Most people dream of having perfectly clean, smooth teeth, yet many struggle with stubborn, crusty deposits that seem impossible to remove at home. These hardened formations, known as dental tartar or calculus, represent one of the most persistent challenges in oral healthcare. Unlike soft plaque that can be brushed away, tartar bonds firmly to tooth enamel and requires specialized intervention for complete removal.
The reality about tartar elimination may surprise you: while countless individuals search for do-it-yourself solutions and home remedies, genuine removal of existing tartar deposits typically necessitates professional dental intervention. The most effective strategy for managing tartar at home isn’t removal—it’s prevention through meticulous oral hygiene practices.
How to Remove Tartar from Teeth – This comprehensive guide will explore the science behind tartar formation, debunk common misconceptions about home removal methods, explain why professional cleaning remains the gold standard for tartar elimination, and provide evidence-based prevention strategies. We’ll also examine the serious health consequences of untreated tartar buildup, help you recognize early warning signs, and identify risk factors that increase your susceptibility to calculus formation.
What Exactly is Tartar and How Does It Form?
Dental tartar represents the mineralized, hardened form of bacterial plaque that has undergone calcification on tooth surfaces. To understand tartar formation, we must first examine its precursor: dental plaque, a soft, sticky biofilm containing millions of bacteria that continuously accumulates on teeth throughout the day.
Plaque consists primarily of streptococcus mutans, lactobacilli, and other pathogenic microorganisms that feed on food particles and sugars in your mouth. These bacteria produce acids as metabolic byproducts, creating an acidic environment that can damage tooth enamel and irritate gingival tissues.
The transformation from plaque to tartar occurs through a process called mineralization or calcification. When plaque remains undisturbed on tooth surfaces for 24-72 hours, calcium and phosphate ions from saliva begin incorporating into the bacterial matrix. This mineralization process creates a hard, crusty deposit that adheres tenaciously to tooth enamel and root surfaces.
Tartar can form both supragingivally (above the gum line) and subgingivally (below the gum line). Supragingival calculus typically appears yellow or brown due to staining from food, beverages, and tobacco products. Subgingival tartar often appears darker, ranging from brown to black, and poses greater threats to periodontal health due to its proximity to gum tissues and tooth roots.
The mineralization process makes tartar significantly harder than the original plaque biofilm. While regular brushing and flossing can effectively remove soft plaque, these mechanical methods prove inadequate against mineralized calculus deposits. The crystalline structure of tartar creates a rough surface that attracts additional plaque accumulation, perpetuating the cycle of bacterial growth and calcification.
| Plaque vs. Tartar Comparison |
|---|
| Characteristic |
| Consistency |
| Removal Method |
| Formation Time |
| Color |
| Surface Texture |
Why “Removing Tartar at Home” is Not Effective for Existing Build-up
Once plaque undergoes mineralization and transforms into tartar, its physical and chemical properties change dramatically, making home removal virtually impossible. The calcified structure of tartar creates a bond strength that exceeds the mechanical force generated by conventional toothbrushes, dental floss, and over-the-counter oral care products.
Many individuals attempt to remove tartar using various home remedies and commercial products marketed for calculus removal. These approaches include abrasive toothpastes containing baking soda or charcoal, metal dental tools purchased online, ultrasonic toothbrushes, and acidic solutions like vinegar or lemon juice. Unfortunately, these methods prove ineffective and potentially harmful.
Abrasive substances and tools can damage tooth enamel, leading to increased sensitivity, microscopic scratches that harbor bacteria, and irreversible enamel loss. Acidic solutions may temporarily soften tartar deposits but simultaneously weaken tooth enamel through demineralization, increasing cavity risk and tooth sensitivity.
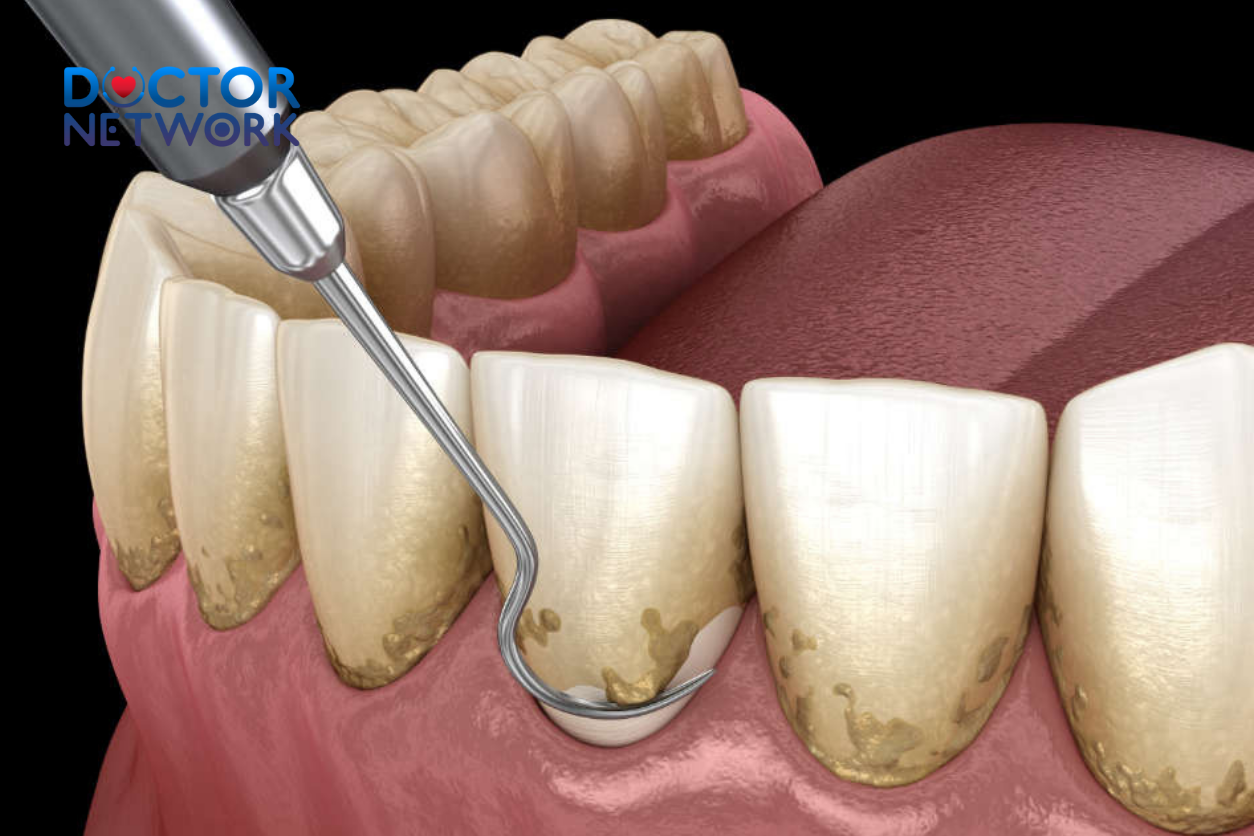
The fundamental issue with home tartar removal lies in the specialized nature of calculus deposits. Professional dental instruments, including ultrasonic scalers and hand instruments, are specifically designed to vibrate at precise frequencies or apply controlled pressure to fracture the crystalline structure of tartar without damaging underlying tooth enamel or gum tissues.
Additionally, complete tartar removal requires comprehensive access to all tooth surfaces, including areas below the gum line that are impossible to reach safely at home. Attempting to remove subgingival calculus without proper training and equipment can result in gum trauma, infection, and permanent tissue damage.
The adhesive strength of tartar to tooth enamel varies depending on the mineral content of your saliva, the duration of calculus formation, and the specific bacterial composition of the original plaque biofilm. Some individuals develop particularly tenacious tartar deposits that require specialized removal techniques and extended treatment sessions even in professional settings.
The Definitive Solution: Professional Dental Cleaning
Professional dental cleaning represents the only safe and effective method for removing established tartar deposits from tooth surfaces and root areas. This specialized treatment must be performed by licensed dental professionals, including dentists and registered dental hygienists, who possess the training, experience, and equipment necessary for complete calculus removal.
The professional tartar removal process, known as scaling, utilizes two primary instrument categories: ultrasonic scalers and hand instruments. Ultrasonic scalers employ high-frequency vibrations (typically 25,000-50,000 cycles per second) combined with water irrigation to fracture calculus deposits and flush away debris. These instruments prove particularly effective for removing large volumes of supragingival and accessible subgingival tartar.
Hand instruments, including curettes and scalers, provide precise control for removing remaining calculus deposits and smoothing root surfaces. These instruments allow dental professionals to access deep periodontal pockets and curved root surfaces that ultrasonic devices might miss.
For patients with significant subgingival tartar accumulation, root planing may be necessary following initial scaling procedures. Root planing involves smoothing rough root surfaces to remove bacterial toxins and create an environment conducive to gum tissue reattachment. This deep cleaning procedure often requires local anesthesia and may be completed over multiple appointments.
Professional cleaning offers several advantages beyond simple tartar removal:
- Complete Access: Dental professionals can safely reach all tooth surfaces, including areas below the gum line
- Tissue Safety: Proper technique prevents gum trauma and bleeding complications
- Comprehensive Assessment: Simultaneous evaluation for gum disease, cavities, and other oral health issues
- Customized Treatment: Tailored approach based on individual tartar patterns and gum health status
- Follow-up Care: Professional recommendations for maintaining results and preventing recurrence
The frequency of professional cleanings varies based on individual risk factors, tartar accumulation rates, and overall oral health status. Most dental professionals recommend cleanings every six months for patients with good oral hygiene and low tartar formation rates. Individuals with rapid calculus accumulation, gum disease history, or certain medical conditions may require more frequent professional interventions, typically every three to four months.
| Professional Cleaning Frequency Guidelines |
|---|
| Patient Category |
| Low Risk (Excellent oral hygiene) |
| Moderate Risk (Average oral hygiene) |
| High Risk (Poor hygiene, smoking, diabetes) |
| Periodontal Disease History |
| Orthodontic Treatment |
The REAL “How to Remove Tartar at Home”: Focus on PREVENTION!
Since removing existing tartar at home proves ineffective and potentially harmful, the most powerful home-based strategy focuses on preventing plaque mineralization through comprehensive oral hygiene practices. Effective plaque control interrupts the calcification process, maintaining the soft biofilm in a removable state.
Proper Brushing Technique and Frequency
Effective toothbrushing requires attention to technique, timing, and tool selection. The optimal brushing angle positions bristles at 45 degrees toward the gum line, allowing bristle tips to penetrate slightly into the gingival sulcus where plaque accumulates most readily. Use gentle, circular motions rather than aggressive back-and-forth scrubbing, which can damage gum tissues and tooth enamel.
Brush for a minimum of two minutes, twice daily, ensuring adequate attention to all tooth surfaces. Many individuals focus primarily on easily accessible front teeth while neglecting posterior molars and lingual (tongue-side) surfaces where tartar formation occurs most frequently. Consider using an electric toothbrush with a timer function to ensure consistent brushing duration and technique.
Select a soft-bristled toothbrush to minimize enamel abrasion and gum irritation. Replace toothbrushes every three to four months or when bristles become frayed, as worn bristles lose effectiveness in plaque removal.
Daily Flossing: The Essential Complement
Dental floss reaches interproximal areas and subgingival spaces that toothbrush bristles cannot access effectively. These areas represent prime locations for plaque accumulation and subsequent tartar formation. Daily flossing removes plaque deposits before mineralization occurs, preventing calculus development in these vulnerable areas.
Proper flossing technique involves using approximately 18 inches of floss, winding most around middle fingers while maintaining 1-2 inches of working floss between thumbs and forefingers. Gently guide floss between teeth using a sawing motion, then curve the floss around each tooth in a C-shape to clean below the gum line.
For individuals with difficulty using traditional floss, alternative interdental cleaning tools include floss picks, water flossers, and interdental brushes. While these tools provide some benefit, traditional floss remains the gold standard for thorough interproximal cleaning.
Fluoride Toothpaste and Antimicrobial Agents
Fluoride toothpaste strengthens tooth enamel through remineralization processes, making teeth more resistant to acid attacks from plaque bacteria. The fluoride ions integrate into enamel crystal structure, creating fluorapatite, which demonstrates greater resistance to demineralization than natural hydroxyapatite.
Some toothpastes contain additional anti-tartar ingredients, such as pyrophosphates or zinc compounds, which may help slow mineralization processes. However, these ingredients cannot remove existing tartar deposits and provide only modest benefits in preventing new calculus formation.
Antimicrobial mouthwashes containing ingredients like cetylpyridinium chloride or essential oils can reduce bacterial populations in areas difficult to reach with mechanical cleaning methods. Use mouthwash as a supplement to, not replacement for, thorough brushing and flossing.
Dietary Considerations for Plaque Control
Bacterial plaque thrives on fermentable carbohydrates, particularly sugars and starches that provide energy for acid-producing microorganisms. Limiting frequency of sugar and starch consumption reduces the substrate available for bacterial metabolism, decreasing acid production and plaque accumulation.
Consider the following dietary strategies:
- Limit Snacking Frequency: Multiple eating episodes throughout the day provide continuous fuel for plaque bacteria
- Choose Low-Cariogenic Foods: Fresh fruits, vegetables, nuts, and dairy products pose lower risks for plaque formation
- Rinse After Eating: Water rinsing helps remove food particles and dilute bacterial acids
- Chew Sugar-Free Gum: Stimulates saliva production, which naturally buffers acids and provides antibacterial compounds
Key Prevention Strategies:
- Brush twice daily with proper technique for 2 minutes minimum
- Floss daily to remove interproximal plaque
- Use fluoride toothpaste to strengthen enamel
- Consider antimicrobial mouthwash as adjunctive therapy
- Limit frequency of sugary and starchy food consumption
- Stay hydrated to maintain optimal saliva flow
- Schedule regular professional cleanings and checkups
The Risks of Ignoring Tartar: Why Removal is Crucial
Untreated tartar accumulation creates a cascade of oral health problems that extend far beyond cosmetic concerns. The rough, porous surface of calculus deposits provides an ideal environment for additional plaque accumulation, creating a self-perpetuating cycle of bacterial growth and mineralization that becomes increasingly difficult to interrupt.
Gum Inflammation and Gingivitis Development
Tartar deposits, particularly those located near or below the gum line, serve as constant irritants to gingival tissues. The bacterial toxins and metabolic byproducts associated with calculus trigger inflammatory responses in surrounding gum tissues, leading to gingivitis—the initial stage of periodontal disease.
Gingivitis manifests through several characteristic symptoms: gum tissues become red and swollen instead of the healthy pink color, bleeding occurs during brushing or flossing, gums may feel tender or painful, and breath odor becomes persistently unpleasant. While gingivitis represents a reversible condition when tartar is removed and proper oral hygiene is restored, untreated inflammation progresses to more serious periodontal conditions.
Progression to Periodontitis and Tooth Loss
When gingivitis remains untreated, the inflammatory process extends deeper into periodontal structures, affecting the periodontal ligament and alveolar bone that support teeth. This advanced condition, known as periodontitis, represents an irreversible form of gum disease with serious long-term consequences.
Periodontitis development involves bacterial penetration below the gum line, forming deep periodontal pockets filled with toxins and calculus deposits. The immune system’s response to persistent bacterial presence leads to destruction of connective tissues and bone resorption around tooth roots. This process results in gum recession, tooth mobility, and eventual tooth loss if intervention doesn’t occur.
Advanced periodontitis affects approximately 42% of adults over age 30 in the United States, making it a leading cause of tooth loss in adults. The condition often progresses silently, with patients unaware of significant tissue destruction until symptoms become severe.
Increased Cavity Risk and Enamel Damage
Tartar deposits make effective plaque removal nearly impossible, creating protected environments where cavity-causing bacteria flourish. The rough surface texture of calculus traps food particles and provides attachment sites for additional bacterial colonization. These bacterial communities produce acids continuously, creating localized acidic environments that promote enamel demineralization and cavity formation.
Cavities associated with tartar buildup often develop in areas that are difficult to clean, such as along the gum line, between teeth, and on root surfaces exposed by gum recession. These locations make cavity detection and treatment more challenging, often requiring more extensive restorative procedures.
Systemic Health Implications
Recent research has established connections between periodontal disease and various systemic health conditions. The chronic inflammation associated with untreated tartar and gum disease may contribute to cardiovascular disease, diabetes complications, respiratory infections, and adverse pregnancy outcomes.
The bacterial species present in periodontal pockets can enter the bloodstream through inflamed gum tissues, potentially affecting distant organ systems. While the exact mechanisms remain under investigation, the association between oral and systemic health underscores the importance of preventing tartar accumulation and maintaining optimal periodontal health.
Cosmetic and Social Consequences
Tartar deposits readily absorb stains from food, beverages, and tobacco products, creating unsightly discoloration that affects smile aesthetics. The yellow, brown, or black appearance of stained calculus can significantly impact self-confidence and social interactions.
Additionally, the bacterial activity associated with tartar produces volatile sulfur compounds that cause persistent bad breath (halitosis). This condition often persists despite regular brushing and mouthwash use because the source—bacterial colonies within calculus deposits—remains protected from mechanical and chemical cleaning methods.
| Consequences of Untreated Tartar |
|---|
| Condition |
| Gingivitis |
| Periodontitis |
| Cavities |
| Halitosis |
| Staining |
Recognizing Tartar: What to Look For
Early identification of tartar formation enables prompt professional intervention before extensive calculus accumulation occurs. Understanding the visual and tactile characteristics of tartar deposits helps individuals recognize when professional cleaning becomes necessary.
Visual Identification of Calculus Deposits
Tartar typically manifests as hard, crusty deposits with distinct coloration patterns that differ from natural tooth enamel. Supragingival calculus (above the gum line) commonly appears yellow to brown, with coloration intensity influenced by dietary habits, smoking status, and individual variations in saliva composition.
The most common locations for visible tartar accumulation include the lingual (tongue-side) surfaces of lower front teeth, buccal (cheek-side) surfaces of upper molars, and areas around orthodontic appliances or dental restorations. These locations correspond to salivary gland openings where mineral-rich saliva promotes rapid calcification of plaque deposits.
Subgingival tartar (below the gum line) often appears darker, ranging from dark brown to black due to blood products and different bacterial compositions in oxygen-poor environments. While subgingival calculus may not be visible during routine self-examination, its presence often correlates with gum inflammation, bleeding, and pocket formation.
Tactile Recognition and Texture Changes
Healthy tooth enamel feels smooth when explored with the tongue tip, while tartar-covered surfaces feel rough, bumpy, or irregular. This textural difference becomes particularly noticeable along the gum line where calculus deposits commonly accumulate.
Many individuals first notice tartar through tongue sensation rather than visual inspection. The rough texture creates an unpleasant feeling and may trap food particles more readily than smooth enamel surfaces. However, avoid using fingernails or other objects to explore suspicious areas, as this can damage gum tissues and introduce bacteria.
Warning Signs Indicating Professional Intervention
Several symptoms suggest the presence of significant tartar accumulation requiring professional attention:
Gum-Related Symptoms:
- Bleeding during brushing or flossing
- Persistent gum tenderness or soreness
- Gum recession exposing root surfaces
- Bad taste in mouth despite good oral hygiene
Tooth-Related Symptoms:
- Increased tooth sensitivity to temperature or pressure
- Rough texture when running tongue over tooth surfaces
- Visible discoloration that doesn’t improve with brushing
- Food trapping in areas that previously felt smooth
General Oral Health Indicators:
- Persistent bad breath despite regular oral hygiene
- Changes in bite or tooth alignment
- Loose or mobile teeth
- Pus or discharge around gum line
These symptoms often indicate that tartar accumulation has progressed beyond simple surface deposits and may involve subgingival calculus formation with associated periodontal inflammation.
Factors That Increase Your Risk of Tartar Build-up
Individual susceptibility to tartar formation varies significantly based on genetic, behavioral, medical, and environmental factors. Understanding personal risk factors enables targeted prevention strategies and appropriate professional care frequency.
Oral Hygiene Habits and Technique Quality
Inadequate or improper oral hygiene represents the most significant modifiable risk factor for tartar development. Many individuals believe they maintain good oral hygiene while actually missing critical areas where plaque accumulates most readily.
Common oral hygiene deficiencies include:
- Insufficient brushing duration (less than 2 minutes)
- Infrequent brushing (less than twice daily)
- Poor brushing technique missing gum line areas
- Inconsistent or absent flossing habits
- Failure to clean posterior teeth thoroughly
- Using worn toothbrushes with ineffective bristles
Tobacco Use and Smoking Effects
Tobacco products significantly increase tartar formation rates through multiple mechanisms. Smoking reduces saliva production, eliminating saliva’s natural cleansing and buffering effects. Nicotine and other tobacco compounds also compromise immune system function, reducing the body’s ability to fight bacterial infections in gum tissues.
Smokeless tobacco products create additional risks by increasing bacterial growth and providing sugars that fuel plaque formation. The sticky residue from tobacco products also provides attachment sites for bacterial colonization and plaque accumulation.
Statistics indicate that smokers develop tartar deposits 2-3 times faster than non-smokers and experience more severe periodontal disease progression. Smoking cessation significantly improves oral health outcomes and reduces tartar formation rates within weeks of quitting.
Genetic Predisposition and Family History
Genetic factors influence several aspects of tartar susceptibility, including saliva composition, immune system responses, and bacterial colonization patterns. Some individuals inherit saliva with higher calcium and phosphate concentrations, promoting faster plaque mineralization despite excellent oral hygiene efforts.
Family history of early tooth loss, gum disease, or rapid tartar formation suggests genetic predisposition requiring more intensive prevention strategies. These individuals may benefit from more frequent professional cleanings and specialized oral care products.
Medical Conditions and Medications
Several systemic conditions and medications affect oral health and tartar formation rates:
Medical Conditions:
- Diabetes: Elevated blood glucose levels promote bacterial growth and impair immune responses
- Sjögren’s syndrome: Autoimmune condition causing dry mouth and reduced saliva production
- HIV/AIDS: Immune system compromise increases infection susceptibility
- Kidney disease: Altered mineral metabolism affects saliva composition
Medications with Oral Effects:
- Antidepressants and antihistamines: Reduce saliva production
- Blood pressure medications: Many cause dry mouth side effects
- Anticonvulsants: Can cause gum overgrowth that traps plaque
- Chemotherapy drugs: Suppress immune function and alter oral tissues
Age-Related Changes
Aging affects multiple factors related to tartar formation. Saliva production naturally decreases with age, reducing the mouth’s natural cleansing mechanisms. Medications required for age-related health conditions often compound this problem.
Motor skill changes associated with aging may impact oral hygiene effectiveness, making thorough plaque removal more challenging. Arthritis in hands and wrists can make proper brushing and flossing techniques difficult to maintain.
Gum recession commonly occurs with aging, exposing root surfaces that accumulate tartar more readily than enamel surfaces. These areas also prove more difficult to clean effectively with standard oral hygiene tools.
Risk Factor Assessment Table:
| Risk Level | Primary Factors | Professional Cleaning Frequency |
|---|---|---|
| Low Risk | Excellent oral hygiene, no medical conditions, non-smoker | Every 6 months |
| Moderate Risk | Average oral hygiene, controlled medical conditions | Every 4-6 months |
| High Risk | Poor oral hygiene, smoking, uncontrolled diabetes | Every 3-4 months |
| Very High Risk | Multiple risk factors, history of periodontal disease | Every 3 months |
Conclusion – How to Remove Tartar from Teeth

Effective tartar management requires understanding a fundamental principle: existing calculus deposits cannot be safely or completely removed through home methods, making professional dental cleaning essential for established tartar elimination. The crystalline structure and strong adhesion of mineralized plaque necessitate specialized instruments and professional expertise that home care cannot replicate.
The most powerful weapon against tartar lies not in removal techniques, but in prevention through meticulous plaque control. Daily brushing with proper technique, consistent interdental cleaning through flossing, and strategic use of fluoride products can prevent plaque mineralization before tartar formation occurs. This prevention-focused approach proves far more effective and economical than attempting to address advanced calculus accumulation.
Regular professional dental visits serve dual purposes in tartar management: removing established deposits that home care cannot eliminate and providing personalized guidance for optimizing prevention strategies. The frequency of these visits should reflect individual risk factors, with high-risk patients requiring more frequent interventions to maintain optimal oral health.
The consequences of ignoring tartar extend far beyond cosmetic concerns, encompassing serious oral health conditions like gingivitis, periodontitis, and increased cavity risk. The potential connections between periodontal disease and systemic health conditions underscore the importance of maintaining excellent oral hygiene and seeking prompt professional care when tartar accumulation occurs.
Success in tartar control depends on recognizing that oral health represents a lifelong commitment requiring consistent daily care, regular professional monitoring, and prompt intervention when problems arise. By understanding the science behind tartar formation, implementing evidence-based prevention strategies, and maintaining regular professional care relationships, individuals can achieve and maintain optimal oral health throughout their lives.
Remember that your oral health professional serves as your partner in tartar management, providing not only treatment services but also personalized recommendations based on your unique risk factors and oral health status. Open communication about your concerns, challenges, and goals enables the development of tailored strategies that fit your lifestyle while maximizing prevention effectiveness.
The investment in proper tartar management—both through daily home care and regular professional cleaning—pays dividends in maintained oral health, preserved natural teeth, enhanced quality of life, and potentially reduced risks for systemic health complications. Take action today to establish or improve your tartar control routine, and consult with dental professionals to develop a personalized plan that addresses your specific needs and risk factors.
5 frequently asked questions
1. What is tartar and why should it be removed?
Tartar, also called dental calculus, is hardened plaque formed when minerals in saliva combine with soft plaque on teeth. It creates a rough surface that harbors bacteria, leading to gum disease, tooth decay, and bad breath. Removing tartar is essential to maintain oral health and prevent serious dental problems.
2. Can I remove tartar from my teeth at home?
Once plaque hardens into tartar, it cannot be effectively removed by regular brushing or flossing alone. While good oral hygiene and some home remedies (like baking soda brushing or vinegar rinses) may help reduce plaque and slow tartar buildup, professional dental cleaning is required to safely and thoroughly remove tartar deposits.
3. What are the best home care steps to prevent tartar buildup?
Brush twice daily with fluoride toothpaste using a soft-bristle brush and proper technique (45-degree angle, gentle strokes).
Floss daily to remove debris between teeth.
Use tartar-control toothpaste containing ingredients that inhibit tartar formation.
Rinse with antibacterial mouthwash after brushing.
Avoid sugary and starchy foods that feed bacteria.
Drink water after meals to wash away food particles.
Chew sugar-free gum to stimulate saliva flow, which naturally cleanses teeth.
4. How do dentists remove tartar professionally?
Dentists or hygienists use specialized tools and techniques:
Scaling: Ultrasonic instruments break and remove tartar from tooth surfaces and below the gumline.
Hand instruments: Fine tools remove remaining deposits and smooth the teeth.
Polishing: Teeth are polished to remove surface stains and make it harder for new tartar to form.
Fluoride treatment: Sometimes applied to strengthen enamel and protect teeth after cleaning.
5. How often should I get professional tartar removal?
It is generally recommended to have professional dental cleanings, including tartar removal, at least twice a year (every six months). People prone to tartar buildup or gum disease may need more frequent visits. Regular cleanings help keep teeth healthy and prevent complications.
References
1. Effective Toothbrushing:
* Technique & Frequency: Brush at least twice a day for two minutes each time, using a soft-bristled toothbrush and fluoride toothpaste. Focus on cleaning all tooth surfaces, especially along the gumline.
* Evidence: Numerous studies and systematic reviews support the effectiveness of toothbrushing for plaque removal.
* Study Example (Cochrane Review):
* Title: “Powered versus manual toothbrushing for oral health.”
* Authors: Deacon, S. A., Glenny, A. M., Deery, C., Robinson, P. G., Heanue, M., Walmsley, A. D., & Shaw, W. C.
* Source: Cochrane Database of Systematic Reviews, 2010. (Note: Cochrane reviews are updated; newer versions may exist).
* Key Finding: Powered toothbrushes show a statistically significant benefit in plaque and gingivitis reduction compared to manual brushes.
* Link: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002281.pub2/full
* DOI: 10.1002/14651858.CD002281.pub2
2. Interdental Cleaning (Flossing, Interdental Brushes):
* Purpose: Cleans between teeth and under the gumline where a toothbrush cannot reach. Do this at least once a day.
* Evidence: Essential for removing interproximal plaque.
* Study Example (Cochrane Review – already cited above for context):
* Title: “Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries.”
* Authors: Worthington, H. V., MacDonald, L., Poklepovic Pericic, T., et al.
* Source: Cochrane Database of Systematic Reviews, 2019.
* Key Finding: Interdental cleaning in addition to toothbrushing may reduce gingivitis and plaque.
* Link: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012018.pub2/full
* DOI: 10.1002/14651858.CD012018.pub2
3. Tartar-Control Toothpastes:
* Mechanism: These toothpastes do not remove existing tartar. They contain ingredients (like pyrophosphates or zinc citrate) that help prevent new plaque from mineralizing into tartar on the tooth surface.
* Evidence: Studies show they can reduce the formation of new supragingival calculus.
* Study Example (Review):
* Title: “Anti-calculus effect of a dentifrice containing pyrophosphate and sodium tripolyphosphate.”
* Authors: Baig, A., & He, T.
* Source: The Journal of Clinical Dentistry, 2005. (Many similar studies exist from various toothpaste manufacturers and independent researchers).
* Key Finding: Dentifrices with these agents show a reduction in calculus formation compared to regular fluoride toothpaste.
* Link (PubMed Abstract): https://pubmed.ncbi.nlm.nih.gov/15825479/
* (Note: This is one example; there are many proprietary studies. The overall mechanism is accepted.)
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.

























