“Can You Get Chlamydia from Kissing?” Worried about chlamydia from kissing? Learn the facts, risks, and how it’s really transmitted in this quick guide.
Can You Get Chlamydia From Kissing? Understanding Transmission Risks

Chlamydia: Can You Catch It from Kissing?
Many people experience anxiety about contracting sexually transmitted infections through everyday intimate contact, particularly wondering if chlamydia can spread through kissing. The direct answer, based on extensive medical research and clinical evidence, is that you generally cannot get chlamydia from kissing, including deep or French kissing. This bacterial infection follows specific transmission pathways that don’t align with the mechanics of oral contact during kissing.
This comprehensive guide will examine the scientific basis behind chlamydia transmission, explain why kissing poses negligible risk, clarify the distinction between kissing and oral sex, and provide evidence-based prevention strategies. We’ll explore the bacterium’s biological requirements, discuss oral chlamydia infections, compare various risk levels, and outline proper testing and treatment protocols to help you make informed decisions about your sexual health.
Section 1: What is Chlamydia?
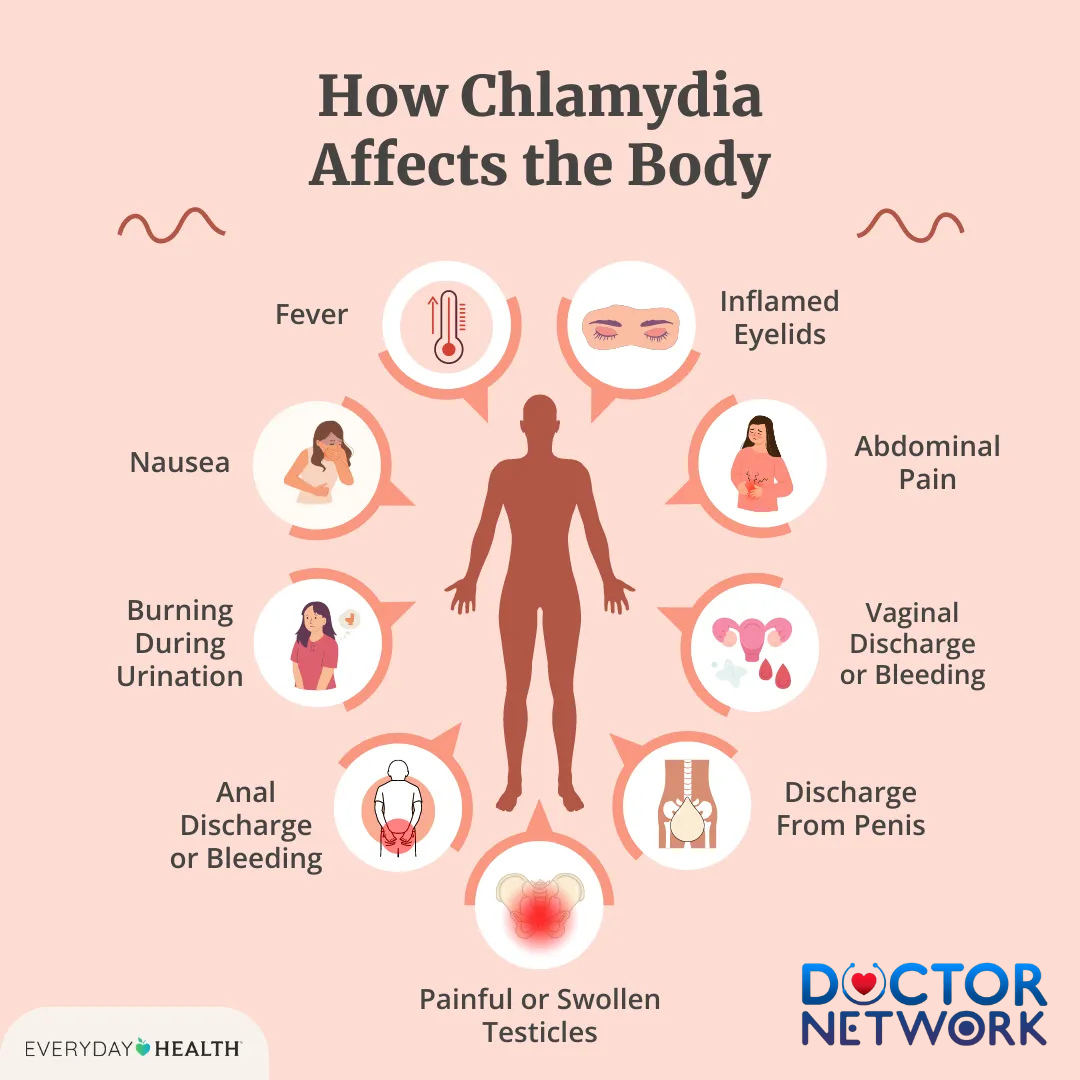
How Chlamydia Affects the Body
Chlamydia represents one of the most prevalent sexually transmitted infections globally, affecting millions of individuals annually across all demographics. This bacterial infection stems from a specific microorganism called Chlamydia trachomatis, which belongs to a unique class of intracellular parasites that require living host cells to survive and reproduce.
Unlike viral sexually transmitted infections such as herpes or HIV, chlamydia’s bacterial nature makes it completely curable with appropriate antibiotic treatment. The pathogen demonstrates remarkable specificity in its target tissues, primarily colonizing mucous membrane surfaces in reproductive organs, rectum, throat, and occasionally the conjunctiva of the eyes.
The infection’s stealth characteristics contribute significantly to its widespread distribution. Most infected individuals remain asymptomatic, unknowingly transmitting the bacterium to sexual partners during unprotected intimate contact. This silent progression allows the infection to establish itself in various anatomical sites before any noticeable symptoms emerge.
Chlamydia trachomatis exhibits particular environmental requirements that directly influence its transmission patterns. The bacterium thrives in warm, moist environments with specific pH levels and nutrient availability, conditions primarily found in genital secretions and certain mucous membrane surfaces.
Section 2: How Chlamydia is Typically Transmitted
Chlamydia transmission occurs exclusively through direct contact with infected bodily fluids containing viable bacteria, specifically requiring access to susceptible mucous membrane tissues. The primary transmission routes involve unprotected sexual activities that facilitate the exchange of genital, anal, or oral secretions between partners.
Primary Transmission Routes
Vaginal transmission represents the most common pathway, occurring when infected cervical or vaginal secretions contact a partner’s genital mucous membranes during penetrative intercourse. The bacteria readily colonize the urethral opening, cervix, and surrounding reproductive tissues in this environment.
Anal transmission follows similar mechanics, with infected rectal secretions or semen facilitating bacterial transfer during anal intercourse. The rectal mucosa provides an ideal environment for Chlamydia trachomatis colonization and subsequent infection establishment.
Oral transmission occurs during oral sex when mouth tissues contact infected genital or anal secretions. This route can result in throat infections or facilitate bacterial transfer from infected oral tissues to a partner’s genitals during reciprocal oral contact.
Maternal-Infant Transmission
Vertical transmission from infected mothers to newborns represents another significant pathway. During vaginal delivery, infants can acquire chlamydia through direct contact with infected cervical secretions, potentially developing conjunctivitis or pneumonia.
| Transmission Route | Risk Level | Required Contact |
|---|---|---|
| Unprotected vaginal sex | High | Direct genital fluid exchange |
| Unprotected anal sex | High | Direct rectal/genital fluid exchange |
| Unprotected oral sex | Moderate to High | Oral-genital mucous membrane contact |
| Mother to child | Moderate | Birth canal passage during delivery |
| Kissing | Negligible | Saliva exchange without genital contact |
The critical factor across all transmission routes involves sufficient bacterial load transfer to susceptible tissue sites. Casual contact, sharing utensils, or touching contaminated surfaces cannot facilitate infection because the bacteria cannot survive outside specific biological environments.
Section 3: Why Kissing is NOT a Typical Transmission Route
Kissing, regardless of intensity or duration, does not constitute a viable transmission mechanism for chlamydia infection based on fundamental biological and environmental factors. The oral cavity during kissing presents an unsuitable environment for Chlamydia trachomatis survival and successful colonization.
Biological Incompatibility
The bacterial species demonstrates remarkable tissue specificity, requiring particular cellular receptors and environmental conditions found primarily in genital, rectal, and specific pharyngeal tissues. Saliva composition, pH levels, and indigenous oral microflora create hostile conditions for chlamydia survival and multiplication.
Chlamydia trachomatis cannot establish sustainable infections through saliva exchange because the bacterium lacks mechanisms to survive the oral environment’s antimicrobial properties. Natural enzymes, competing bacterial populations, and mechanical cleaning actions effectively eliminate any transient bacterial presence during kissing.
Fluid Exchange Distinctions
Standard kissing involves saliva exchange without direct contact between oral tissues and primary infection sites where bacterial concentrations reach transmissible levels. The mucous membranes involved in kissing differ significantly from those targeted during sexual transmission, lacking the specific cellular receptors required for bacterial attachment and invasion.
Even passionate kissing with extensive saliva exchange cannot replicate the conditions necessary for successful transmission. The bacterial load in saliva remains insufficient, and the contact duration with appropriate tissue types proves inadequate for infection establishment.
Oral Sex vs. Kissing Distinction
This fundamental difference separates oral sex from kissing in transmission risk assessment. Oral sex involves direct contact between oral mucous membranes and infected genital or anal tissues, creating ideal conditions for bacterial transfer. The sustained contact, appropriate tissue types, and sufficient bacterial exposure combine to enable transmission.
Kissing lacks these critical elements entirely. The contact remains limited to oral tissues without involvement of primary infection sites, bacterial concentrations remain below transmissible thresholds, and the environmental conditions prevent successful colonization.
Section 4: Understanding Oral Chlamydia
Oral chlamydia infections occur when Chlamydia trachomatis colonizes throat tissues, typically remaining asymptomatic while maintaining transmission potential to sexual partners. These pharyngeal infections develop almost exclusively through oral sex performed on infected individuals, not through kissing activities.
Infection Characteristics
Throat chlamydia establishes itself in specific pharyngeal tissues that share cellular characteristics with genital mucous membranes. The infection often remains clinically silent, producing no noticeable symptoms while maintaining bacterial viability for extended periods.
When symptoms do manifest, they typically include persistent sore throat, throat irritation, or mild pharyngeal discomfort that patients often attribute to common respiratory infections. This symptom overlap frequently delays proper diagnosis and treatment.
Transmission from Oral Sites
Individuals with oral chlamydia can transmit the infection to partners through subsequent oral sex activities. The infected throat tissues contain sufficient bacterial loads to establish genital or anal infections in susceptible partners during oral contact with their reproductive organs.
However, oral chlamydia cannot transmit through kissing because the infection sites remain deeper in the pharyngeal tissues, not on surface areas involved in kissing contact. The bacterial concentrations in saliva remain below transmissible levels even with active throat infections.
Key Misconception Clarification
The existence of oral chlamydia creates confusion about kissing transmission risks. Many individuals incorrectly assume that throat infections automatically create kissing transmission potential. Scientific evidence consistently demonstrates that pharyngeal chlamydia requires specific contact patterns achievable only through oral sex, not casual oral contact.
This distinction proves crucial for accurate risk assessment and prevention planning. Oral chlamydia presence indicates sexual transmission routes, not kissing pathways, requiring appropriate partner notification and treatment protocols.
Section 5: Comparing Risk Levels
Understanding relative transmission risks helps individuals make informed decisions about sexual health practices and prevention strategies. The risk spectrum ranges from negligible (kissing) to significant (unprotected sexual contact) based on biological transmission requirements.
Risk Assessment Framework
Negligible Risk Activities include kissing, sharing utensils, casual contact, and environmental exposure. These activities cannot facilitate transmission because they lack the necessary biological conditions for bacterial survival and colonization.
Moderate Risk Activities encompass protected sexual contact with barrier method failures, oral sex with infected partners, and certain intimate contact patterns involving genital secretion exposure without full protection.
High Risk Activities involve unprotected vaginal, anal, or oral sex with infected partners, multiple concurrent sexual relationships without testing, and sexual contact with individuals of unknown STI status.
| Risk Category | Activities | Transmission Probability |
|---|---|---|
| Negligible | Kissing, casual contact | Effectively zero |
| Low | Protected sexual contact | <5% per exposure |
| Moderate | Inconsistent barrier use | 10-30% per exposure |
| High | Unprotected sexual contact | 30-50% per exposure |
Behavioral Risk Factors
Beyond specific sexual activities, certain behavioral patterns significantly influence overall chlamydia acquisition risk. Multiple concurrent partners, inconsistent testing schedules, and inadequate communication about STI status compound individual exposure risks.
Age demographics also influence risk patterns, with sexually active individuals under 25 experiencing higher infection rates due to various biological and behavioral factors. This elevated risk necessitates more frequent testing and enhanced prevention strategies.
Prevention Priority Assessment
Effective prevention efforts should focus on genuinely high-risk behaviors rather than low-probability transmission concerns. Anxiety about kissing transmission diverts attention from evidence-based prevention strategies that address actual transmission pathways.
Primary Prevention Targets:
- Consistent barrier method use during all sexual activities
- Regular STI testing for sexually active individuals
- Open communication with sexual partners about infection status
- Prompt treatment completion for diagnosed infections
Section 6: Symptoms, Testing, and Treatment
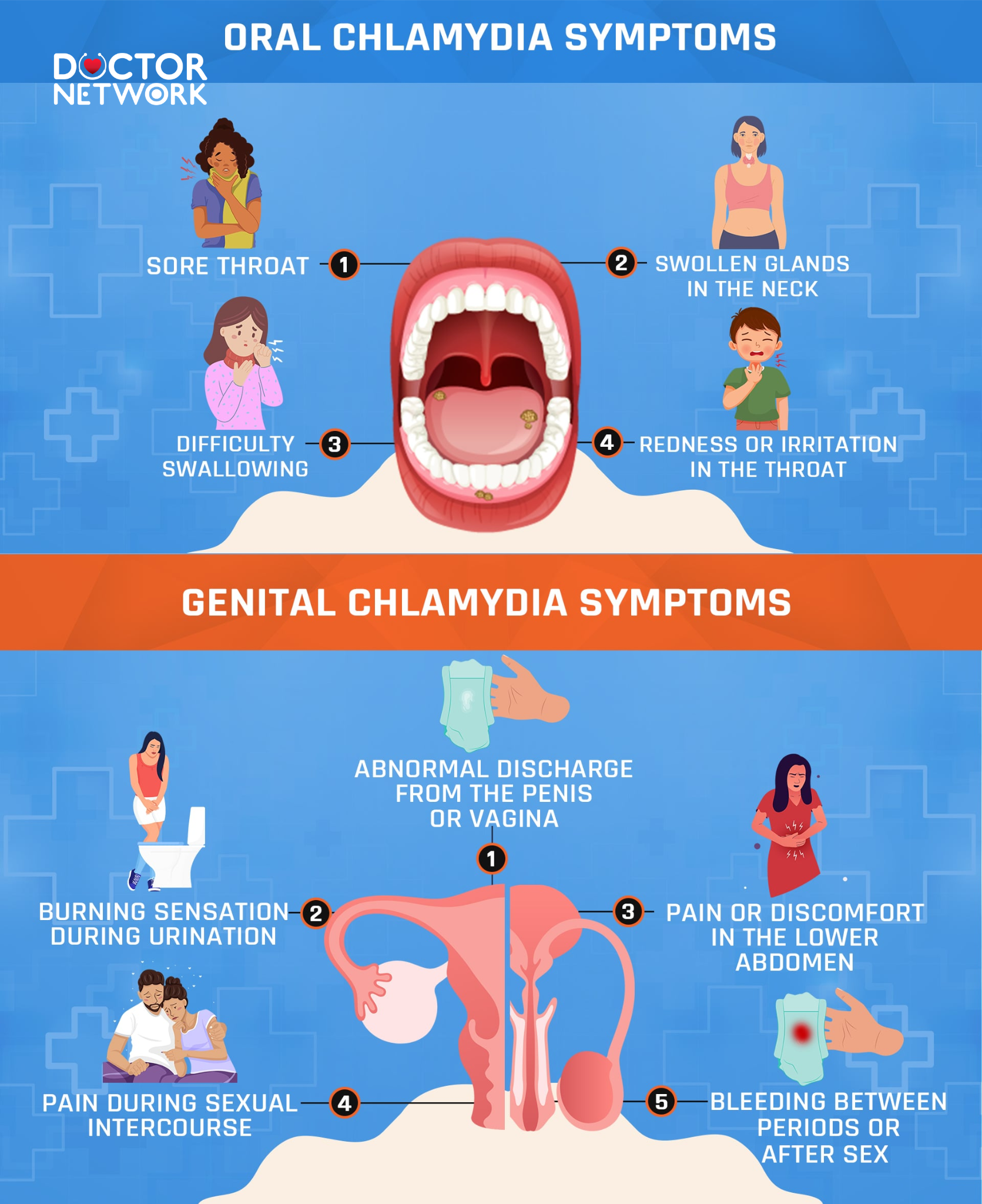
Oral Chlamydia Symptoms & Genital Chlamydia Symptoms
Chlamydia infections frequently progress asymptomatically, creating silent transmission chains that contribute to widespread prevalence. Understanding symptom patterns, testing protocols, and treatment approaches enables effective infection management and prevention.
Symptom Presentations
Genital chlamydia symptoms, when present, typically emerge 1-3 weeks after exposure. Women may experience abnormal vaginal discharge, painful urination, pelvic pain, bleeding between periods, or pain during sexual intercourse. Men commonly report urethral discharge, burning during urination, testicular pain, or rectal discomfort.
Oral chlamydia rarely produces noticeable symptoms, occasionally causing persistent sore throat, throat irritation, or mild pharyngeal discomfort easily mistaken for common respiratory conditions.
Rectal chlamydia may cause anal discharge, rectal pain, bleeding, or discomfort during bowel movements, though many cases remain completely asymptomatic.
Testing Methodologies
Modern chlamydia testing utilizes highly sensitive nucleic acid amplification tests (NAATs) that detect bacterial genetic material with exceptional accuracy. These tests can analyze urine samples, genital swabs, rectal swabs, or throat swabs depending on exposure risks and anatomical sites.
Urine testing provides the most convenient screening method for genital infections, requiring simple sample collection without invasive procedures. This approach works effectively for both men and women, detecting urethral and cervical infections reliably.
Swab testing offers superior sensitivity for specific anatomical sites, particularly rectal and throat locations where urine testing cannot detect infections. Healthcare providers recommend site-specific testing based on sexual behavior patterns and exposure risks.
Testing Recommendations
Frequency Guidelines:
- Sexually active women under 25: Annual screening
- Sexually active men under 25 (high-risk): Annual screening
- All individuals with new partners: Pre-relationship testing
- Anyone with multiple partners: Every 3-6 months
- Symptomatic individuals: Immediate testing
Treatment Protocols
Chlamydia responds excellently to antibiotic treatment, achieving cure rates exceeding 95% with appropriate medication regimens. Standard treatment involves either azithromycin (single dose) or doxycycline (seven-day course), both demonstrating equivalent efficacy.
Treatment Success Factors:
- Complete medication course completion
- Sexual abstinence during treatment period
- Partner notification and simultaneous treatment
- Follow-up testing in certain circumstances
Partner treatment proves essential for preventing reinfection cycles. All sexual partners from the preceding 60 days require evaluation and treatment, regardless of symptom presence or testing results.
| Treatment Option | Dosage | Duration | Cure Rate |
|---|---|---|---|
| Azithromycin | 1g single dose | 1 day | >95% |
| Doxycycline | 100mg twice daily | 7 days | >95% |
| Alternative options | Varies | 7-14 days | >90% |
Section 7: Prevention
Effective chlamydia prevention requires comprehensive strategies addressing actual transmission pathways rather than focusing on low-risk activities like kissing. Evidence-based approaches emphasize barrier protection, regular testing, and partner communication.
Barrier Protection Strategies
Condom effectiveness reaches 85-95% for preventing chlamydia transmission when used consistently and correctly during all sexual activities. Latex and polyurethane condoms provide equivalent protection levels, with proper application and removal techniques proving crucial for optimal effectiveness.
Dental dam usage during oral sex provides effective protection against oral-genital transmission. These barriers prevent direct mucous membrane contact while maintaining intimate experience quality.
Female condoms offer woman-controlled protection options, providing coverage for vaginal and some external genital areas during intercourse.
Testing Integration
Regular STI screening enables early detection and treatment before complications develop or transmission occurs. Testing frequency should align with individual risk factors, relationship patterns, and sexual activity levels.
Testing Schedule Optimization:
- New relationship initiation: Both partners test before unprotected contact
- Multiple partners: Quarterly screening for all sexually active individuals
- Symptom development: Immediate comprehensive testing
- Post-exposure concerns: Testing at appropriate intervals based on exposure timing
Communication Strategies
Open dialogue about sexual health creates supportive environments for prevention and early intervention. Effective communication includes discussing testing history, sharing results, and planning protection strategies collaboratively.
Conversation Framework:
- Share personal testing schedules and recent results
- Discuss preferred protection methods and consistency
- Plan regular health check-ins and testing updates
- Address concerns or symptoms promptly and supportively
Risk Reduction Hierarchy
Primary Prevention focuses on eliminating exposure risks through abstinence, mutual monogamy with tested partners, or consistent barrier method use.
Secondary Prevention emphasizes early detection through regular screening, enabling prompt treatment before complications or transmission events.
Tertiary Prevention involves comprehensive treatment and partner management to prevent reinfection and reduce community transmission rates.
Successful prevention programs combine multiple approaches, addressing individual behaviors, relationship dynamics, and broader public health considerations simultaneously.
Summary of Evidence-Based Prevention and Transmission
Scientific evidence consistently demonstrates that chlamydia cannot transmit through kissing, including passionate or prolonged oral contact. The bacterial infection requires specific transmission conditions involving direct contact between infected secretions and susceptible mucous membrane tissues, circumstances that kissing cannot replicate.
Chlamydia trachomatis spreads exclusively through unprotected sexual contact – vaginal, anal, or oral sex – where infected genital, rectal, or pharyngeal secretions contact a partner’s reproductive tissues. The bacterium’s environmental requirements and tissue specificity make casual contact transmission, including kissing, biologically impossible.
Individuals concerned about STI transmission should redirect their focus toward evidence-based prevention strategies: consistent barrier method use during sexual activities, regular comprehensive testing, and open communication with sexual partners about infection status. These approaches address actual transmission risks while providing effective protection against chlamydia and other sexually transmitted infections.
If you’re sexually active, prioritize regular STI screening regardless of symptom presence, as chlamydia often remains asymptomatic while maintaining transmission potential. Early detection and prompt treatment prevent complications while reducing community transmission rates, contributing to broader public health goals and personal wellness outcomes.
Frequently asked questions about the topic “Can you get chlamydia from kissing?” along with their answers
1. Can you get chlamydia from kissing?
No, you cannot catch chlamydia from kissing because chlamydia is not transmitted through saliva. Kissing someone who has chlamydia is generally considered safe.
2. How is chlamydia transmitted?
Chlamydia is primarily spread through sexual contact involving infected genital fluids, including vaginal, oral, or anal sex without protection. It can also be passed from mother to baby during childbirth.
3. Is it possible to get chlamydia from kissing if there are sores or cuts in the mouth?
The risk remains very low, but theoretically, if a person has infected genital fluids in their mouth and there are open sores or cuts, it might increase the chance of transmission. However, this is very uncommon.
4. Can chlamydia infect the throat?
Yes, chlamydia can infect the throat if transmitted through oral sex. However, this does not mean it can be spread by simple kissing.
5. How can you protect yourself from chlamydia?
To reduce the risk of chlamydia infection, use condoms or dental dams during vaginal, oral, and anal sex, get regularly tested for STIs, avoid sexual contact with infected partners, and communicate openly about sexual health.
References
Centers for Disease Control and Prevention. (n.d.). Chlamydia – Detailed Fact Sheet. Retrieved from https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm
Centers for Disease Control and Prevention. (n.d.). Chlamydia – FAQs. Retrieved from https://www.cdc.gov/std/chlamydia/faqs.htm
National Health Service. (n.d.). Chlamydia – Causes. Retrieved from https://www.nhs.uk/conditions/chlamydia/causes/
Mayo Clinic Staff. (n.d.). Chlamydia trachomatis infection. Retrieved from https://www.mayoclinic.org/diseases-conditions/chlamydia/symptoms-causes/syc-20355349
Edwards, S., Carne, C., & O’Mahony, C. (2000). Detection of Chlamydia trachomatis in semen and saliva from men with and without urethritis. Journal of the European Academy of Dermatology and Venereology, 14(4), 271-274. DOI: 10.1046/j.1468-3083.2000.00091.x
Bissessor, M., Tabrizi, S. N., Fairley, C. K., Danielewski, J., & Hocking, J. S. (2011). Is there a role for kissing in the remote transmission of Chlamydia trachomatis?. Sexually Transmitted Infections, 87(2), 151-152. DOI: 10.1136/sti.2010.045637
Chow, E. P. F., Cornelisse, V. J., Williamson, D. A., Priest, D., Hocking, J. S., Bradshaw, C. S., … & Fairley, C. K. (2019). Is kissing a risk factor for oropharyngeal gonorrhoea? A systematic review and meta-analysis. Sexually Transmitted Infections, 95(5), 313-320. DOI: 10.1136/sextrans-2018-053847 (Included for context on pharyngeal STIs, not direct evidence for chlamydia transmission via kissing).
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.


























