Discover common root canal treatment side effects including nerve damage, infections & recovery tips. Complete medical guide with prevention strategies 2025.
Root Canal Treatment Side Effects: Complete Guide to Complications and Management
Root canal treatment side effects represent a critical concern for patients considering endodontic therapy, encompassing various temporary and permanent complications that affect approximately 5-10% of individuals undergoing this widely performed dental procedure. While root canal therapy demonstrates a 95% success rate in preserving infected or damaged teeth, comprehending root canal treatment side effects, potential adverse reactions, and evidence-based management strategies remains essential for informed patient decisions and optimal therapeutic outcomes.
This comprehensive medical guide examines the complete spectrum of root canal treatment side effects, from immediate post-operative symptoms to rare but serious long-term complications. We’ll analyze common root canal treatment side effects including pain, swelling, and temporary sensitivity, alongside less frequent adverse events such as instrument fracture, perforation, and endodontic flare-ups. Furthermore, this article addresses contraindications, risk factors, prevention strategies, and evidence-based management protocols that both dental professionals and patients must understand when considering root canal treatment side effects and their implications.
Understanding Root Canal Treatment Side Effects and Associated Risks
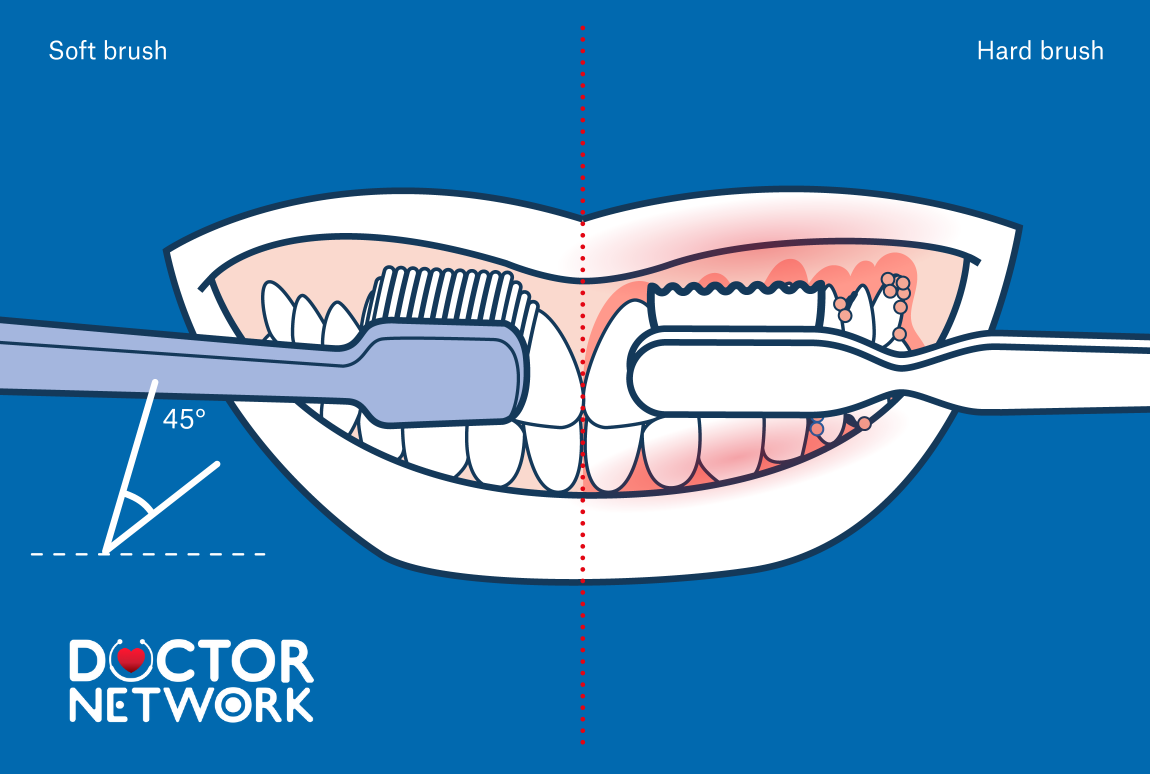
Root Canal look likes
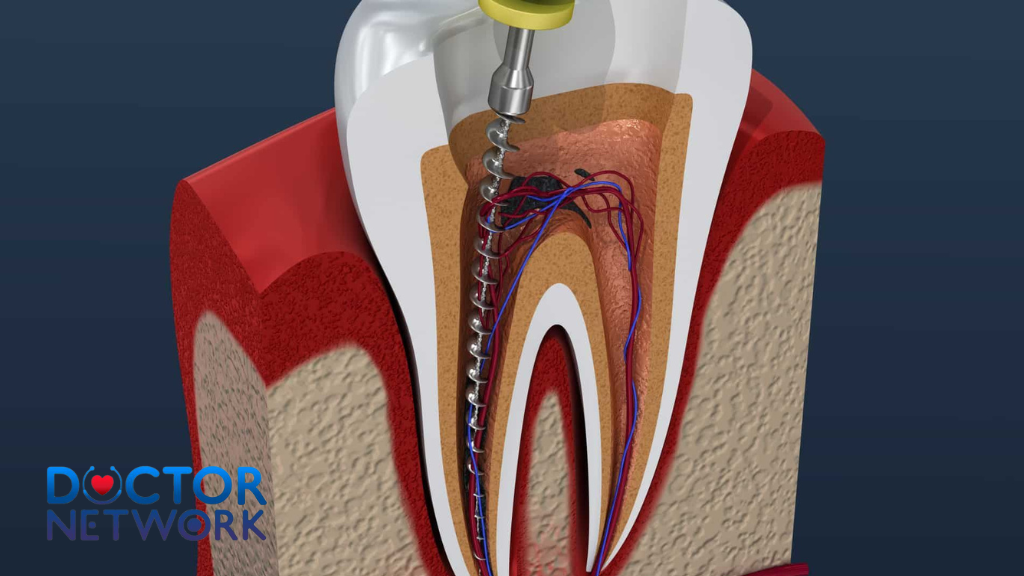
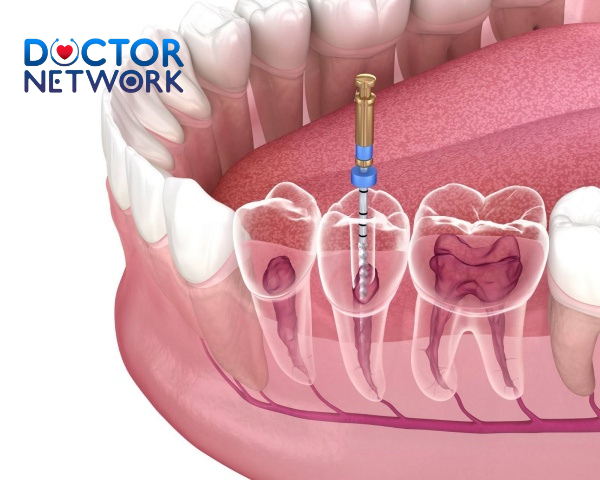
Root canal treatment side effects develop from the complex nature of endodontic procedures, which involve removing infected pulp tissue, cleaning root canals, and sealing the tooth structure to prevent reinfection. The inflammatory response triggered by instrumentation, irrigation solutions, and obturation materials frequently produces various root canal treatment side effects ranging from mild discomfort to severe complications requiring emergency intervention.
Root canal treatment side effects typically manifest in three distinct phases: intraoperative events occurring during treatment, immediate post-operative reactions within 24-48 hours, and delayed complications emerging weeks to months after therapy completion. Understanding this temporal pattern of root canal treatment side effects helps clinicians anticipate potential issues and implement appropriate preventive measures.
The severity and frequency of root canal treatment side effects correlate with multiple factors including tooth location, extent of pre-existing infection, patient immune status, operator experience, and treatment complexity. Anterior teeth generally present fewer root canal treatment side effects compared to posterior molars due to simpler root anatomy and improved access for thorough debridement.
Common Immediate Root Canal Treatment Side Effects
Post-Operative Pain and Discomfort
Post-endodontic pain stands as the most frequently reported root canal treatment side effect, affecting 30-60% of patients within the first 72 hours following endodontic therapy. This discomfort typically ranges from mild sensitivity to moderate throbbing pain, reflecting the inflammatory response to mechanical instrumentation and chemical irrigation of periapical tissues.
The intensity of post-operative pain varies significantly based on pre-treatment symptoms, with previously symptomatic teeth generally producing more pronounced discomfort than asymptomatic cases. Necrotic pulps with extensive periapical pathology often generate more severe inflammatory reactions due to bacterial toxin release and tissue trauma during debridement procedures.
Pain management protocols typically involve non-steroidal anti-inflammatory drugs (NSAIDs) as first-line therapy, with ibuprofen 600-800mg every 6-8 hours providing optimal anti-inflammatory and analgesic effects. Acetaminophen can be added for enhanced pain control, while opioid medications are reserved for severe cases requiring additional intervention.
Swelling and Facial Edema
Root canal treatment side effects frequently include facial swelling occurring in approximately 10-15% of patients, typically developing 12-24 hours post-treatment and reaching peak intensity within 48-72 hours. This inflammatory response results from tissue trauma, bacterial endotoxin release, and immune system activation in response to treatment procedures.
The anatomical location of swelling depends on the treated tooth, with maxillary posterior teeth potentially causing cheek and periorbital edema, while mandibular molars may produce submandibular and neck swelling. Severe cases can compromise airway patency, particularly when involving mandibular posterior teeth with associated Ludwig’s angina development.
Management strategies include cold compress application during the first 24 hours, followed by warm compresses to promote resolution. Corticosteroids may be prescribed for severe cases, while antibiotics are indicated when swelling accompanies signs of spreading infection or systemic involvement.
Temporary Tooth Sensitivity
Heightened tooth sensitivity frequently follows root canal treatment, manifesting as sharp pain responses to temperature changes, pressure, or percussion. This hypersensitivity typically resolves within 2-4 weeks as periapical tissues heal and inflammation subsides.
Thermal sensitivity may persist longer in cases involving incomplete debridement, residual vital tissue, or overfilled root canals extending beyond the apex. Mechanical sensitivity often correlates with high restoration contacts requiring occlusal adjustment to reduce traumatic forces during function.
Desensitizing toothpastes containing potassium nitrate or fluoride compounds can provide symptomatic relief, while persistent sensitivity may indicate treatment failure requiring retreatment or surgical intervention.
Moderate to Severe Root Canal Treatment Side Effects
You should have a root canal when the soft tissue (dental pulp) is infected or inflamed, causing pain, swollen gums, etc.
Endodontic Flare-Ups
Endodontic flare-ups represent serious root canal treatment side effects involving acute exacerbations of periapical pathology occurring during or immediately after endodontic therapy, affecting 2-5% of patients and characterized by severe pain, swelling, and potential systemic symptoms. These root canal treatment side effects typically develop when bacterial irritants or debris are extruded beyond the root apex during instrumentation.
Predisposing factors include pre-existing acute apical periodontitis, inadequate access cavity preparation, aggressive instrumentation techniques, and incomplete canal debridement. Patients with compromised immune systems, diabetes mellitus, or other systemic conditions face increased risks for flare-up development.
Management requires immediate intervention including drainage establishment, copious irrigation, medicament placement, and systemic antibiotic therapy when indicated. NSAIDs provide anti-inflammatory benefits, while corticosteroids may be necessary for severe cases involving significant facial swelling or trismus.
Instrument Separation and Retrieval Challenges
Endodontic instrument fracture occurs in approximately 2-6% of root canal procedures, with separated instruments potentially blocking complete canal preparation and obturation. Nickel-titanium rotary instruments show higher fracture rates compared to stainless steel hand files, particularly in severely curved or calcified canals.
The clinical significance of retained instrument fragments depends on their location, size, and associated bacterial contamination. Fragments in the apical third often require surgical removal or may be bypassed with careful technique, while coronal fragments typically necessitate retrieval for successful treatment completion.
Ultrasonic techniques, specialized retrieval systems, and microsurgical approaches provide options for instrument removal, though success rates vary based on fragment characteristics and canal anatomy. In some cases, retained instruments can be incorporated into the root filling without compromising treatment success.
Perforation and Anatomical Complications
Root perforations represent serious procedural complications occurring in 1-3% of endodontic cases, involving unintended communication between the root canal system and surrounding periodontal tissues. These iatrogenic defects can compromise treatment prognosis and may require complex repair procedures or tooth extraction.
Lateral perforations typically occur during post space preparation or aggressive canal instrumentation, while apical perforations result from overzealous apex preparation or loss of working length control. Strip perforations commonly affect mesial roots of mandibular molars due to excessive dentin removal during canal shaping.
Immediate recognition and management are crucial for optimal outcomes, with mineral trioxide aggregate (MTA) representing the gold standard for perforation repair due to its biocompatibility and sealing properties. Delayed treatment often results in bacterial contamination and inflammatory root resorption, significantly compromising long-term prognosis.
Rare but Serious Root Canal Treatment Side Effects
Nerve Damage and Paresthesia
Inferior alveolar nerve injury represents one of the most concerning root canal treatment side effects, though rare, potentially causing permanent complications following mandibular endodontic procedures. This neurological damage can result in temporary or permanent numbness, tingling, or altered sensation in the lower lip, chin, and tongue, making it among the most feared root canal treatment side effects by patients.
The incidence of nerve damage among root canal treatment side effects remains extremely low (less than 0.1%), but risk factors include anatomical variations, excessive instrumentation beyond the apex, and cytotoxic irrigant extrusion. Hypochlorite accidents involving sodium hypochlorite injection beyond the root apex represent severe root canal treatment side effects causing immediate intense pain, tissue necrosis, and potential permanent nerve damage.
Early recognition and immediate management are essential for minimizing permanent sequelae. Treatment protocols include copious saline irrigation, corticosteroid administration, and prompt referral to oral and maxillofacial surgery specialists for comprehensive evaluation and potential nerve repair procedures.
Sinus Complications and Communication
Maxillary posterior root canal treatment can occasionally result in sinus complications due to the close anatomical relationship between root apices and the maxillary sinus floor. Inadvertent sinus perforation may occur during aggressive apical preparation, while irrigant extrusion can cause acute sinusitis or tissue necrosis.
Oro-antral communication development represents a serious complication requiring immediate recognition and appropriate management to prevent chronic sinusitis or osteomyelitis. Symptoms may include unilateral nasal congestion, purulent discharge, facial pain, and a metallic taste associated with irrigant penetration into the sinus cavity.
Management strategies include antibiotic prophylaxis, decongestants, and in some cases, surgical closure of the communication. Prevention involves careful radiographic evaluation of root-to-sinus relationships and conservative instrumentation techniques when treating maxillary posterior teeth.
Table 1: Common Root Canal Side Effects and Their Frequency
| Side Effect | Frequency | Duration | Severity Level |
|---|---|---|---|
| Post-operative Pain | 30-60% | 2-7 days | Mild to Moderate |
| Tooth Sensitivity | 40-50% | 1-4 weeks | Mild |
| Facial Swelling | 10-15% | 3-5 days | Moderate |
| Endodontic Flare-up | 2-5% | 3-7 days | Severe |
| Instrument Fracture | 2-6% | N/A | Variable |
| Root Perforation | 1-3% | N/A | Severe |
| Nerve Damage | <0.1% | Variable | Severe |
Risk Factors and Patient Considerations
Pre-Existing Medical Conditions
Certain systemic conditions significantly influence the risk profile for root canal treatment complications, requiring careful evaluation and potential treatment modifications. Diabetes mellitus patients face increased risks for delayed healing, infection, and endodontic flare-ups due to compromised immune function and altered inflammatory responses.
Cardiovascular diseases, particularly those requiring anticoagulant therapy, may predispose patients to excessive bleeding during treatment and prolonged healing periods. Immunocompromised patients, including those receiving chemotherapy, organ transplant recipients, or individuals with HIV/AIDS, require special consideration due to increased infection risks and potential for severe complications.
Osteoporosis and bisphosphonate therapy present unique challenges, with potential risks for osteonecrosis of the jaw following invasive dental procedures. While routine endodontic treatment typically doesn’t require bisphosphonate discontinuation, careful risk-benefit analysis and coordination with treating physicians remain essential.
Anatomical Variations and Complexity Factors
Complex root canal anatomy significantly increases the likelihood of treatment complications and adverse outcomes. Teeth with multiple canals, severe curvatures, calcified chambers, or previous endodontic treatment present heightened challenges requiring advanced techniques and extended treatment times.
C-shaped root configurations commonly found in mandibular second molars create difficulties in complete debridement and obturation, potentially leading to persistent infection and treatment failure. Dens invaginatus, taurodontism, and other developmental anomalies require specialized approaches and may carry higher complication rates.
Radiographic evaluation using cone-beam computed tomography (CBCT) provides detailed anatomical information, allowing clinicians to anticipate potential challenges and modify treatment approaches accordingly. Three-dimensional imaging particularly benefits complex cases where conventional radiography proves inadequate for complete anatomical assessment.
Prevention Strategies for Root Canal Treatment Side Effects
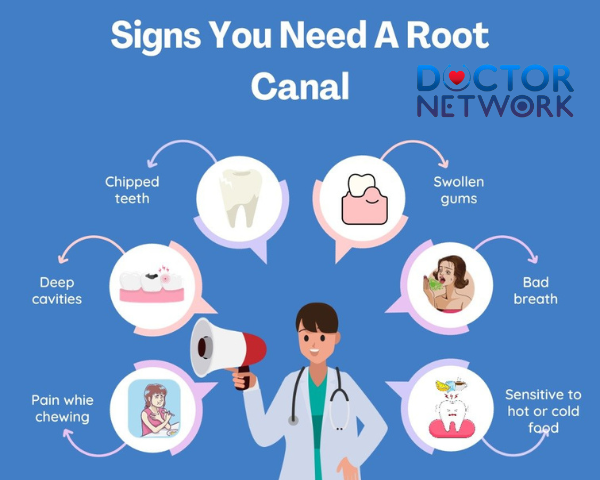
Signs You Need A Root Canal
Proper Patient Selection and Evaluation
Comprehensive pre-treatment evaluation represents the cornerstone of preventing root canal treatment side effects, involving thorough medical history review, clinical examination, and appropriate radiographic assessment. Patient selection criteria should consider tooth restorability, periodontal status, and overall treatment prognosis before initiating endodontic therapy to minimize potential root canal treatment side effects.
Informed consent procedures must clearly outline potential root canal treatment side effects, expected outcomes, and alternative treatment options including extraction and implant placement. Patients should understand the possibility of various root canal treatment side effects, treatment failure, need for retreatment, and potential complications requiring additional intervention.
Risk stratification based on clinical findings, anatomical complexity, and patient factors allows for appropriate treatment planning and referral to specialist when indicated. High-risk cases may benefit from endodontic specialist evaluation to optimize treatment outcomes and minimize complications.
Advanced Techniques and Technology
Modern endodontic techniques and technologies significantly reduce complication rates when properly implemented. Operating microscopes provide enhanced visualization for precise instrumentation and identification of anatomical variations, while rotary instrumentation systems offer improved efficiency and reduced procedural errors.
Electronic apex locators enhance working length determination accuracy, reducing risks of overinstrumentation and associated complications. Digital radiography provides immediate feedback and reduced radiation exposure compared to conventional film-based systems.
Ultrasonic irrigation activation improves debridement efficacy while minimizing extrusion risks, and thermoplasticized obturation techniques ensure superior seal quality compared to traditional cold lateral compaction methods.
Management of Root Canal Treatment Side Effects
Immediate Post-Operative Care
Proper post-operative instructions and pain management protocols significantly influence patient comfort and reduce the severity of root canal treatment side effects. Clear verbal and written instructions should address expected root canal treatment side effects, pain medication schedules, and emergency contact procedures for severe complications.
NSAIDs provide optimal anti-inflammatory effects and pain control for most patients, with ibuprofen 600-800mg every 6-8 hours representing first-line therapy. Acetaminophen can be added for enhanced analgesia, while prescription opioids are reserved for severe cases requiring additional intervention.
Ice application during the first 24 hours helps minimize swelling, followed by warm compresses to promote resolution and circulation. Patients should be advised to avoid chewing on the treated tooth until permanent restoration placement and to maintain excellent oral hygiene to prevent secondary infection.
When to Seek Emergency Care
Patients must understand warning signs of serious root canal treatment side effects requiring immediate professional attention, including severe uncontrolled pain, significant facial swelling, difficulty swallowing or breathing, and signs of systemic infection such as fever and malaise.
Progressive swelling extending beyond the immediate treatment area represents one of the more dangerous root canal treatment side effects, particularly when involving the neck or floor of mouth, potentially indicating serious complications requiring emergency intervention. Allergic reactions to medications or materials, though rare among root canal treatment side effects, necessitate immediate medical attention and possible hospitalization.
Persistent severe pain beyond the expected post-operative period may indicate incomplete treatment, missed canals, or other complications requiring prompt evaluation and possible retreatment or surgical intervention.
Table 2: Pain Management Protocol for Root Canal Side Effects
| Pain Level | Medication | Dosage | Duration | Additional Measures |
|---|---|---|---|---|
| Mild (1-3/10) | Ibuprofen | 400mg q6h | 2-3 days | Cold compress |
| Moderate (4-6/10) | Ibuprofen + Acetaminophen | 600mg + 650mg q6h | 3-5 days | Cold/warm compress |
| Severe (7-10/10) | Prescription opioid + NSAID | As prescribed | As needed | Emergency evaluation |
Long-Term Considerations
Success Rates and Prognosis
Root canal treatment demonstrates excellent long-term success rates, with studies reporting 85-95% success at 5-10 year follow-up periods when performed according to current standards of care. Success rates correlate with multiple factors including pre-treatment pulpal and periapical status, quality of coronal restoration, and patient compliance with follow-up care.
Teeth with vital pulps generally show higher success rates compared to necrotic cases with periapical pathology, while retreatment cases demonstrate lower success rates due to increased complexity and potential anatomical challenges. Quality of coronal seal significantly influences long-term outcomes, with delayed restoration placement associated with increased failure rates.
Regular follow-up examinations allow for early detection of potential complications and assessment of healing progress. Radiographic evaluation at 6-month and annual intervals provides objective assessment of periapical healing and treatment success.
Factors Affecting Treatment Outcomes
Multiple variables influence endodontic treatment outcomes beyond the technical aspects of canal preparation and obturation. Patient age affects healing capacity, with younger patients generally demonstrating better healing responses and higher success rates compared to elderly individuals.
Systemic health status plays a crucial role in treatment outcomes, with well-controlled diabetic patients showing comparable success rates to healthy individuals, while uncontrolled diabetes significantly compromises healing and increases failure rates. Smoking substantially reduces treatment success through impaired circulation and delayed healing responses.
The quality and timing of coronal restoration critically affects long-term prognosis, with immediate temporary restoration providing better outcomes than delayed restoration placement. Full coverage crowns generally provide superior protection compared to large composite restorations, particularly for posterior teeth subjected to heavy occlusal forces.
Alternative Treatment Options
When Root Canal Treatment May Not Be Appropriate
Certain clinical situations may contraindicate root canal treatment in favor of alternative approaches, including extraction and implant placement or bridge construction. Teeth with extensive crown destruction, vertical root fractures, or severe periodontal involvement may demonstrate poor long-term prognosis despite successful endodontic therapy.
Economic considerations and patient preferences may influence treatment decisions, with implant therapy potentially offering superior long-term outcomes in specific cases. Young patients with developing roots may benefit from vital pulp therapy procedures rather than conventional root canal treatment when pulp exposure is minimal.
Systemic health factors, including severe immunocompromise or inability to maintain oral hygiene, may favor extraction over complex endodontic treatment requiring extended healing periods and multiple appointments.
Comparative Risk Analysis
Implant placement presents different risk profiles compared to endodontic treatment, with surgical complications including nerve damage, sinus perforation, and implant failure requiring consideration. However, successful implants typically demonstrate predictable long-term outcomes without risks of endodontic failure or retreatment needs.
Extraction and bridge construction avoid endodontic complications but require preparation of adjacent healthy teeth, potentially compromising their long-term prognosis. Removable partial dentures present the lowest initial risk but may affect function, esthetics, and oral health through increased plaque accumulation and bone resorption.
Cost-benefit analysis should consider not only immediate treatment expenses but also long-term maintenance requirements, potential complications, and replacement needs over the patient’s lifetime.
List of Key Prevention Strategies:
- Comprehensive Pre-treatment Evaluation
- Thorough medical history review
- Complete radiographic assessment
- Pulp vitality testing
- Periodontal evaluation
- Proper Treatment Planning
- Anatomical complexity assessment
- Risk factor identification
- Alternative treatment consideration
- Specialist referral when indicated
- Advanced Clinical Techniques
- Operating microscopy utilization
- Electronic apex locator use
- Gentle instrumentation protocols
- Optimal irrigation procedures
- Post-operative Care Excellence
- Clear patient instructions
- Appropriate pain management
- Follow-up appointment scheduling
- Emergency contact provision
Patient Education and Communication
Setting Realistic Expectations
Effective patient communication begins with establishing realistic expectations regarding treatment duration, discomfort levels, and potential complications. Patients should understand that some post-operative discomfort is normal and expected, while severe pain or swelling requires immediate attention.
The multi-appointment nature of complex cases should be explained, along with the importance of completing treatment in a timely manner to prevent bacterial recontamination. Patients must understand their role in treatment success through compliance with instructions and attendance at scheduled appointments.
Financial considerations and insurance coverage should be discussed openly, including potential costs for complications or retreatment if initial therapy fails. Alternative treatment options should be presented objectively, allowing patients to make informed decisions based on their individual circumstances and preferences.
Documentation and Informed Consent
Comprehensive documentation serves both clinical and legal purposes, providing detailed records of treatment decisions, complications encountered, and patient responses to therapy. Pre-treatment photographs and radiographs establish baseline conditions, while progress notes document healing and complications.
Informed consent procedures must cover potential risks specific to the patient’s case, including anatomical challenges, medical history considerations, and alternative treatment options. Patients should acknowledge understanding of potential complications and their management.
Emergency contact procedures and after-hours care arrangements should be clearly documented and provided to patients, ensuring appropriate care access when complications arise outside normal business hours.
Table 3: Root Canal Success Factors and Their Impact
| Factor | Impact on Success | Preventive Measure | Success Rate Improvement |
|---|---|---|---|
| Pre-treatment Status | High | Proper diagnosis | 15-20% |
| Anatomical Complexity | Moderate | CBCT imaging | 10-15% |
| Operator Experience | High | Specialist referral | 20-25% |
| Coronal Seal Quality | Very High | Immediate restoration | 25-30% |
| Patient Compliance | Moderate | Clear instructions | 10-15% |
Research and Future Developments
Emerging Technologies
Regenerative endodontic procedures represent promising alternatives to traditional root canal treatment, particularly for immature teeth with necrotic pulps. These biological approaches aim to restore pulp vitality and promote continued root development through tissue engineering principles and growth factor application.
Laser-assisted endodontic therapy shows potential for improved disinfection and reduced post-operative complications through selective bacterial elimination and enhanced healing responses. However, current evidence remains limited regarding significant clinical advantages over conventional treatment methods.
Advanced imaging technologies, including optical coherence tomography and micro-computed tomography, provide unprecedented visualization of root canal anatomy and treatment outcomes, potentially improving treatment success rates and reducing complications.
Evidence-Based Practice Evolution
Current research focuses on optimizing treatment protocols through systematic reviews and meta-analyses of clinical outcomes. Large-scale longitudinal studies provide valuable data regarding long-term success rates and factors influencing treatment outcomes.
Microbiological research continues to identify new bacterial species and resistance patterns, leading to improved irrigation protocols and antibiotic selection strategies. Understanding of biofilm formation and elimination guides development of enhanced disinfection techniques.
Pain management research explores novel approaches including pharmacogenomics-based medication selection and alternative analgesic strategies to minimize post-operative discomfort while reducing opioid dependence risks.
Conclusion and Key Takeaways
Root canal treatment side effects encompass a comprehensive spectrum of complications ranging from common, mild post-operative discomfort to rare but serious neurological damage or sinus involvement. Understanding these potential root canal treatment side effects, their frequency, and appropriate management strategies enables both dental professionals and patients to make informed treatment decisions and optimize outcomes while minimizing adverse effects.
The vast majority of endodontic procedures proceed without significant root canal treatment side effects, with modern techniques and technologies contributing to high success rates and improved patient comfort. However, proper patient selection, thorough pre-treatment evaluation, and adherence to established protocols remain essential for minimizing root canal treatment side effects and managing complications when they occur.
Effective communication between dental professionals and patients, including comprehensive informed consent regarding potential root canal treatment side effects and realistic expectation setting, forms the foundation of successful endodontic treatment. Patients equipped with accurate information about potential root canal treatment side effects and their management are better prepared to navigate the treatment process and achieve optimal outcomes with minimal complications.
Prevention strategies, including advanced diagnostic techniques, specialized instrumentation, and evidence-based protocols, continue to evolve and improve treatment safety while reducing root canal treatment side effects. When complications do arise, prompt recognition and appropriate management typically result in successful resolution without long-term sequelae.
Future developments in regenerative endodontics, laser therapy, and advanced imaging technologies promise to further reduce root canal treatment side effects and improve treatment outcomes. However, the fundamental principles of thorough evaluation, careful technique, and comprehensive patient care remain the cornerstones of successful endodontic treatment with minimal root canal treatment side effects.
Frequently asked About “Root Canal Treatment Side Effects”
1. Is pain normal after a root canal treatment?
Yes, mild pain and discomfort are common for a few days following the procedure due to inflammation of the surrounding tissues. This pain usually subsides with time and can be managed with over-the-counter pain relievers such as ibuprofen. Severe or prolonged pain is uncommon and should be evaluated by a dentist.
2. Can a root canal cause infection or swelling?
While the goal of root canal treatment is to eliminate infection, there is a small risk of reinfection if bacteria remain or re-enter the tooth. Swelling around the treated area can occur but typically diminishes within a few days. If swelling worsens, spreads to the face or neck, or is accompanied by fever or pus, immediate dental care is necessary.
3. Will my tooth be sensitive to hot or cold after the treatment?
Temporary sensitivity to hot and cold is common after root canal therapy due to tissue inflammation, especially if there was pain or infection before the procedure. This sensitivity usually resolves within a few days without further treatment.
4. Can root canal treatment cause tooth discoloration?
Yes, discoloration of the treated tooth can occur, often due to internal bleeding or changes in the tooth’s structure after extensive infection or treatment. Cosmetic procedures such as teeth whitening or crowns can restore the tooth’s natural appearance if desired.
5. Are there any long-term side effects or risks?
Long-term side effects are rare but may include persistent pain, tooth fracture, or reinfection if the root canal filling or seal fails. Since the pulp is removed, the tooth can become more brittle, so dentists often recommend placing a crown to protect it. Persistent symptoms should be promptly evaluated by a dental professional.
References
https://kitchenerfamilydentist.com/blog/root-canal-treatment-the-10-most-frequently-asked-questions/
https://www.eastidahorootcanals.com/root-canal-treatment-side-effects-myths-vs-reality/
https://www.dezy.com/blogs/root-canal-treatment-side-effects-health-problems-and-risks
https://www.gentleteeth.com/root-canal-treatment-side-effects/
https://eastorangeendodontics.com/blog/root-canal-treatment-side-effects/
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.