How to cure gum disease without a dentist? This pressing question affects millions of people worldwide who struggle with inflamed, bleeding gums and seek alternative solutions to expensive dental procedures. While home remedies and meticulous oral hygiene practices are essential for preventing periodontal disease and managing its early stage (gingivitis), you cannot completely cure advanced periodontitis without professional dental intervention.
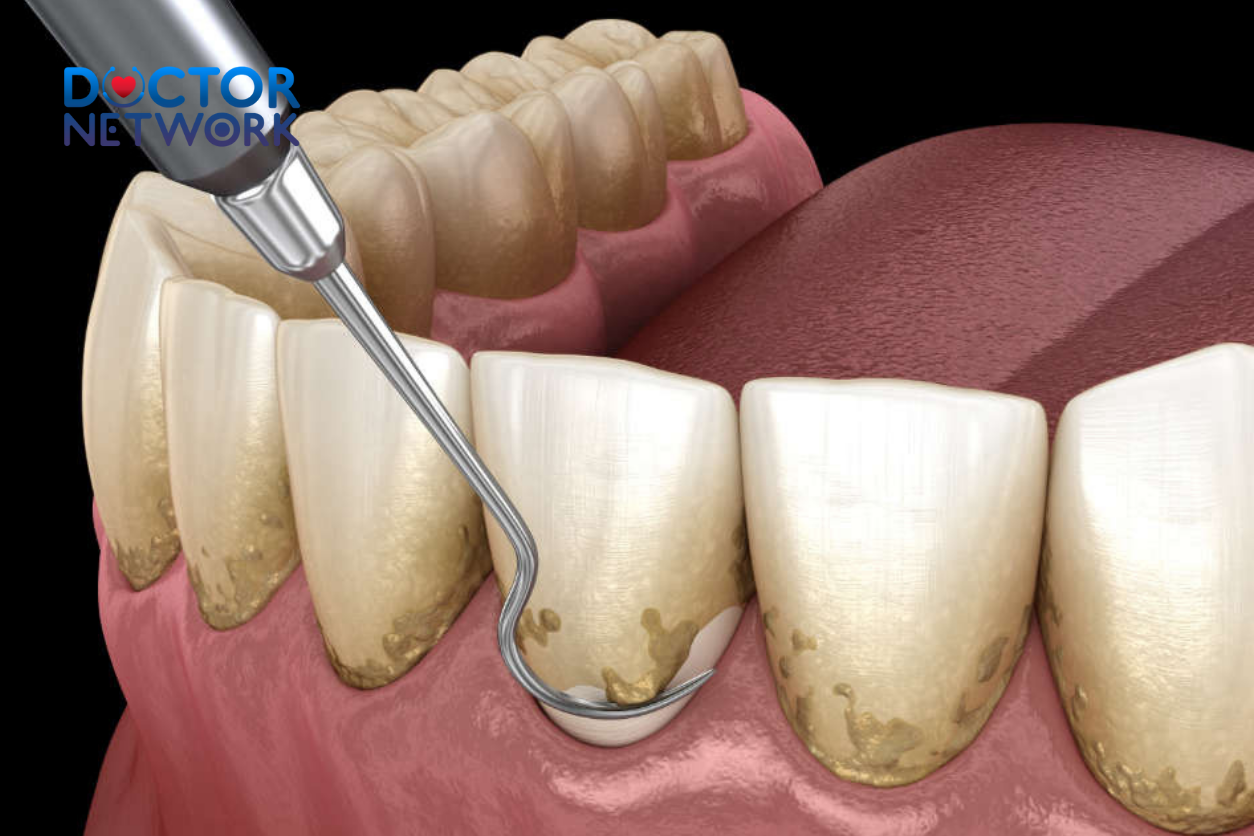
The harsh reality is that bacterial plaque serves as the primary culprit behind gum disease. When plaque accumulates and hardens into tartar (calculus), it becomes impossible to remove through home care alone, requiring specialized dental instruments and professional expertise. This progression follows a predictable pattern: plaque and tartar buildup leads to gingival inflammation (gingivitis), which, if left untreated, can advance to periodontitis, causing irreversible damage to the bone and connective tissue supporting your teeth.
However, home care strategies play a crucial role in preventing gum disease, treating early-stage gingivitis, and supporting professional treatment for more advanced periodontal conditions. This comprehensive guide will explore the science behind gum disease, examine evidence-based home remedies, discuss natural treatments, and explain when professional dental care becomes absolutely necessary.
Throughout this article, we’ll cover the fundamental differences between gingivitis and periodontitis, explore proven home care techniques including oil pulling and herbal mouthwashes, discuss dietary modifications that support gum health, and provide clear guidance on recognizing symptoms that require immediate professional attention. We’ll also examine the broader health implications of untreated periodontal disease and its connections to cardiovascular disease, diabetes complications, and pregnancy risks.
Understanding Gum Disease: Gingivitis vs. Periodontitis
Gum disease represents a bacterial infection affecting the gingival tissues, caused by plaque accumulation that triggers inflammatory responses throughout the oral cavity. This condition exists on a spectrum, ranging from reversible inflammation to permanent tissue destruction.
Gingivitis: The Early, Reversible Stage
Gingivitis manifests as inflammation of the gums that remains completely reversible through proper oral hygiene practices and professional dental care. This initial stage presents with characteristic symptoms including red, swollen, or bleeding gums, particularly noticeable during brushing or flossing activities. Patients typically experience minimal discomfort, teeth remain stable without mobility, and no irreversible damage occurs to the underlying bone or periodontal ligament structures.
The encouraging aspect of gingivitis lies in its complete reversibility. With consistent home care, including thorough plaque removal through brushing and interdental cleaning, combined with professional dental cleanings, the gingival tissues can return to their healthy, pink appearance within weeks.
Periodontitis: The Advanced, Irreversible Stage
Periodontitis develops when gingivitis spreads below the gum line, causing irreversible destruction to the supporting tissues and alveolar bone surrounding the teeth. This advanced stage presents with multiple concerning symptoms that worsen progressively over time.
Key manifestations include:
- Persistent gingival swelling and inflammation
- Chronic halitosis (bad breath) that doesn’t respond to routine oral hygiene
- Gingival recession, making teeth appear longer than normal
- Formation of deep periodontal pockets between gums and teeth
- Tooth mobility or shifting positions
- Pain during mastication (chewing)
- Purulent discharge between teeth and gums
- Metallic taste in the mouth
- Progressive tooth loss in severe cases
Symptoms often remain subtle until patients reach their 40s or 50s, earning periodontitis the nickname “silent disease.” This delayed presentation makes early detection and prevention critically important.
Specialized Types of Periodontitis
| Type | Characteristics | Risk Factors |
|---|---|---|
| Chronic Periodontitis | Slow progression, most common form | Poor oral hygiene, age, smoking |
| Aggressive Periodontitis | Rapid progression, often genetic | Family history, specific bacterial strains |
| Necrotizing Periodontal Disease | Severe tissue death, rare occurrence | Immunocompromised status, stress, malnutrition |

Causes and Risk Factors
Bacterial plaque accumulation serves as the primary cause of all forms of gum disease, creating an environment where pathogenic microorganisms thrive and produce toxins that trigger inflammatory responses.
Primary Contributing Factors
Inadequate Oral Hygiene: Insufficient brushing and flossing allows plaque to accumulate along the gum line, providing nutrients for harmful bacteria to multiply and establish biofilms that resist removal.
Smoking and Tobacco Use: Tobacco products significantly increase periodontitis risk while simultaneously hindering treatment effectiveness by reducing blood flow to gingival tissues and impairing immune system responses.
Nutritional Deficiencies: Diets low in essential nutrients, particularly vitamin C, vitamin D, and antioxidants, compromise immune function and tissue repair mechanisms. Conversely, high intake of processed carbohydrates and sugars feeds harmful oral bacteria.
Systemic Health Connections
Several systemic conditions create predisposing factors for periodontal disease development:
- Diabetes Mellitus: Especially poorly controlled diabetes, creates elevated glucose levels in saliva and compromised immune responses
- Immunocompromising Conditions: Including cancer, HIV/AIDS, and autoimmune disorders
- Hormonal Fluctuations: During puberty, pregnancy, menopause, or oral contraceptive use
- Genetic Predisposition: Family history of periodontal disease increases individual susceptibility
- Medication Side Effects: Drugs that reduce saliva production or cause gingival overgrowth
Age and Lifestyle Factors
Risk increases significantly after age 35, with additional factors including chronic stress, physical irregularities such as crooked teeth or poorly fitting dental restorations, and certain medications that affect oral health.
Home Care Steps & Remedies: Prevention & Early Gingivitis Management
Foundational oral hygiene practices form the cornerstone of gum disease prevention and early-stage treatment, requiring consistent daily implementation and proper technique.
Essential Daily Oral Hygiene Protocol
Proper Brushing Technique: Brush at least twice daily using a soft or extra-soft bristled toothbrush, preferably electric models that provide superior plaque removal. Dedicate two full minutes to brushing all tooth surfaces, replacing toothbrushes every 3-4 months or when bristles become frayed. Use fluoride toothpaste and avoid aggressive brushing that can damage gingival tissues.
Interdental Cleaning: Daily flossing or interdental cleaning removes plaque from areas where toothbrush bristles cannot reach effectively. Options include traditional dental floss, floss picks, interdental brushes of various sizes, or water flossing devices that use pressurized water streams.
Antibacterial Toothpaste: Select toothpaste formulations containing antibacterial agents such as triclosan or stannous fluoride that help reduce harmful bacteria while strengthening tooth enamel.
Evidence-Based Rinses and Mouthwashes
Saltwater Rinse: This natural disinfectant may help reduce plaque accumulation and gingivitis likelihood. A 2017 research study demonstrated saltwater rinses performed as effectively as chlorhexidine in reducing plaque levels, though a 2024 study suggested potentially lower effectiveness compared to chlorhexidine or certain herbal formulations.
Preparation: Mix 1/2 teaspoon salt with warm water, allow cooling to comfortable temperature before use.
Caution: Excessive or long-term use may negatively affect enamel due to increased oral acidity.
Herbal Mouthwashes and Natural Remedies
Lemongrass Oil: Research supports its effectiveness in reducing plaque formation and preventing gingivitis development. Properly dilute essential oil with ethyl alcohol and water to prevent tissue irritation.
Aloe Vera: Studies demonstrate effectiveness equal to chlorhexidine in reducing plaque and gingivitis symptoms. Use 100% pure aloe vera juice without additional dilution requirements.
Tea Tree Oil: A 2020 study showed promising results for gingivitis treatment. Add several drops to warm water for rinsing, or apply one drop to toothpaste before brushing.
Sage: Possesses both antibacterial and anti-inflammatory properties. A 2024 research study found sage mouthwash significantly improved periodontitis symptoms. Prepare by simmering fresh or dried sage with salt in water, then cooling before use.
Guava Leaf: Traditional medicine applications show anti-plaque properties in research studies. Prepare by boiling crushed leaves, cooling the mixture, and adding salt for enhanced effectiveness.
Oil Pulling: Ancient Practice, Modern Benefits
Oil pulling involves swishing oil in the mouth for 20-30 minutes to reduce harmful bacteria and eliminate toxins from oral tissues. This practice allows bacteria to dissolve in the oil, which is then expelled from the mouth.
Coconut Oil: Contains lauric acid with anti-inflammatory and antimicrobial properties. A 2020 study demonstrated significant reductions in plaque and gingivitis signs with regular coconut oil pulling. Use fractionated coconut oil for optimal consistency.
Arimedadi Oil: May help inhibit plaque growth and improve gingivitis symptoms, containing beneficial compounds from clove and acacia. Apply by massaging several drops directly onto gingival tissues.
Important Safety Note: Never swallow oil during or after pulling, as it contains concentrated bacteria and toxins.
Topical Gum Treatments
Apply pea-sized amounts of these treatments directly to gums after brushing and rinsing, avoiding eating or drinking for 30 minutes afterward, then rinse thoroughly.
Ginseng Gel: A 2024 study found ginseng gel performed as effectively as chlorhexidine gel in reducing plaque and dental disease markers.
Curcumin Gel (Turmeric): Research suggests potential benefits for preventing plaque and gingivitis due to potent anti-inflammatory properties found in curcumin compounds.
Dietary and Lifestyle Modifications for Gum Health
Nutrition plays a fundamental role in supporting immune system function and maintaining healthy gingival tissues, while specific lifestyle changes can dramatically impact treatment outcomes.
Optimal Nutrition for Periodontal Health
Balanced Diet Components:
- Fresh fruits and vegetables rich in antioxidants and vitamin C
- Whole grains providing B-vitamins and fiber
- Lean proteins supporting tissue repair
- Calcium-rich dairy products or alternatives strengthening teeth and bones
- Omega-3 fatty acids reducing inflammation
Foods to Limit or Avoid:
- Sugary snacks and beverages that feed harmful bacteria
- Processed foods high in refined carbohydrates
- Sticky candies that adhere to teeth
- Acidic foods that may erode enamel when consumed excessively
Hydration and Oral Health
Drinking adequate water (aim for eight 8-ounce glasses daily) washes away food debris and bacteria while reducing plaque buildup. Water also stimulates saliva production, which provides natural antibacterial protection and helps neutralize acids produced by oral bacteria.
Consider flavoring water with fresh fruit slices or consuming sugar-free herbal teas to maintain interest in proper hydration while supporting oral health goals.
Critical Lifestyle Changes
Smoking Cessation: Quitting tobacco use represents one of the most impactful changes for improving treatment effectiveness and overall periodontal health. Seek professional guidance including nicotine replacement therapy, counseling services, and support groups.
Stress Management: Chronic stress compromises immune system function and may contribute to teeth grinding (bruxism) that damages gums. Implement stress-reduction techniques such as meditation, exercise, or professional counseling.
Managing Underlying Health Conditions: Work with healthcare providers to optimize control of diabetes, autoimmune conditions, and other systemic diseases that affect oral health.
Limitations of Home Remedies & When Professional Care Becomes Essential
Home remedies cannot remove calcified tartar deposits or reverse the irreversible damage caused by advanced periodontitis, making professional intervention necessary for comprehensive treatment.
Critical Limitations of Home Treatment
Even the most diligent home care regimen cannot address certain aspects of periodontal disease:
- Tartar Removal: Once plaque hardens into tartar, only professional scaling instruments can effectively remove these deposits
- Deep Pocket Cleaning: Periodontal pockets deeper than 3-4mm require specialized instruments to access and clean effectively
- Bone Regeneration: Lost alveolar bone cannot regenerate without advanced periodontal surgical procedures
- Accurate Diagnosis: Distinguishing between gingivitis and periodontitis requires professional assessment and diagnostic tools
Immediate Professional Care Warning Signs
| Symptom Category | Specific Warning Signs | Urgency Level |
|---|---|---|
| Pain and Bleeding | Severe pain, persistent bleeding, bleeding after eating | Immediate |
| Tissue Changes | Noticeable gum recession, spaces between teeth, loose teeth | Urgent |
| Persistent Symptoms | Bad breath unresponsive to home care, metallic taste | Prompt |
Seek Professional Care Immediately for:
- Severe pain or bleeding that disrupts daily activities
- Gingivitis symptoms that don’t improve with 2-3 weeks of consistent home care
- Bleeding and tender gums that persist despite proper oral hygiene
- Unexplained bleeding after normal eating activities
- Chronic halitosis that doesn’t respond to thorough oral hygiene
- Noticeable gum recession making teeth appear longer
- New spaces appearing between previously tight teeth
- Any degree of tooth mobility or shifting positions
- Pain during normal chewing activities
- Oral ulcers, red patches, or lumps in mouth tissues
Professional Diagnostic Capabilities
Only qualified dental professionals can accurately diagnose gum disease severity and determine whether you’re dealing with reversible gingivitis or irreversible periodontitis requiring specialized treatment approaches.
The Role of Professional Dental Care: Integrated Treatment Approach
Professional dental care provides essential services that complement and enhance home care efforts, creating a comprehensive treatment strategy for optimal oral health outcomes.
Importance of Regular Dental Visits
Schedule dental visits at least annually, with increased frequency for individuals with gum disease risk factors or active symptoms. Early detection and intervention prevent progression from gingivitis to periodontitis.
Professional Diagnostic Process
Comprehensive Examination: Dentists perform thorough visual and tactile examinations of all oral tissues, noting inflammation, bleeding, and tissue changes.
Periodontal Probing: Specialized instruments measure pocket depths around each tooth, with measurements exceeding 3-4mm indicating potential periodontitis.
Radiographic Assessment: X-rays reveal bone loss patterns and extent of periodontal damage not visible during clinical examination.
Professional Treatment Modalities
Scaling and Root Planing: Deep cleaning procedures remove plaque and tartar from above and below the gum line, with root planing smoothing root surfaces to prevent future bacterial adherence.
Antimicrobial Therapy: Prescription treatments include:
- Chlorhexidine rinses with proven antibacterial effectiveness
- Antibiotic gels or microspheres placed directly into periodontal pockets
- Systemic antibiotics for severe infections or specific bacterial strains
Advanced Surgical Interventions: When conservative treatments prove insufficient, periodontal surgery may involve:
- Flap surgery to access and clean deep pocket areas
- Bone grafting procedures to regenerate lost alveolar bone
- Guided tissue regeneration using specialized membranes
- Soft tissue grafts to cover exposed root surfaces
Integrating Home Care with Professional Treatment
Home care remains critical for maintaining health improvements achieved through professional treatment. Consistent daily oral hygiene prevents reinfection and supports long-term treatment success.
Long-Term Maintenance and Prevention Strategies
Sustainable oral health requires lifelong commitment to consistent daily practices combined with regular professional monitoring and intervention.
Daily Maintenance Protocol
Consistency Priority: Maintain rigorous oral hygiene routines every single day, as even brief lapses can allow harmful bacteria to reestablish and multiply rapidly.
Morning and Evening Routines:
- Thorough brushing with proper technique
- Complete interdental cleaning
- Antibacterial rinse application
- Inspection for changes or concerning symptoms
Professional Monitoring Schedule
Follow your dentist’s recommended schedule for cleanings and examinations, which may range from every 3-6 months depending on your periodontal status and risk factors.
Symptom Monitoring and Response
Key Indicators to Watch:
- Gum color changes from healthy pink to red
- Swelling or puffiness in gingival tissues
- Bleeding during routine oral hygiene
- Changes in breath odor
- Tooth sensitivity or mobility
- Gum recession progression
Response Protocol: Contact your dental professional promptly when symptoms return or worsen, as early intervention prevents progression and complications.
Lifestyle Maintenance
Continue beneficial dietary practices, maintain smoking cessation, manage stress effectively, and address any systemic health conditions that influence oral health.
Potential Broader Health Connections
Untreated periodontitis extends beyond oral health, potentially contributing to serious systemic health complications through bacterial spread and inflammatory responses.
Cardiovascular Disease Links
Research suggests associations between periodontal disease and increased risk of:
- Stroke: Chronic oral inflammation may contribute to cerebrovascular events
- Heart Attack and Coronary Artery Disease: Periodontal bacteria may directly affect arterial health
- Atherosclerosis: Inflammatory processes may accelerate arterial plaque formation
Metabolic and Systemic Complications
Diabetes Complications: Periodontal disease can worsen glycemic control, while diabetes increases periodontitis severity, creating a bidirectional relationship requiring careful management.
Other Systemic Risks:
- Kidney disease progression
- Respiratory infections and lung complications
- Rheumatoid arthritis symptom exacerbation
Pregnancy and Reproductive Health
Pregnant women with periodontal disease face increased risks of:
- Preterm birth delivery
- Low birth weight infants
- Preeclampsia development
- Pregnancy complications
Emerging Research Connections
Recent studies suggest potential links between periodontal disease and:
- Breast Cancer Risk: Particularly among postmenopausal women who smoke
- Cognitive Decline: Potential connections to dementia and Alzheimer’s disease
- Autoimmune Conditions: Shared inflammatory pathways with various autoimmune disorders
The exact mechanisms underlying these connections remain under investigation, but bacterial spread and chronic inflammatory responses likely play significant roles.
5 frequently asked questions about “how to cure gum disease without a dentist”
What are the early signs of gum disease I can recognize at home? Red, swollen, or tender gums, bleeding gums (especially when brushing or flossing), persistent bad breath, receding gums, loose teeth, deep pockets in the gums, and pain when chewing can be early signs of gum disease. Recognizing these symptoms early is key to preventing the disease from progressing.
How does improving my oral hygiene help with gum disease? Plaque and bacteria are major causes of gum disease. Brushing your teeth twice a day for two minutes with fluoride toothpaste, flossing daily to remove plaque and food particles, and using an antibacterial mouthwash can significantly reduce bacteria and keep your mouth clean.
Are there natural remedies that can reduce gum inflammation and bacteria? Yes, several natural remedies can help. A salt water rinse made with warm water can soothe irritated gums and kill bacteria3. Oil pulling with coconut oil for 10-20 minutes can also help reduce harmful bacteria in the mouth3. Additionally, applying a turmeric paste to the gums may reduce swelling and pain due to its anti-inflammatory properties.
How does my diet affect gum disease? A balanced diet rich in vitamins and minerals like Vitamin C and calcium is essential for maintaining strong gums. Staying hydrated helps encourage saliva production, which naturally cleanses the mouth. Reducing sugary and processed foods can also help, as these promote the growth of unwanted bacteria in the mouth.
Can stress and smoking affect gum disease? Yes, stress lowers immunity, making it harder for your body to fight infections like gum disease. Engaging in stress-reducing activities such as yoga and meditation can be beneficial. Smoking reduces blood flow to the gums and impairs healing. Quitting smoking can greatly improve gum health and prevent the risk of periodontal disease.
Conclusion
Gum disease begins with simple plaque accumulation and progresses to gingival inflammation (gingivitis), which often responds well to diligent home care practices and remains completely reversible with proper treatment. However, when gingivitis advances to periodontitis, it causes irreversible damage to supporting structures and requires professional dental intervention to manage effectively and prevent further tissue loss.
Home remedies and excellent oral hygiene represent powerful tools for prevention and treatment support, but they cannot substitute for professional dental care when advanced periodontal disease develops. Natural treatments including oil pulling, herbal mouthwashes, and dietary modifications provide valuable complementary benefits when used appropriately alongside conventional treatments.
The most effective approach to maintaining optimal oral health combines consistent daily home care practices with regular professional dental monitoring and treatment. This integrated strategy prevents serious complications, maintains functional dentition throughout life, and potentially reduces risks of associated systemic health problems.
Early intervention remains crucial – don’t delay seeking professional evaluation if you suspect gum disease development. Prompt diagnosis and appropriate treatment preserve your oral health, protect your overall wellbeing, and prevent costly complications that develop when periodontal disease progresses untreated.
Remember that investing in your oral health today provides lifelong benefits for both your smile and your overall health and quality of life.
References
1. The Foundation: Mechanical Plaque Removal (Brushing and Flossing)
This is the most scientifically validated and essential method for controlling gingivitis. The goal is to physically remove the bacterial plaque film.
Title: Flossing for the management of periodontal diseases and dental caries in adults
Authors: H. V. Worthington, J. MacDonald, P. D. Poklepovic Pericic, et al.
Source: Cochrane Database of Systematic Reviews
Key Findings:
This is a high-level review of existing studies. The authors found “low-certainty evidence” that flossing in addition to toothbrushing may reduce gingivitis more than toothbrushing alone.
While the evidence for flossing specifically is not as robust as one might think, the underlying principle of interdental cleaning (cleaning between the teeth) is universally accepted as critical for removing plaque that a toothbrush cannot reach.
Conclusion: Meticulous and consistent mechanical cleaning is the cornerstone of preventing and reversing gingivitis.
Link: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008829.pub3/full
2. Oil Pulling
This ancient Ayurvedic practice involves swishing oil (typically sesame or coconut) in the mouth. Studies have investigated its effect on plaque and gingivitis.
Title: Effect of oil pulling on plaque induced gingivitis: a randomized, controlled, triple-blind study
Authors: S. Asokan, J. Emmadi, R. Chamundeswari
Source: Indian Journal of Dental Research
Key Findings:
This randomized controlled trial compared oil pulling with sesame oil to a standard chlorhexidine mouthwash in subjects with plaque-induced gingivitis.
The study found that after 10 days, “oil pulling therapy showed a reduction in the plaque index, modified gingival scores, and total colony count of aerobic microorganisms.”
The reduction in gingivitis was statistically significant and was comparable to the effects of the chlorhexidine rinse. This suggests oil pulling can be an effective adjunctive therapy.
3. Herbal Rinses (e.g., Tea Tree Oil)
Various plant extracts have been studied for their antimicrobial and anti-inflammatory properties.
Title: The effect of a tea tree oil-containing mouthwash on plaque and chronic gingivitis
Authors: C. R. Arweiler, D. Donos, M. Netuschil, H. Reich, A. Sculean
Source: Australian Dental Journal
Key Findings:
This study investigated a mouthwash containing tea tree oil. It found that the tea tree oil group showed a “significant reduction of gingival inflammation and bleeding” compared to the placebo group.
It suggests that certain herbal ingredients can have a therapeutic effect on gingivitis, likely due to their antimicrobial and anti-inflammatory properties.
4. Saltwater Rinses (Saline Solution)
This is a common home remedy, though high-level clinical trials are less common than for commercial products. Its mechanism is primarily based on basic science principles.
Title: Wound healing activities of different natural products: A review
Author: P. D. T. M. Rekha, R. K. Kollipara, P. S. Gupta, et al.
Source: Journal of Pharmacy and BioAllied Sciences
Key Findings:
While not a direct study on gum disease, this review (and others like it) discusses the principles of wound healing. A hypertonic saline (saltwater) solution can temporarily increase blood flow, cleanse the area, and create a less favorable environment for some bacteria through osmosis.
It is widely recommended by dentists as a soothing, adjunctive treatment after dental procedures to promote healing and reduce mild inflammation. Its effect on reversing established gingivitis on its own is less documented but is considered a safe, supportive measure.
Link: (This paper provides general context on natural product healing) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8472044/
5. Why Professional Care is Essential for Periodontitis
This resource from the leading professional body for periodontists explains why you cannot treat advanced disease at home.
Title: Scaling and Root Planing
Author: American Academy of Periodontology (AAP)
Source: Perio.org (Patient Resources)
Key Findings:
The AAP explains that the primary cause of periodontitis is plaque and calculus (tartar) that forms below the gum line.
“Home care, such as brushing and flossing, will only clean the portion of the tooth above the gum line.”
Scaling and root planing is a non-surgical procedure performed by a dental professional to manually remove the calculus from deep pockets and smooth the tooth root to help the gums reattach. This cannot be replicated at home with any brush, pick, or rinse.
Link: https://www.perio.org/for-patients/periodontal-treatments-and-procedures/scaling-and-root-planing/
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.