Can popping a gum abscess kill you? a gum abscess can indeed pose life-threatening risks, though immediate death is uncommon – the primary danger lies in bacterial spread that can trigger sepsis, a potentially fatal systemic infection. This seemingly minor dental issue transforms into a serious medical emergency when bacteria from the ruptured abscess enter your bloodstream, potentially affecting vital organs including your heart, lungs, and brain.
This comprehensive guide examines the critical health risks associated with self-draining dental abscesses, explores professional treatment protocols, and provides evidence-based prevention strategies. We’ll cover the pathophysiology of periodontal infections, analyze mortality statistics, discuss emergency interventions, and outline proper wound care techniques to help you make informed decisions about your oral health.
Understanding Gum Abscesses: Medical Definition and Pathogenesis
A gum abscess represents a localized purulent infection within the periodontal tissues, characterized by bacterial colonization and subsequent inflammatory response. These dental infections typically manifest as fluctuant, pus-filled lesions resembling cutaneous boils or pustules along the gingival margin.
The pathogenesis involves bacterial invasion through compromised tissue barriers, often occurring at sites of periodontal disease, dental trauma, or inadequate oral hygiene. Common causative organisms include Streptococcus species, Staphylococcus aureus, and anaerobic bacteria such as Porphyromonas gingivalis and Prevotella intermedia.

Clinical Presentation and Diagnostic Criteria
Dental practitioners identify gum abscesses through characteristic clinical manifestations:
Primary Symptoms:
- Intense, throbbing odontogenic pain
- Localized gingival swelling and erythema
- Purulent discharge with characteristic malodor
- Temperature sensitivity and masticatory dysfunction
Secondary Manifestations:
- Regional lymphadenopathy
- Systemic fever and malaise
- Trismus (limited mouth opening)
- Facial cellulitis in advanced cases
The Fatal Risk: How Popping Abscesses Leads to Sepsis
Self-drainage of periodontal abscesses creates a direct pathway for bacterial dissemination into systemic circulation. When patients rupture these infections manually, they risk introducing additional pathogens while forcing existing bacteria deeper into tissue planes and vascular channels.
Sepsis occurs when the body’s inflammatory response to infection becomes dysregulated, leading to organ dysfunction and potential mortality. The progression follows this dangerous cascade: localized infection → bacteremia → sepsis → septic shock → multi-organ failure.
Mortality Statistics and Risk Factors
| Condition | Mortality Rate | Time to Critical State |
|---|---|---|
| Untreated Dental Abscess | 0.1-0.3% | 24-72 hours |
| Dental Sepsis | 10-40% | 6-24 hours |
| Septic Shock | 40-60% | 2-6 hours |
Healthcare databases reveal approximately 2,000-3,000 deaths annually in the United States from dental infections, with Ludwig’s angina and descending necrotizing fasciitis representing the most severe complications.
High-Risk Patient Populations:
- Immunocompromised individuals (diabetes, HIV, chemotherapy patients)
- Elderly patients with multiple comorbidities
- Individuals with prosthetic heart valves or cardiac devices
- Patients taking immunosuppressive medications
Dangerous Complications of Self-Drainage
Manual rupture of gum abscesses introduces multiple complications that trained dental professionals specifically avoid through sterile technique and complete debridement protocols.
Bacterial Translocation and Systemic Spread
Incomplete drainage leaves residual infected material within periodontal pockets, creating persistent bacterial reservoirs. These organisms can migrate through fascial planes, reaching critical anatomical structures including the parapharyngeal space, retropharyngeal area, and superior mediastinum.
The most feared complication involves bacterial seeding of cardiac structures, particularly in patients with pre-existing valvular disease or prosthetic devices. Infective endocarditis carries mortality rates of 15-30% despite aggressive antibiotic therapy.
Anatomical Spread Patterns
Local Complications:
- Osteomyelitis of the mandible or maxilla
- Periodontal ligament destruction
- Alveolar bone necrosis
- Adjacent tooth involvement
Regional Complications:
- Submandibular space infection
- Parapharyngeal abscess formation
- Cavernous sinus thrombosis
- Orbital cellulitis
Systemic Complications:
- Bacteremia and septicemia
- Infective endocarditis
- Brain abscess formation
- Pneumonia from aspiration
Professional Treatment Protocols vs. Self-Treatment Risks
Dental professionals employ evidence-based protocols that minimize complications while ensuring complete infection resolution. These standardized approaches contrast sharply with the unpredictable outcomes of self-treatment attempts.
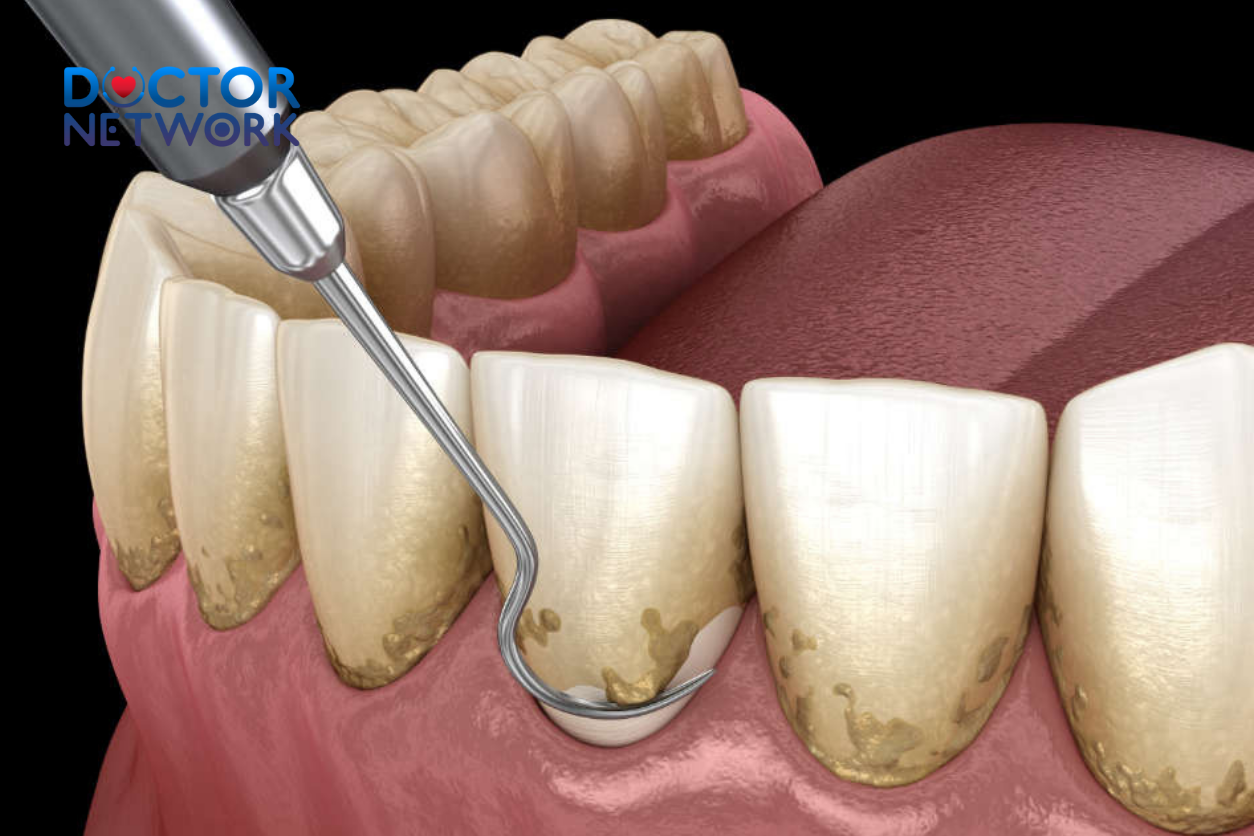
Standard Clinical Management
Phase 1: Emergency Stabilization
- Pain management with appropriate analgesics
- Antibiotic therapy targeting oral pathogens
- Incision and drainage under sterile conditions
- Irrigation with antimicrobial solutions
Phase 2: Definitive Treatment
- Endodontic therapy or extraction
- Periodontal debridement and scaling
- Restoration of damaged tooth structure
- Long-term antimicrobial prophylaxis if indicated
Comparison: Professional vs. Self-Treatment Outcomes
| Treatment Aspect | Professional Care | Self-Treatment |
|---|---|---|
| Sterile Technique | Standard protocol | Contaminated environment |
| Complete Drainage | Ensured through training | Often incomplete |
| Antibiotic Selection | Culture-guided therapy | No antimicrobial coverage |
| Complication Rate | <5% | 25-40% |
| Resolution Time | 3-7 days | Weeks to months |
Emergency Warning Signs Requiring Immediate Medical Attention
Certain clinical presentations indicate progression beyond localized infection, demanding urgent medical intervention to prevent life-threatening complications.
Critical Symptoms Requiring Emergency Care
Immediate Emergency (Call 911):
- Difficulty breathing or swallowing
- High fever with chills and confusion
- Rapid pulse with low blood pressure
- Facial swelling extending to the neck
- Severe trismus preventing mouth opening
Urgent Medical Attention (Within 2-4 Hours):
- Progressive facial swelling
- Persistent fever above 101°F (38.3°C)
- Severe, unrelenting pain
- Pus drainage with increasing odor
- Swollen lymph nodes in neck
Same-Day Dental Care:
- New onset of throbbing pain
- Visible gum swelling or “pimple”
- Bad taste or odor in mouth
- Sensitivity to temperature changes
- Bleeding from gum tissue
Proper First Aid if Abscess Ruptures Naturally
When gum abscesses rupture spontaneously, immediate appropriate care can minimize complications while preparing for professional treatment.
Step-by-Step Emergency Protocol
- Hand Hygiene: Wash hands thoroughly with antimicrobial soap for 20 seconds
- Gentle Drainage: Apply light pressure with clean fingers to express remaining pus
- Oral Irrigation: Rinse mouth with warm saline solution (1 teaspoon salt per cup water)
- Pain Management: Take appropriate over-the-counter analgesics as directed
- Professional Consultation: Contact dental provider within 24 hours
Contraindications and Precautions
- Never use sharp instruments or needles for drainage
- Avoid hydrogen peroxide, which can damage healing tissues
- Don’t apply heat directly to the affected area
- Refrain from consuming alcohol or tobacco products
- Avoid hard or chewy foods that might traumatize the area
Prevention Strategies: Evidence-Based Oral Health Maintenance
Preventing gum abscesses requires comprehensive oral hygiene protocols combined with regular professional monitoring and early intervention for periodontal disease.
Daily Oral Hygiene Protocol
Essential Components:
- Brushing twice daily with fluoride dentifrice
- Daily interdental cleaning with floss or water irrigation
- Antimicrobial mouth rinse for high-risk patients
- Tongue cleaning to reduce bacterial load
Advanced Preventive Measures:
- Professional cleanings every 3-6 months
- Periodontal maintenance for gum disease patients
- Nutritional counseling to support immune function
- Smoking cessation programs
Risk Factor Modification
| Risk Factor | Modification Strategy | Expected Outcome |
|---|---|---|
| Poor Oral Hygiene | Daily plaque removal protocol | 70-80% reduction in infections |
| Diabetes | Glycemic control optimization | 50-60% lower complication rates |
| Smoking | Cessation programs and support | 40-50% improved healing |
| Stress | Management techniques | 20-30% reduced recurrence |
When to Seek Professional Help: Clinical Decision Guidelines
Understanding appropriate timing for professional intervention can prevent minor infections from progressing to life-threatening conditions.
Triage Categories for Dental Infections
Category 1: Immediate Emergency (0-2 hours)
- Airway compromise or breathing difficulty
- Signs of sepsis or systemic toxicity
- Rapid progression of facial swelling
- Altered mental status with fever
Category 2: Urgent Care (2-8 hours)
- Moderate facial swelling without airway involvement
- Persistent fever with localized infection
- Severe pain unresponsive to analgesics
- Progressive lymphadenopathy
Category 3: Routine Appointment (24-48 hours)
- Localized gum swelling without systemic symptoms
- Mild to moderate pain with functional impairment
- New onset of dental sensitivity
- Chronic or recurrent gum infections

Long-term Health Implications and Systemic Connections
Research demonstrates significant associations between periodontal infections and systemic diseases, highlighting the importance of comprehensive oral health management.
Cardiovascular Disease Connections
Periodontal pathogens can directly invade coronary arteries, contributing to atherosclerotic plaque formation and cardiovascular events. Studies indicate a 19-28% increased risk of coronary heart disease in patients with severe periodontal disease.
The inflammatory mediators produced during gum infections, including C-reactive protein and interleukin-6, promote systemic inflammation that accelerates cardiovascular disease progression.
Diabetes and Metabolic Complications
Gum infections create a bidirectional relationship with diabetes mellitus, where periodontal disease worsens glycemic control while hyperglycemia impairs immune response to oral pathogens.
Clinical Implications:
- Diabetic patients show 2-3 times higher rates of severe periodontal disease
- Untreated gum infections can increase HbA1c levels by 0.4-0.7%
- Successful periodontal treatment improves diabetes management
- Regular dental care reduces diabetes-related complications
Respiratory and Pregnancy Outcomes
Aspiration of oral pathogens contributes to pneumonia development, particularly in elderly and hospitalized patients. Pregnant women with severe periodontal disease show increased risks of preterm birth and low birth weight infants.
Conclusion: The Critical Importance of Professional Dental Care
The question “Can popping a gum abscess kill you?” has a clear answer: while immediate death is rare, the potential for life-threatening complications makes self-treatment an unacceptable risk. The bacterial spread from improperly drained abscesses can trigger sepsis, endocarditis, and other fatal conditions that develop rapidly once systemic circulation becomes compromised.
Professional dental care provides the only safe and effective approach to managing gum abscesses. Trained practitioners possess the sterile technique, appropriate instrumentation, and clinical expertise necessary to completely resolve infections while minimizing complication risks.
Prevention through excellent oral hygiene, regular dental visits, and early intervention for periodontal disease remains the most effective strategy for avoiding these potentially dangerous infections. When symptoms develop, seeking immediate professional care can prevent a minor dental problem from becoming a medical emergency.
Remember that your oral health directly impacts your overall well-being. The mouth serves as a gateway to systemic circulation, making proper management of dental infections crucial for maintaining optimal health and preventing life-threatening complications.
5 common questions about “Can Popping a Gum Abscess Kill You?”
1. Is it dangerous to pop a gum abscess at home?
Popping a gum abscess at home is very dangerous because it can cause bacteria to spread further, worsening the infection. Attempting to pop it yourself may push bacteria deeper into the gum tissue, leading to increased swelling, pain, and delayed healing. Without proper treatment, the infection can spread to surrounding areas or even enter the bloodstream, causing serious complications.
2. Can popping a gum abscess cause death?
Although rare, popping a gum abscess can lead to life-threatening complications if the infection spreads into the bloodstream (sepsis) or reaches critical areas such as the brain, neck, or airway. These severe complications require immediate medical attention. Therefore, dental professionals strongly advise against self-popping and recommend seeking professional treatment.
3. What should I do if my gum abscess bursts on its own?
If a gum abscess bursts naturally, you might feel temporary relief due to the release of pressure, but the infection is not fully resolved. You should:
Rinse your mouth gently with warm salt water to clean the area and reduce bacteria.
Spit out the pus instead of swallowing it to prevent spreading bacteria.
Use a clean gauze to control any bleeding.
Take pain relief medication if necessary.
Visit a dentist promptly for proper cleaning and treatment to prevent the infection from spreading.
4. What is the proper treatment for a gum abscess?
Professional treatment typically includes:
A dentist will perform sterile drainage to remove the pus and reduce infection.
Antibiotics may be prescribed to control the infection.
Additional procedures such as deep cleaning, root canal treatment, or tooth extraction might be necessary to eliminate the source of infection.
Follow-up care and good oral hygiene are essential to prevent recurrence.
5. How can I prevent gum abscesses?
Effective prevention includes:
Maintaining good oral hygiene by brushing teeth at least twice a day and flossing daily.
Regular dental check-ups to detect and treat dental issues early.
Avoiding food particles getting trapped between teeth.
Promptly treating dental problems such as cavities and gum disease.
Avoiding harmful habits like smoking and excessive sugar consumption.
Scientific Evidence
Sepsis:
Description: This is a life-threatening condition that arises when the body’s response to an infection injures its own tissues and organs. Bacteria from the dental abscess can enter the bloodstream (bacteremia), leading to a systemic inflammatory response. Sepsis can progress to septic shock, multiple organ failure, and death.
Evidence/Studies:
Textbooks: Standard medical and dental textbooks extensively cover sepsis as a potential complication of untreated or improperly managed infections. Examples include “Oral and Maxillofacial Pathology” (Neville, Damm, Allen, Chi) and “Principles and Practice of Infectious Diseases” (Mandell, Douglas, and Bennett).
Scientific Articles: Numerous case reports and studies document sepsis originating from dental infections.
Source: Anaya, J. M., et al. (2006). Sepsis of dental origin. Medicina Oral, Patología Oral y Cirugía Bucal, 11(3), E221-E224. This review article discusses cases of severe sepsis originating from dental infections.
General Statement: The link between localized infection and sepsis is well-established in medical literature. Any action that promotes the spread of bacteria from a localized site increases sepsis risk.
Ludwig’s Angina:
Description: This is a severe, rapidly spreading cellulitis (bacterial infection of the skin and tissues beneath it) of the floor of the mouth, typically occurring in adults with concomitant dental infections (often from lower molars). Swelling can obstruct the airway, leading to asphyxiation and death if not emergently managed (often requiring a surgical airway like a tracheostomy).
Evidence/Studies:
Textbooks: “Oral and Maxillofacial Surgery” (e.g., edited by Fonseca, Marciani, Turvey) will have detailed sections on Ludwig’s Angina.
Scientific Articles:
Source: Boscolo-Rizzo P, Da Mosto MC. (2009). Submandibular space infection: a potentially lethal infection. International Journal of Infectious Diseases, 13(3), 327-333. This study highlights the life-threatening nature of infections in the submandibular space, including Ludwig’s Angina.
Source: Bridgeman A, Wiesenfeld D, Hellyar A, Sheldon W. (1997). Major maxillofacial infections. An audit of 100 cases. Australian Dental Journal, 42(3), 172-177. This audit includes cases of severe maxillofacial infections, some of which would have been Ludwig’s Angina or similar airway-compromising infections.
Cavernous Sinus Thrombosis:
Description: An infection from an upper tooth (especially canines or premolars) can spread via veins to the cavernous sinus, a large collection of thin-walled veins located at the base of the brain. This can cause a blood clot (thrombosis) in the sinus. It’s a rare but extremely dangerous condition with a high mortality rate or severe neurological deficits.
Evidence/Studies:
Textbooks: “Walsh and Hoyt’s Clinical Neuro-Ophthalmology” (Miller, Newman, Biousse, Kerrison) discusses this condition.
Scientific Articles:
Source: Cannon ML, Antonio BL, McCloskey JJ, et al. (1998). Cavernous sinus thrombosis complicating an odontogenic infection. Pediatric Emergency Care, 14(4), 281-283. A case report illustrating the link.
Source: Yousuf K, Ali KR, Tarakji B, Azzeghaiby SN. (2014). Cavernous sinus thrombosis secondary to odontogenic infection – a case report and literature review. Journal of International Oral Health, 6(2), 104–107.
Brain Abscess:
Description: Bacteria from a dental infection can spread hematogenously (through the blood) or by direct extension through anatomical planes to the brain, forming an abscess. This is a life-threatening neurological emergency.
Evidence/Studies:
Scientific Articles:
Source: Moazzam A, Rajeswaran G, Riaz A, et al. (2015). Intracranial complications of odontogenic infections: A systematic review. International Journal of Surgery, 19, 69-74. This review consolidates evidence on how dental infections can lead to intracranial complications like brain abscesses.
Source: Bali, R. K., Sharma, P., Gaba, S., Kaur, A., & Ghanghas, P. (2015). A review of complications of odontogenic infections. National Journal of Maxillofacial Surgery, 6(2), 136–143. This review also discusses brain abscesses as a potential complication.
Mediastinitis:
Description: Infection from lower teeth can spread down through fascial spaces of the neck into the mediastinum (the space in the chest between the lungs that contains the heart, major blood vessels, esophagus, and trachea). Descending necrotizing mediastinitis has a very high mortality rate.
Evidence/Studies:
Scientific Articles:
Source: Esteves R, et al. (2019). Descending necrotizing mediastinitis of odontogenic origin: a literature review. Revista Portuguesa de Cirurgia Cardio-Torácica e Vascular, 26(1), 29-33.
Source: Freeman RK, Vallières E, Verrier ED, Karmy-Jones R, Wood DE. (2000). Descending necrotizing mediastinitis: an analysis of the effects of serial surgical debridement on patient mortality. The Journal of Thoracic and Cardiovascular Surgery, 119(2), 260-267. While not solely focused on dental origin, it highlights the severity and mortality of mediastinitis.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.