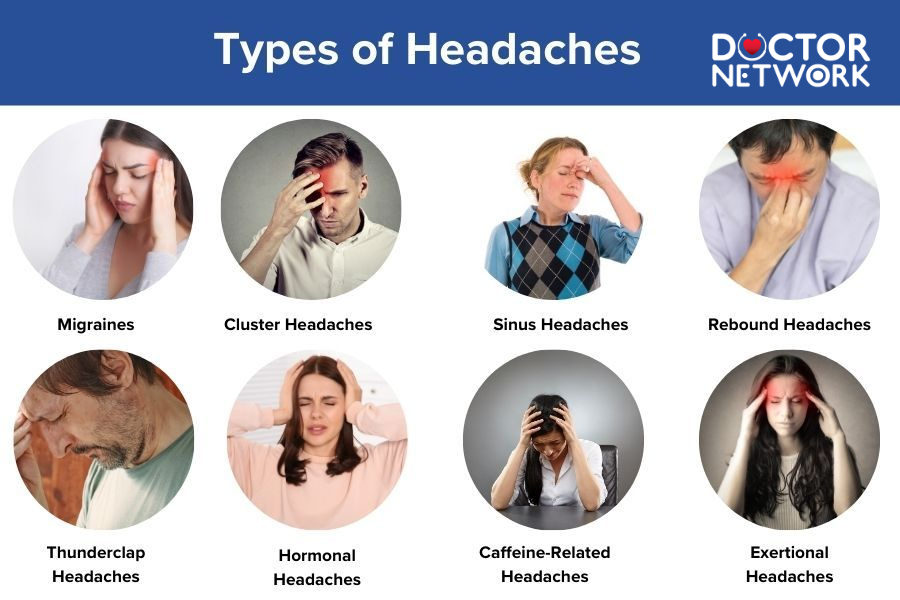
Headache disorders represent one of the most prevalent neurological complaints, with tension-type headaches accounting for approximately 90% of all primary headache episodes. These headaches typically present as bilateral, pressing, or tightening pain without associated nausea or photophobia. Migraine headaches affect roughly 12% of the population and feature unilateral, throbbing pain often accompanied by nausea, vomiting, and sensory sensitivities.
Cluster headaches constitute a less common but severe headache type, characterized by excruciating unilateral pain around the eye or temple region. These episodes occur in cyclical patterns, with patients experiencing multiple attacks daily for weeks or months, followed by remission periods. Secondary headaches result from underlying medical conditions, medications, or structural abnormalities affecting the head and neck region.
Common headache triggers include stress, dehydration, sleep disturbances, eye strain, hormonal fluctuations, dietary factors, and environmental stimuli. Muscular tension in the neck, shoulders, and scalp frequently contributes to tension-type headaches, while vascular changes play a significant role in migraine pathophysiology. Weather changes, bright lights, strong odors, and certain foods can precipitate headache episodes in susceptible individuals.
The vast spectrum of potential headache causes necessitates comprehensive evaluation to identify underlying factors. This broad differential diagnosis includes neurological disorders, vascular conditions, infectious processes, medication effects, and systemic diseases that may manifest with cranial pain as a primary or secondary symptom.
Exploring the Potential Link: Direct vs. Indirect Mechanisms
Direct causation between elevated cholesterol levels and headache occurrence lacks substantial scientific evidence in current medical literature. Cholesterol molecules themselves do not directly activate pain receptors or trigger nociceptive pathways in cranial structures. However, research suggests that severe hypercholesterolemia might influence cerebral blood flow through rheological changes, potentially affecting neuronal function and pain processing.
Indirect mechanisms present more compelling pathways connecting hyperlipidemia to headache development. Atherosclerotic plaque formation within cerebral arteries can compromise blood flow to brain tissue, creating conditions conducive to headache generation. Carotid artery stenosis, resulting from cholesterol-mediated atherosclerosis, may reduce cerebral perfusion and contribute to vascular headache patterns.
Hypertension frequently coexists with hypercholesterolemia, creating a synergistic effect on cardiovascular risk. Elevated blood pressure can trigger headaches through various mechanisms, including increased intracranial pressure, vascular dilation, and altered pain sensitivity. The combination of high cholesterol and hypertension accelerates atherosclerotic progression and amplifies headache risk through compromised cerebrovascular function.
Cerebrovascular events, including stroke and transient ischemic attacks (TIA), represent serious complications of untreated hypercholesterolemia. These conditions often present with severe headaches as initial symptoms, particularly in cases involving posterior circulation territories. The increased stroke risk associated with elevated cholesterol levels creates indirect pathways to headache development through acute vascular events.
Systemic inflammation accompanying atherosclerotic processes may contribute to headache susceptibility through inflammatory mediator release. Chronic low-grade inflammation associated with hyperlipidemia can sensitize pain pathways and lower headache thresholds. Inflammatory cytokines and prostaglandins produced during atherosclerotic plaque formation may influence trigeminovascular system function, potentially triggering headache episodes.
| Mechanism Type | Pathway | Headache Risk | Clinical Evidence |
|---|---|---|---|
| Direct | Cholesterol → Pain receptors | Low | Limited |
| Atherosclerosis | Plaque → Reduced blood flow | Moderate | Established |
| Hypertension | High BP → Vascular changes | High | Strong |
| Stroke/TIA | Acute vascular event | Very High | Definitive |
| Inflammation | Cytokines → Pain sensitization | Moderate | Emerging |
Are There Specific Headache Symptoms Linked to High Cholesterol?

High cholesterol, also known as hypercholesterolemia
Headaches potentially associated with hypercholesterolemia-related complications typically manifest as vascular-type pain patterns rather than specific cholesterol-related characteristics. These headaches often present with throbbing or pulsating quality, may worsen with physical activity, and frequently accompany other cardiovascular symptoms such as chest discomfort, shortness of breath, or dizziness.
Hypertensive headaches linked to concurrent high cholesterol typically occur in the occipital region (back of the head) and may be described as a dull, constant ache that worsens in the morning. These headaches often correlate with blood pressure spikes and may be accompanied by neck stiffness, visual disturbances, or nausea. The pain intensity frequently parallels blood pressure elevation, improving as hypertension is controlled.
Cerebrovascular headaches associated with cholesterol-mediated atherosclerosis may present with sudden onset, severe intensity, and atypical characteristics compared to the patient’s usual headache pattern. Warning signs include headaches accompanied by focal neurological symptoms, altered mental status, speech difficulties, or motor weakness. These presentations require immediate medical evaluation to rule out stroke or other acute cerebrovascular events.
Chronic headache patterns in patients with hyperlipidemia may reflect underlying endothelial dysfunction and compromised cerebral perfusion. These headaches might present as gradually worsening tension-type or mixed headache patterns, often accompanied by cognitive symptoms such as difficulty concentrating, memory problems, or mental fatigue. The relationship between these symptoms and cholesterol levels requires further investigation through clinical studies.
Key Warning Signs Requiring Immediate Medical Attention:
- Sudden, severe headache unlike previous episodes
- Headache with focal neurological symptoms
- Progressive headache with altered consciousness
- Headache accompanied by fever and neck stiffness
- New headache pattern in patients over 50 years old
Diagnosis: How to Determine the Cause of a Headache
Comprehensive headache evaluation begins with detailed medical history taking, focusing on headache characteristics, triggers, family history, and associated symptoms. Physicians assess pain location, quality, intensity, duration, frequency, and temporal patterns to classify headache types and identify potential underlying causes. Cardiovascular risk factor assessment, including cholesterol levels, blood pressure, smoking history, and family history of heart disease, provides crucial diagnostic information.
Physical examination encompasses neurological assessment, cardiovascular evaluation, and musculoskeletal examination of the head and neck region. Blood pressure measurement, fundoscopic examination, and assessment of carotid bruits help identify cardiovascular complications that might contribute to headache development. Neurological examination focuses on detecting focal deficits, altered mental status, or signs of increased intracranial pressure.
Laboratory investigations typically include comprehensive lipid profile testing to assess total cholesterol, LDL cholesterol, HDL cholesterol, and triglyceride levels. Additional blood work may encompass complete blood count, inflammatory markers, thyroid function tests, and vitamin levels to exclude secondary headache causes. Glucose tolerance testing and kidney function assessment help identify metabolic disorders commonly associated with hyperlipidemia.
Advanced diagnostic imaging becomes necessary when clinical presentation suggests secondary headache causes or cerebrovascular complications. Magnetic resonance imaging (MRI) of the brain can detect structural abnormalities, chronic small vessel disease, or silent cerebral infarcts associated with hyperlipidemia. Computed tomography (CT) scanning provides rapid assessment for acute cerebrovascular events, while carotid ultrasound evaluates for atherosclerotic plaque formation and stenosis.
| Diagnostic Test | Purpose | Abnormal Findings | Clinical Significance |
|---|---|---|---|
| Lipid Profile | Assess cholesterol levels | LDL >130 mg/dL | Cardiovascular risk |
| Blood Pressure | Detect hypertension | >140/90 mmHg | Headache trigger |
| Brain MRI | Rule out structural causes | White matter lesions | Vascular disease |
| Carotid Ultrasound | Assess vessel health | Plaque formation | Stroke risk |
Treatment and Management
Cholesterol management represents the cornerstone of addressing potential headache connections through lipid-lowering interventions. Statin therapy, including atorvastatin, simvastatin, and rosuvastatin, effectively reduces LDL cholesterol levels and demonstrates additional anti-inflammatory properties that may benefit headache frequency and intensity. These medications work by inhibiting HMG-CoA reductase, the rate-limiting enzyme in cholesterol synthesis.
Lifestyle modifications form the foundation of comprehensive cholesterol management and headache prevention. Dietary changes emphasizing Mediterranean-style eating patterns, rich in omega-3 fatty acids, antioxidants, and fiber, can improve lipid profiles while potentially reducing headache frequency. Regular aerobic exercise enhances cardiovascular health, improves blood flow, and may decrease headache occurrence through stress reduction and endorphin release.
Concurrent management of associated conditions, particularly hypertension, requires coordinated therapeutic approaches. Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) may provide dual benefits by controlling blood pressure and reducing headache frequency in some patients. Beta-blockers, while effective for hypertension, also serve as migraine preventive medications in appropriate candidates.
Integrated headache management strategies should address both acute symptom relief and preventive measures. For patients with concurrent hyperlipidemia and frequent headaches, preventive medications such as topiramate or propranolol may offer additional benefits. These medications can reduce headache frequency while potentially providing cardiovascular protection or metabolic benefits.
Comprehensive Treatment Approach:
- Statin therapy for cholesterol reduction
- Lifestyle modifications (diet, exercise, stress management)
- Blood pressure control if hypertensive
- Headache-specific treatments (acute and preventive)
- Regular monitoring and follow-up care
Other Factors to Consider
Multiple risk factors commonly coexist with hypercholesterolemia and contribute to both cardiovascular disease and headache development. Obesity significantly increases cholesterol synthesis and alters lipid metabolism while contributing to headache frequency through various mechanisms including sleep apnea, insulin resistance, and chronic inflammation. Weight management through caloric restriction and increased physical activity addresses both conditions simultaneously.
Type 2 diabetes mellitus frequently accompanies hyperlipidemia as part of metabolic syndrome, creating synergistic cardiovascular risks. Diabetic patients experience higher rates of both tension-type and migraine headaches, potentially related to glucose fluctuations, diabetic complications, or medication effects. Optimal glycemic control may reduce headache frequency while improving lipid profiles.
Smoking cessation represents a critical intervention for patients with hypercholesterolemia and headaches, as tobacco use accelerates atherosclerosis and increases headache risk through multiple pathways. Nicotine withdrawal can temporarily worsen headaches, but long-term cessation provides substantial cardiovascular and neurological benefits. Smoking cessation programs should be integrated into comprehensive care plans.
Chronic stress contributes to both cholesterol elevation and headache development through neuroendocrine mechanisms involving cortisol and sympathetic nervous system activation. Stress management techniques, including mindfulness meditation, yoga, and cognitive-behavioral therapy, may provide benefits for both conditions. Regular stress assessment and intervention should be incorporated into patient care protocols.
Dietary factors influence both cholesterol levels and headache susceptibility through various mechanisms. Processed foods high in saturated fats and trans fats worsen lipid profiles while certain food additives may trigger headaches in susceptible individuals. Nutritional counseling should address both cardiovascular risk reduction and headache trigger identification and avoidance.
Bridging the Gap: Cholesterol, Headaches, and Vascular Health
The relationship between high cholesterol and headaches operates primarily through indirect mechanisms rather than direct causation. While hypercholesterolemia itself rarely triggers headaches directly, the cardiovascular complications it generates—including atherosclerosis, hypertension, and increased stroke risk—create significant pathways to headache development. Current medical understanding suggests that managing cholesterol levels may reduce headache frequency by addressing these underlying vascular risk factors.
Atherosclerotic changes in cerebral blood vessels, hypertensive episodes, and inflammatory processes associated with lipid disorders represent the primary mechanisms linking cholesterol elevation to headache occurrence. Patients with both conditions benefit from comprehensive management approaches that address cardiovascular risk factors while providing appropriate headache treatment. The evidence supporting this connection continues to evolve as research explores the complex interactions between metabolic, vascular, and neurological systems.
Effective management requires coordinated care addressing both cholesterol reduction and headache control through lifestyle modifications, appropriate medications, and regular monitoring. Healthcare professionals should maintain awareness of potential connections between these conditions while avoiding overattribution of headaches to cholesterol elevation without proper evaluation of alternative causes.
Prevention strategies emphasizing cardiovascular health promotion may provide dual benefits for both cholesterol management and headache reduction. Patients experiencing frequent headaches in the context of hyperlipidemia should undergo comprehensive evaluation to identify treatable underlying causes and optimize both cardiovascular and neurological outcomes through evidence-based interventions.
Key Takeaways:
- High cholesterol rarely causes headaches directly
- Cardiovascular complications create indirect pathways to headache development
- Comprehensive management addresses both conditions simultaneously
- Healthcare professional consultation is essential for proper diagnosis and treatment
- Prevention strategies benefit both cardiovascular and neurological health
Consultation with qualified healthcare professionals remains essential for accurate diagnosis, appropriate treatment selection, and ongoing monitoring of both cholesterol levels and headache patterns. Individual treatment plans should be tailored to specific patient needs, risk factors, and comorbid conditions to optimize both cardiovascular and neurological outcomes.
Frequently common questions about whether high cholesterol can cause headaches, along with detailed answers based on current research and expert opinions
1. Can high cholesterol directly cause headaches?
No, high cholesterol itself does not directly cause headaches. There is no definitive evidence that elevated cholesterol levels alone trigger headaches or migraines. Headaches are not considered a classic symptom of high cholesterol.
2. How might high cholesterol be related to headaches indirectly?
High cholesterol can lead to atherosclerosis, which is the buildup of cholesterol plaques in arteries. This narrows the arteries and reduces blood flow, including to the brain, which may contribute to headaches or migraines. Additionally, high cholesterol can cause or worsen high blood pressure, a known cause of headaches. Chronic inflammation associated with high cholesterol might also affect blood vessels in the brain, potentially leading to headache episodes.
3. Is there a link between cholesterol levels and migraine severity?
Some studies have found that people with migraines, especially those with aura, tend to have higher total cholesterol and LDL (“bad”) cholesterol levels compared to those without migraines. For example, migraine sufferers often show increased frequency and intensity of headaches when cholesterol levels are elevated. After migraine treatments, cholesterol levels sometimes decrease along with migraine symptoms, suggesting an association. However, these findings show correlation, not causation, and more research is needed.
4. Are headaches more common in people with hyperlipidemia (high cholesterol)?
Research indicates that individuals with hyperlipidemia may experience headaches more frequently, with greater severity and longer duration, compared to people with normal cholesterol levels. This suggests that lipid abnormalities could contribute to headache occurrence, but the exact mechanisms remain unclear.
5. Should people with high cholesterol and headaches be concerned?
While high cholesterol does not directly cause headaches, it is important to manage cholesterol levels to reduce the risk of cardiovascular diseases, which can indirectly affect brain health and potentially contribute to headaches. If you experience frequent or severe headaches along with high cholesterol, it is advisable to consult a healthcare provider to evaluate possible underlying causes such as high blood pressure or atherosclerosis.
References
American Heart Association. (n.d.). What are the Symptoms of High Blood Pressure? Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/why-high-blood-pressure-is-a-silent-killer/what-are-the-symptoms-of-high-blood-pressure
Cleveland Clinic. (2023, October 2). Headaches & High Cholesterol: Is There a Link? Retrieved from https://health.clevelandclinic.org/can-high-cholesterol-cause-headaches
Golomb, B. A., & Evans, M. A. (2008). Statin adverse effects: a review of the literature and evidence for a mitochondrial mechanism. American Journal of Cardiovascular Drugs, 8(6), 373–418. https://doi.org/10.2165/0129784-200808060-00004
Mayo Clinic Staff. (2023, July 22). High cholesterol – Symptoms and causes. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/symptoms-causes/syc-20350800
National Health Service (NHS). (2022, November 24). Statins – Side effects. Retrieved from https://www.nhs.uk/conditions/statins/side-effects/
Serrano-Hernando, F. J., Martín-Láez, R., Simal-Hernández, J. A., & Vázquez-Barquero, A. (2009). Headache as the sole manifestation of symptomatic carotid stenosis. Cephalalgia, 29(5), 576-578. https://doi.org/10.1111/j.1468-2982.2008.01760.x
Vestergaard, K., Andersen, G., Nielsen, M. I., & Jensen, T. S. (1993). Headaches and TIA or minor stroke: a prospective study. Cephalalgia, 13(4), 259-262. https://doi.org/10.1046/j.1468-2982.1993.1304259.x
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.


























