Wisdom teeth cannot regenerate after complete surgical removal, contrary to widespread patient concerns and internet myths. Once an oral surgeon or dental professional extracts the entire third molar—including its crown, roots, and surrounding periodontal structures—the biological machinery necessary for tooth reformation is permanently eliminated. This fundamental principle stems from human dental development, where tooth-forming cells (odontoblasts) and dental lamina remnants cease functioning by early adulthood.
Can Wisdom Teeth Grow Back? – Many patients experience confusion about post-extraction sensations, mistaking normal healing processes for tooth regrowth. This comprehensive analysis will examine the biological impossibility of wisdom tooth regeneration, explore phenomena commonly misidentified as regrowth, clarify what constitutes complete extraction, and provide essential post-operative expectations. Understanding these distinctions helps patients navigate recovery with realistic expectations while recognizing when professional consultation becomes necessary.
Why Wisdom Teeth Don’t Grow Back After Complete Extraction
The Biology of Tooth Formation

Human odontogenesis follows a precisely orchestrated developmental sequence that begins during embryonic stages and concludes by early adulthood. Tooth formation requires active dental lamina—specialized epithelial tissue containing multipotent stem cells capable of initiating tooth bud development. These cellular structures guide enamel formation through ameloblasts, dentin production via odontoblasts, and root development through Hertwig’s epithelial root sheath.
The dental lamina undergoes programmed apoptosis (cell death) after completing its developmental mission, typically before age 25. Third molars represent the final teeth in this developmental cascade, emerging between ages 17-25. Once extraction removes the complete tooth structure, the biological infrastructure for regeneration—including stem cell populations, signaling molecules, and organizational templates—no longer exists within the extraction socket.
Adult human dentition lacks the regenerative capacity observed in certain animal species. Sharks continuously replace teeth throughout their lifespan through persistent dental lamina activity. Humans evolved differently, developing permanent dentition designed for lifelong function rather than continuous replacement. This evolutionary trade-off provides stronger, more durable teeth but eliminates regenerative potential.
What Complete Extraction Means
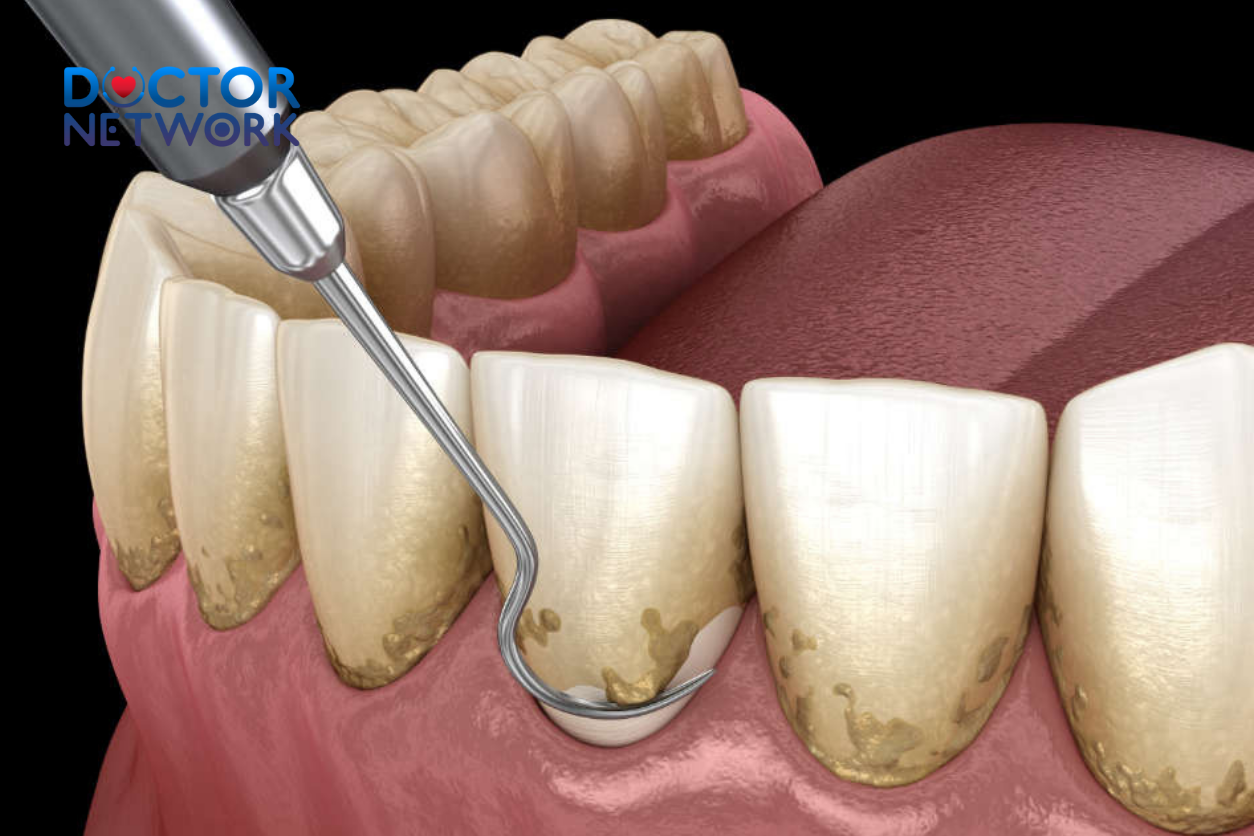
Complete wisdom tooth extraction encompasses total removal of all dental tissues, including the clinical crown, cervical line, and entire root system extending to the apex. Oral surgeons employ specialized elevators, forceps, and occasionally surgical burs to ensure comprehensive extraction of root fragments, particularly when roots exhibit complex morphology or dilaceration.
The extraction process involves careful luxation of periodontal ligament fibers, controlled application of rotational and lateral forces, and meticulous debris removal from the alveolar socket. Post-extraction irrigation eliminates bone fragments, tooth remnants, and infected tissue that could compromise healing. The resulting extraction site undergoes predictable healing phases: blood clot formation, granulation tissue development, and eventual osseous fill-in over 3-6 months.
Successful extraction creates an environment where alveolar bone gradually remodels to restore jawbone contour. Osteoblasts deposit new bone matrix while osteoclasts remove damaged tissue, ultimately creating a smooth, integrated bony surface. This remodeling process confirms complete tooth removal while establishing the biological impossibility of regrowth from the treated site.
What Might Be Mistaken for Wisdom Teeth “Regrowth”
Eruption of Supernumerary Teeth
Supernumerary teeth represent additional tooth buds beyond the normal complement of 32 permanent teeth, occurring in approximately 1-4% of the population. These accessory dental structures develop from hyperactivity of the dental lamina or splitting of existing tooth germs during odontogenesis. Supernumerary molars can remain dormant within jawbone for decades before beginning eruption, particularly in the posterior mandible or maxilla.
When a supernumerary tooth erupts months or years after wisdom tooth extraction, patients may mistakenly attribute this emergence to regrowth of the previously removed tooth. However, supernumerary teeth represent entirely distinct dental structures with separate developmental origins, root systems, and morphological characteristics. These teeth often exhibit altered crown anatomy, including peg-shaped forms, conical configurations, or supplemental molar patterns.
| Characteristic | Regenerated Wisdom Tooth (Myth) | Supernumerary Tooth (Reality) |
|---|---|---|
| Developmental Origin | Same tooth bud as extracted tooth | Separate, additional tooth bud |
| Crown Morphology | Identical to original wisdom tooth | Often altered shape/size |
| Root Formation | Would match original root pattern | Typically different root configuration |
| Eruption Timeline | Immediate post-extraction period | Can occur years later |
| Radiographic Appearance | Would show at exact extraction site | May appear adjacent to extraction site |
Retained Root Fragments
Intentional or inadvertent retention of root fragments represents a recognized complication occurring in 15-20% of complex wisdom tooth extractions. Oral surgeons may deliberately leave small apical fragments when removal risks damage to adjacent anatomical structures, particularly the inferior alveolar nerve or maxillary sinus. These retained fragments typically measure less than 3mm and lack pulpal tissue or odontoblastic activity.
Retained root pieces do not possess regenerative capacity to develop into complete teeth. However, these fragments can cause symptoms that patients misinterpret as tooth regrowth: localized discomfort, intermittent swelling, altered taste sensation, or palpable hard tissue beneath gingival tissue. Bacterial colonization of retained fragments may produce chronic low-grade infection, creating persistent symptoms that seem to indicate ongoing dental activity.
Most retained root fragments remain asymptomatic and gradually integrate with surrounding bone through ankylosis. When fragments cause problems, treatment options include surgical retrieval, antibiotic therapy for associated infections, or continued monitoring with periodic radiographic evaluation. The decision depends on fragment size, location, symptom severity, and patient health status.
Healing Sensations and Bone Remodeling
Normal post-extraction healing produces various sensations that patients may misinterpret as tooth regrowth. The extraction socket undergoes extensive tissue remodeling involving inflammatory responses, angiogenesis (new blood vessel formation), fibroblast proliferation, and osteogenesis (bone formation). These biological processes create sensations including tingling, pressure, throbbing, or perceived movement within the extraction site.
Alveolar bone remodeling continues for 6-12 months after extraction, with most dramatic changes occurring during the first 8 weeks. Initial healing involves blood clot organization and granulation tissue formation, followed by woven bone deposition and eventual lamellar bone maturation. Patients frequently experience pressure sensations as new bone fills the extraction socket, particularly during active osteoblastic phases.
Gingival tissue also undergoes significant remodeling as soft tissues adapt to altered jawbone contours. Epithelial migration, collagen synthesis, and tissue maturation create textural changes that patients may perceive as hard tissue formation. Understanding these normal healing phenomena helps distinguish physiological recovery from pathological conditions requiring professional evaluation.
Eruption or Movement of Adjacent Teeth
Wisdom tooth extraction removes mechanical barriers that may have restricted adjacent second molar movement or eruption completion. Following extraction, second molars occasionally experience slight mesial drift or continued vertical eruption, particularly in younger patients with incomplete root development. This tooth movement can create the illusion of new dental structure appearing in the former wisdom tooth region.
Adjacent tooth movement typically occurs gradually over months to years, representing normal physiological adaptation to altered occlusal forces and spatial relationships. Orthodontic principles suggest that teeth naturally migrate toward areas of reduced resistance, explaining why second molars may shift posteriorly into extraction sites. However, this movement involves existing teeth rather than new tooth formation.
Patients should understand that adjacent tooth movement represents normal dental adaptation rather than wisdom tooth regrowth. Significant tooth migration may require orthodontic intervention if it creates occlusal problems, spacing issues, or compromised oral hygiene access. Regular dental monitoring helps distinguish normal adaptation from problematic tooth movement requiring treatment.
What to Expect After Wisdom Tooth Extraction
Normal Recovery Process and Timeline
Wisdom tooth extraction recovery follows a predictable sequence of healing phases, each characterized by specific symptoms and tissue changes. The immediate post-operative period (24-72 hours) involves blood clot stabilization, initial inflammatory response, and acute pain management. Patients typically experience moderate to severe discomfort, facial swelling, and limited mouth opening during this critical healing window.
The inflammatory phase (days 3-7) features peak swelling, gradual pain reduction, and early granulation tissue formation. Soft tissue healing accelerates as epithelial cells begin covering the extraction site, while inflammatory mediators promote angiogenesis and cellular proliferation. Patients notice improved comfort and function as acute symptoms subside, though complete healing requires several weeks.
| Healing Phase | Timeline | Expected Symptoms | Tissue Changes |
|---|---|---|---|
| Immediate (0-72 hours) | First 3 days | Severe pain, bleeding, swelling | Blood clot formation, hemostasis |
| Inflammatory (3-7 days) | Week 1 | Peak swelling, moderate pain | Inflammatory response, early granulation |
| Proliferative (1-3 weeks) | Weeks 2-3 | Decreasing symptoms | Granulation tissue formation |
| Remodeling (3-12 weeks) | Months 1-3 | Minimal symptoms | Bone formation, tissue maturation |
| Maturation (3-6 months) | Months 3-6 | Complete resolution | Final bone remodeling |
Managing Common Post-Operative Symptoms
Effective symptom management requires understanding normal post-extraction experiences versus complications requiring professional intervention. Swelling typically peaks 48-72 hours after surgery, then gradually subsides over 7-10 days. Ice application during the first 24 hours helps minimize inflammatory response, while warm compresses after day 2 promote circulation and healing.
Pain management involves a multimodal approach combining prescription analgesics, anti-inflammatory medications, and supportive care measures. Most patients experience significant pain relief within 3-5 days, with complete resolution by 7-10 days. Persistent or worsening pain beyond this timeline may indicate complications such as dry socket, infection, or retained debris.
Essential Post-Operative Care Guidelines:
- Apply ice packs 20 minutes on, 20 minutes off for first 24 hours
- Take prescribed medications as directed, including antibiotics if indicated
- Maintain gentle oral hygiene while avoiding extraction site disruption
- Consume soft, lukewarm foods and avoid carbonated beverages
- Avoid smoking, alcohol, and strenuous physical activity for 72 hours
- Sleep with head elevated to reduce swelling and promote drainage
- Attend scheduled follow-up appointments for progress evaluation
Recognizing Complications and When to Seek Care
While most wisdom tooth extractions heal without problems, certain complications require prompt professional attention. Dry socket (alveolar osteitis) occurs in 5-10% of extractions when the blood clot dislodges prematurely, exposing bone and nerve endings. This condition produces severe, throbbing pain typically beginning 2-4 days post-extraction, often accompanied by bad breath and unpleasant taste.
Infection signs include persistent or worsening pain beyond day 3, fever above 101°F (38.3°C), increased swelling after initial improvement, purulent drainage, and lymph node enlargement. These symptoms indicate bacterial invasion requiring antibiotic therapy and possible surgical intervention. Delayed healing or unusual tissue appearance also warrants professional evaluation.
Warning Signs Requiring Immediate Professional Contact:
- Severe, worsening pain after day 3
- Fever, chills, or signs of systemic infection
- Excessive bleeding that doesn’t respond to pressure
- Numbness or tingling persisting beyond 24 hours
- Difficulty swallowing or breathing
- Unusual discharge or persistent bad taste
- Signs of allergic reaction to medications
Addressing Patient Anxiety and Concerns
Post-extraction anxiety often stems from unfamiliarity with normal healing processes and fear of complications. Patients frequently worry about pain duration, infection risk, and long-term consequences of tooth removal. Education about expected recovery phases helps alleviate concerns while providing realistic expectations for healing progression.
Communication between patients and dental professionals plays a crucial role in successful recovery outcomes. Patients should feel comfortable discussing unusual sensations, asking questions about healing progress, and seeking clarification about post-operative instructions. Regular follow-up appointments provide opportunities to assess healing, address concerns, and modify treatment plans when necessary.
Many patients express specific anxiety about the permanence of tooth removal and potential regrowth. Understanding the biological impossibility of wisdom tooth regeneration helps patients accept the definitive nature of extraction while focusing on optimal healing outcomes. This knowledge empowers patients to distinguish normal healing sensations from pathological conditions requiring intervention.
Conclusion

Complete wisdom tooth extraction definitively eliminates any possibility of tooth regrowth due to the permanent absence of regenerative dental tissues and developmental structures. The biological reality of human odontogenesis confirms that once extraction removes the entire tooth—including crown, roots, and surrounding periodontal apparatus—no cellular mechanism exists to regenerate identical dental structures at the extraction site.
Phenomena commonly mistaken for wisdom tooth regrowth include supernumerary tooth eruption, retained root fragment symptoms, normal healing sensations, and adjacent tooth movement. Each of these conditions has distinct characteristics, treatment implications, and underlying mechanisms that differ fundamentally from true tooth regeneration. Patients experiencing unusual post-extraction symptoms should consult their oral surgeon or dentist for accurate diagnosis and appropriate management.
Understanding realistic expectations for wisdom tooth extraction recovery empowers patients to navigate the healing process with confidence while recognizing when professional intervention becomes necessary. The combination of proper post-operative care, patient education, and regular professional monitoring ensures optimal outcomes and addresses any concerns that may arise during the recovery period.
5 frequently asked questions
1. Can wisdom teeth grow back after they’ve been removed?
No, wisdom teeth do not grow back after they have been completely removed. The entire tooth, including the root, is extracted during surgery, which prevents any regrowth.
2. Why do some people think their wisdom teeth have grown back?
Sometimes, what appears to be regrowth is actually the eruption of extra teeth called supernumerary teeth. These are additional teeth beyond the usual four wisdom teeth, present in about 2% of people. They can erupt after the original wisdom teeth have been removed but are not true regrowth.
3. Can incomplete extraction cause wisdom teeth to “grow back”?
If a small root fragment is left behind after extraction, it may cause a painful cyst or a tooth-like structure to develop. This is not a new tooth growing but a complication that sometimes requires further treatment.
4. Why are wisdom teeth often removed?
Wisdom teeth are frequently removed because they often do not have enough space to erupt properly, leading to impaction, crowding, pain, infection, or damage to adjacent teeth. They can also be difficult to clean, increasing the risk of decay and gum disease.
5. Can wisdom teeth grow back years later after removal?
No, once wisdom teeth are extracted, they will not grow back later in life. There is no possibility of regrowth in adulthood as adult teeth do not regenerate after removal.
In summary, wisdom teeth do not regrow after extraction. Occasional appearances of extra teeth are due to supernumerary teeth, not true regrowth. Complete removal including roots is key to preventing any recurrence.
Scientific Evidence and Sources:
General Information from Public Health and Veterinary Organizations:
Source: Centers for Disease Control and Prevention (CDC)
Title: “Fleas – Biology” and “Life Cycle and Hosts”
Key Points: The CDC explicitly states that fleas (like the cat flea) can bite and infest pets like dogs and cats, and also bite humans. They highlight that flea bites on humans are usually found around the legs and ankles.
Link (Biology): https://www.cdc.gov/fleas/fleas_biology.html
Link (Life Cycle and Hosts): https://www.cdc.gov/fleas/life_cycle_and_hosts.html (States: “The most common flea is the cat flea, Ctenocephalides felis, which infests cats, dogs, humans, and other mammalian and avian hosts.”)
Authoritative Veterinary Parasitology Literature:
Seminal Review Article:
Title: “The Biology, Ecology, and Management of the Cat Flea”
Authors: Rust, M. K., & Dryden, M. W.
Source: Annual Review of Entomology, Vol. 42:451-473 (January 1997)
Key Points: This highly cited review extensively details the biology of C. felis, its prevalence on both dogs and cats, and its role as a pest to humans. It confirms that C. felis is the predominant flea on domestic pets and readily bites humans. Michael W. Dryden is a leading expert in flea biology and control.
Link (Abstract & Access Options): https://www.annualreviews.org/doi/abs/10.1146/annurev.ento.42.1.451
DOI: 10.1146/annurev.ento.42.1.451
Disease Transmission Potential (Fleas as Vectors):
Fleas from dogs (primarily C. felis) can transmit certain pathogens to humans:Bartonella henselae (Cat Scratch Disease): While cats are the main reservoir, fleas transmit the bacteria between cats, and infected flea feces can contaminate a scratch or bite on a human. Dogs can also carry Bartonella species transmitted by fleas.
Source: CDC
Title: “Bartonella infection (Cat Scratch Disease, Trench Fever, and Carrión’s Disease)”
Dipylidium caninum (Flea Tapeworm): Humans, especially children, can become infected by accidentally ingesting a flea infected with tapeworm larvae (e.g., after petting an infested dog and then putting fingers in their mouth).
Source: CDC – DPDx (Laboratory Identification of Parasites of Public Health Concern)
Title: “Parasites – Dipylidiasis (also known as Dog and Cat Flea Tapeworm Infection)”
Rickettsia typhi (Murine Typhus) and Rickettsia felis (Flea-borne Spotted Fever): Fleas can transmit these rickettsial diseases.
Source: CDC
Title: “Murine Typhus”
Example Study (R. felis):
Title: “Rickettsia felis: A New Spotted Fever Group Rickettsia in Ctenocephalides Fleas from Opossums, Dogs, and Cats”
Authors: Azad, A.F., Radulovic, S., Higgins, J.A., Noden, B.H., & Troyer, J.M.
Source: The Journal of Parasitology, 1997 (This is an older but foundational paper identifying R. felis in fleas from various hosts, including dogs).
Link (JSTOR – may require access): https://www.jstor.org/stable/3284518
Human Reactions to Flea Bites (e.g., Papular Urticaria):
Flea bites can cause itchy, red bumps, often in clusters or lines, typically on the lower legs and ankles. Some people develop an allergic reaction known as papular urticaria.
Example Article (Discussing insect bite reactions, including fleas):
Title: “Papular urticaria: A common and challenging pediatric dermatosis.”
Authors: Steen, C. J., Carbonaro, P. A., & Schwartz, R. A.
Source: International Journal of Dermatology, 2004.
Key Points: While not solely about fleas from dogs, it describes the common human skin reaction to bites from insects like fleas, which are frequently brought into human environments by pets.
Link (PubMed): https://pubmed.ncbi.nlm.nih.gov/15117365/
DOI: 10.1111/j.1365-4632.2004.02079.x
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.