The simple act of sipping through a straw becomes a critical concern following wisdom tooth extraction, as this seemingly innocent action can trigger dry socket—a painful complication that affects over 5% of wisdom teeth removal patients. Wisdom teeth extraction ranks among the most frequently performed oral surgical procedures, with millions of Americans undergoing this treatment annually to address impacted molars, overcrowding, or infection prevention. Understanding proper post-operative care protocols significantly influences your recovery trajectory, comfort level, and healing timeline.
“When can i use a straw after wisdom teeth removal?” – The primary concern surrounding straw usage centers on alveolar osteitis, commonly known as dry socket, which occurs when protective blood clots become dislodged from extraction sites. This comprehensive guide examines the scientific rationale behind straw restrictions, establishes evidence-based timelines for safe reintroduction, explores effective hydration alternatives, and provides detailed post-operative care instructions. We’ll also address potential complications, individual risk factors, and professional recommendations to ensure optimal healing outcomes following your oral surgery procedure.
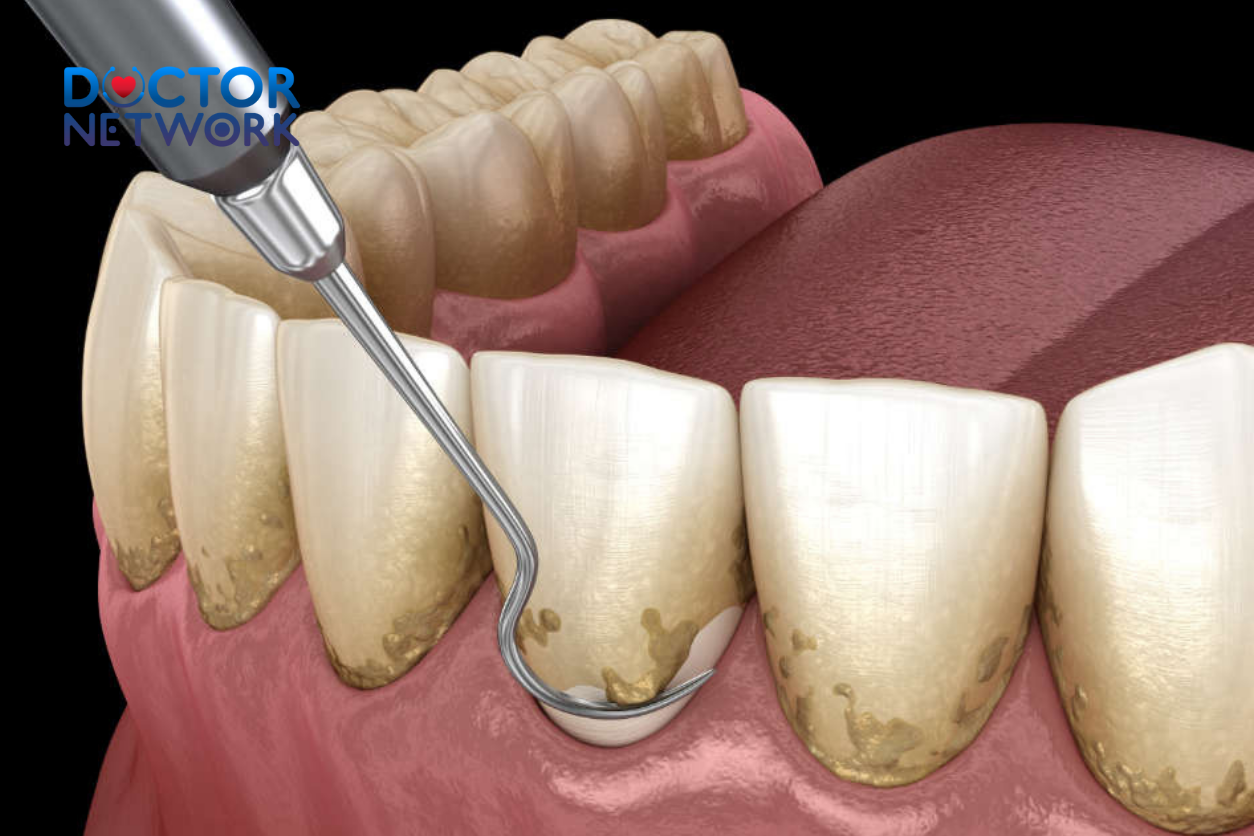
Understanding the Risks: Why Avoid Straws Initially?
Immediate post-extraction healing depends entirely on blood clot formation at surgical sites, creating nature’s protective barrier over exposed bone and nerve endings. This coagulation process begins within minutes of tooth removal, forming a fibrin mesh that shields underlying tissues from bacterial invasion, food debris, and physical trauma. The blood clot serves multiple critical functions: protecting sensitive alveolar bone, providing scaffolding for new tissue growth, and preventing infection at the extraction socket.
Straw usage creates negative pressure within the oral cavity through suction mechanics, generating forces that can dislodge these vital blood clots. The vacuum effect produced during sipping mimics the same mechanism that causes complications with spitting, vigorous rinsing, or smoking—all activities that oral surgeons strictly prohibit during initial healing phases.
Dry Socket (Alveolar Osteitis): The Primary Complication
Dry socket represents the most significant risk associated with premature straw usage, occurring when blood clots dissolve prematurely or become mechanically displaced from extraction sites. This condition exposes underlying alveolar bone and nerve endings, creating excruciating pain that often radiates to the temporal region, ear canal, and neck area. Unlike typical post-surgical discomfort, dry socket pain intensifies rather than diminishes over time, typically manifesting 3-5 days post-operatively.
Statistical analysis reveals dry socket incidence rates exceeding 5% for wisdom teeth extractions, compared to less than 2% for routine tooth removals. Risk factors include female gender, oral contraceptive use, smoking habits, advanced age (over 30), and complex surgical extractions requiring bone removal or tooth sectioning.
Additional Complications from Early Straw Use
Beyond dry socket formation, premature straw usage can precipitate several other complications:
Persistent Bleeding: Suction forces can disrupt hemostasis (blood clotting), causing renewed hemorrhage from extraction sites. This bleeding may prove difficult to control and require emergency intervention.
Bacterial Infiltration: Compromised clot integrity creates pathways for oral bacteria to invade surgical sites, potentially leading to localized infections or systemic complications in immunocompromised patients.
Enhanced Inflammatory Response: Mechanical disruption of healing tissues triggers increased inflammatory mediator release, resulting in prolonged swelling, enhanced pain sensation, and delayed recovery timelines.
Impaired Wound Healing: Disrupted blood supply and cellular matrix formation significantly compromise the body’s natural repair mechanisms, potentially doubling recovery duration.

Establishing the Timeline: When is it Safe to Sip?
Most oral surgeons recommend avoiding straw usage for a minimum of one week following wisdom teeth removal, though individual healing patterns and surgical complexity may necessitate longer restriction periods. This timeline reflects the natural progression of wound healing phases and decreasing dry socket risk over time.
Detailed Recovery Timeline
| Time Period | Straw Safety | Key Considerations |
|---|---|---|
| 0-48 Hours | AVOID COMPLETELY | Blood clot formation critical; highest complication risk |
| Days 3-5 | CONTINUE AVOIDING | Peak dry socket risk period; clot remains fragile |
| Days 6-7 | CAUTIOUS CONSIDERATION | Consult surgeon before attempting; gradual risk reduction |
| Week 2 | LOW RISK | Most patients can safely resume with gentle technique |
| Week 3+ | NORMAL USE | Full healing typically achieved; standard activities resume |
Immediate Post-Operative Period (First 24-48 Hours)
Complete straw avoidance remains mandatory during this critical window when initial hemostasis occurs. Blood clot formation continues actively, and any suction pressure can catastrophically disrupt this process. Patients should also avoid vigorous mouth rinsing, spitting, or any activities creating oral pressure changes.
Days 3-5: Peak Risk Window
The dry socket risk reaches maximum levels during this timeframe, even as surface healing appears to progress normally. Blood clots remain mechanically fragile and biochemically unstable, making them particularly susceptible to dislodgement through suction forces.
First Week Milestone
After seven days, dry socket risk diminishes significantly as clot organization advances and initial epithelialization occurs. However, professional consultation remains advisable before resuming straw usage, particularly for complex extractions or patients with risk factors.
Individual Factors Affecting Timeline
Several patient-specific variables can extend the cautious period beyond standard recommendations:
- Surgical Complexity: Impacted wisdom teeth requiring bone removal or tooth sectioning typically necessitate longer healing periods
- Age Considerations: Patients over 30 years demonstrate slower healing rates and increased complication risks
- Smoking History: Tobacco use significantly impairs wound healing through vasoconstriction and reduced oxygen delivery
- Medical Conditions: Diabetes, autoimmune disorders, and certain medications can compromise healing capacity
- Hormonal Factors: Oral contraceptives and hormonal fluctuations affect coagulation mechanisms
Variation in Professional Recommendations
Different oral surgeons may establish slightly varying protocols based on their surgical techniques, patient populations, and clinical experience. Some practitioners advocate for 10-14 day restriction periods, particularly for complex cases or high-risk patients. Always prioritize your surgeon’s specific instructions over general guidelines, as they possess intimate knowledge of your particular surgical circumstances.
Hydration Alternatives: Staying Comfortable While Healing
Maintaining adequate fluid intake proves crucial for optimal healing, immune function, and medication effectiveness during recovery. Dehydration can exacerbate swelling, impair pain medication absorption, and compromise the body’s natural repair mechanisms.
Recommended Hydration Methods
Direct Cup Drinking: Use gentle sipping motions from cups or glasses, avoiding excessive head tilting that might create pressure changes. Choose vessels with comfortable rim shapes that don’t require lip pursing.
Spoon-Fed Hydration: This method provides controlled liquid delivery without suction pressure. Use tablespoons for measured intake, particularly effective for consuming broths, soups, or liquid medications.
Wide-Opening Bottles: Sports bottles or containers with large openings allow direct liquid access without creating vacuum effects. Avoid squeeze bottles that might generate pressure.
Hydrating Foods: Incorporate moisture-rich options including:
- Clear broths and vegetable soups (served warm, not hot)
- Fruit juices diluted with water
- Gelatin desserts and sugar-free alternatives
- Ice cream and frozen yogurt (without chunks or nuts)
- Fresh fruits like watermelon, oranges, and grapes
Irrigation Syringe Considerations
While primarily designed for wound cleaning beginning around day 5 post-operatively, some practitioners may recommend irrigation syringes for hydration in specific circumstances. These devices serve mainly for debris removal from extraction sites rather than primary fluid intake, though they can provide controlled liquid delivery when necessary.
Comprehensive Post-Operative Care (Beyond Straws)
Successful wisdom teeth recovery extends far beyond straw avoidance, encompassing dietary modifications, oral hygiene protocols, pain management strategies, and activity restrictions. Following comprehensive post-operative instructions significantly reduces complication rates and accelerates healing timelines.
Dietary Guidelines and Nutritional Considerations
Proper nutrition supports tissue repair, immune function, and overall recovery progress during the initial healing phases.
Recommended Foods by Healing Phase
| Days 1-3 | Days 4-7 | Week 2+ |
|---|---|---|
| Smoothies (no straw) | Soft pasta dishes | Gradually firm textures |
| Applesauce | Scrambled eggs | Tender meats |
| Yogurt (plain) | Mashed potatoes | Cooked vegetables |
| Pudding | Soft-cooked rice | Fresh fruits |
| Ice cream | Cottage cheese | Normal diet resumption |
Foods to Avoid
First Two Weeks: Eliminate hard, crunchy, or sticky items that could become impacted in extraction sites:
- Popcorn, nuts, and seeds
- Potato chips and crackers
- Chewy candies or gum
- Raw vegetables and tough meats
- Spicy or acidic foods that might irritate wounds
Temperature Considerations: Avoid extremely hot beverages or foods that could increase bleeding or discomfort. Room temperature or cool items often provide optimal comfort during initial healing.
Oral Hygiene and Wound Care Protocols
Maintaining oral cleanliness while protecting extraction sites requires modified techniques and gentle approaches during the healing process.
Daily Hygiene Schedule
First 24 Hours: Complete mouth rinsing avoidance allows undisturbed clot formation. Gentle teeth brushing away from surgical sites remains acceptable using soft-bristled brushes.
Days 2-7: Begin warm salt water rinses (½ teaspoon salt in 8 ounces water) 2-3 times daily, especially after eating. Use gentle swishing motions rather than vigorous rinsing to avoid clot disruption.
Week 2+: Gradually resume normal oral hygiene practices, including careful cleaning around extraction sites as comfort permits.
Additional Oral Care Considerations
- Avoid alcohol-containing mouthwashes that can irritate healing tissues
- Use prescription mouth rinses if provided, typically starting 48 hours post-operatively
- Maintain gentle brushing techniques, gradually approaching extraction sites as healing progresses
- Avoid spitting forcefully; allow liquids to drain naturally from the mouth
Pain Management and Swelling Control
Effective discomfort management enhances patient comfort and supports the healing process through reduced stress responses and improved sleep quality.
Medication Protocols
Prescription Pain Relief: Follow prescribed opioid medications exactly as directed, understanding that complete pain elimination may not occur. Never exceed recommended dosages, and be aware of drowsiness effects that impair driving ability.
Over-the-Counter Options: Ibuprofen provides excellent anti-inflammatory effects for post-surgical swelling and discomfort. Acetaminophen offers additional pain relief and can be safely combined with ibuprofen under professional guidance.
Swelling Management Techniques
Cold Therapy: Apply ice packs or cold compresses to external cheek areas for 20-minute intervals during the first 48 hours. This vasoconstriction reduces inflammatory responses and numbs discomfort.
Head Elevation: Sleep with multiple pillows or in a recliner to maintain head elevation above heart level, promoting lymphatic drainage and reducing facial swelling.
Timeline Expectations: Swelling typically peaks 36-48 hours post-operatively and may persist for up to one week. Maximum facial edema usually occurs on day 2-3 before gradually subsiding.
Activity Restrictions and Physical Limitations
Physical exertion can increase blood pressure and heart rate, potentially disrupting clot formation and causing renewed bleeding from extraction sites.
Activity Guidelines by Recovery Phase
- First 24 Hours: Complete rest recommended; avoid any activities requiring mental alertness while under anesthesia effects
- Days 2-5: Light activities only; avoid exercise, heavy lifting, or anything elevating heart rate significantly
- Week 2: Gradual activity resumption as comfort permits; continue avoiding contact sports or high-intensity exercise
- Week 3+: Normal activity levels typically achievable for most patients
Suture Management
Surgical sites may require sutures for optimal healing and bleeding control, with different types requiring varying care approaches.
Dissolvable Sutures: These materials typically dissolve within 7-14 days without removal procedures. Avoid manipulating these sutures with your tongue or fingers.
Non-dissolvable Sutures: Require professional removal appointments, usually scheduled 7-10 days post-operatively. Maintain careful cleaning around suture sites without disturbing the materials.
Lifestyle Modifications During Recovery
Smoking and Tobacco Cessation: Complete tobacco avoidance for at least one week proves essential, as nicotine significantly impairs wound healing through vasoconstriction and reduced oxygen delivery to tissues.
Alcohol Restrictions: Avoid alcoholic beverages for at least 24 hours post-anesthesia, as alcohol can interact with pain medications and impair healing processes.
Nasal Care: Avoid forceful nose blowing for one week following upper wisdom teeth removal, as this can create pressure changes affecting extraction sites.
Recognizing and Managing Potential Complications
Early complication recognition enables prompt intervention and prevents serious sequelae that could compromise healing outcomes or require emergency treatment.
Warning Signs Requiring Professional Contact
Immediate dental consultation becomes necessary when experiencing any of the following symptoms:
Pain-Related Concerns
- Severe pain uncontrolled by prescribed medications
- Pain that worsens rather than improves after day 3
- Throbbing or sharp pain radiating to the ear (potential dry socket)
- New pain developing several days after initial improvement
Bleeding Complications
- Heavy bleeding persisting beyond 60 minutes despite gauze pressure
- Bright red blood flow that soaks multiple gauze pads hourly
- Renewed bleeding several days post-operatively
- Blood clots appearing in saliva consistently
Infection Indicators
- Fever exceeding 101°F (38.3°C) with chills
- Foul taste or odor emanating from extraction sites
- Visible pus or yellow discharge
- Increasing facial swelling after 72 hours
- Red streaking extending from surgical areas
Functional Limitations
- Difficulty opening the mouth (trismus) that worsens over time
- Problems swallowing liquids or medications
- Persistent nausea preventing adequate nutrition
- Numbness extending beyond expected anesthesia duration
Initial Self-Care Interventions
Before seeking professional care, several self-management techniques may address minor complications:
Bleeding Control: Apply firm pressure using clean gauze pads for 45-60 minutes while sitting upright. Avoid repeatedly checking the site, which can disrupt clot formation.
Swelling Management: Continue cold therapy applications and maintain head elevation during rest periods. Over-the-counter anti-inflammatory medications can provide additional relief.
Pain Relief: Ensure proper medication timing and dosing according to prescribed schedules. Combination therapy using both prescription and over-the-counter options often proves most effective.
Managing Specific Complications
Dry Socket Treatment
This condition requires professional intervention, as dentists must clean the extraction site and apply medicated dressings to promote healing. Home remedies prove inadequate for managing dry socket effectively.
Minor Infections
Early-stage infections may respond to enhanced oral hygiene using warm salt water rinses and prescribed antibiotics. However, professional evaluation remains essential to prevent progression to serious complications.
Persistent Swelling
Swelling continuing beyond one week may indicate infection, allergic reactions, or other complications requiring professional assessment and treatment modification.
Consulting Your Dental Professional
Your oral surgeon or general dentist possesses comprehensive knowledge of your specific surgical circumstances, medical history, and individual risk factors that influence recovery recommendations.
Importance of Personalized Care
Every wisdom tooth extraction presents unique challenges based on tooth position, surgical complexity, patient age, and underlying health conditions. Generic advice cannot replace individualized professional guidance tailored to your specific situation.
Communication Guidelines
Maintain open communication channels with your dental team throughout the recovery process. Most practices provide emergency contact information for urgent concerns arising outside normal business hours.
Routine Questions: Schedule follow-up appointments as recommended, typically 1-2 weeks post-operatively for healing assessment and suture removal if necessary.
Urgent Concerns: Contact your practitioner immediately for signs of infection, uncontrolled pain, persistent bleeding, or suspected dry socket development.
Prescription Management
Pain medications and antibiotics typically require refills during standard business hours. Plan ahead for weekend or holiday periods by ensuring adequate medication supplies for comfort management.
Safe Reintroduction of Straws
Once your oral surgeon approves straw usage—typically after the one-week minimum restriction period—gradual reintroduction using gentle techniques minimizes complication risks.
Progressive Reintroduction Strategy
Initial Attempts: Begin with thin liquids like water or diluted juices, using minimal suction pressure to test tolerance. Start with brief sipping sessions rather than prolonged drinking periods.
Monitoring Protocol: Pay careful attention to any discomfort, unusual tastes, or signs of bleeding following straw use. Discontinue immediately if any adverse symptoms develop.
Gradual Progression: Successfully tolerated thin liquids can be followed by slightly thicker beverages, always maintaining gentle suction techniques.
Long-Term Benefits of Straw Usage
Once complete healing occurs, straws offer several advantages for post-surgical patients:
- Precise Liquid Delivery: Directs beverages past sensitive areas that may remain slightly tender
- Hygiene Maintenance: Reduces contact between liquids and healing extraction sites
- Convenience Factor: Facilitates consumption of nutritional shakes and liquid supplements
- Temperature Control: Allows consumption of cold beverages that might otherwise cause discomfort through direct contact
Alternative Straw Considerations
While research specifically comparing different straw types remains limited, logical considerations suggest that wider-diameter straws might require less suction pressure than narrow varieties. However, no definitive evidence establishes safety differences between plastic, metal, silicone, or paper straw materials regarding dry socket risk.
Addressing Information Limitations
Current dental literature focuses primarily on straw avoidance rather than detailed reintroduction protocols or comparative analysis of different straw types and techniques.
Straw Type Considerations
Professional recommendations typically address “straw usage” generically without distinguishing between various materials, diameters, or designs. No published studies compare suction pressures generated by different straw configurations or their relative safety profiles.
Special Circumstances
Limited guidance exists for patients who might require straw usage due to physical limitations, neurological conditions, or other medical circumstances that complicate alternative hydration methods. Such situations require individualized professional consultation.
Evidence Gaps
Further research could potentially establish:
- Optimal straw diameters for minimizing suction pressure
- Comparative safety profiles of different straw materials
- Modified techniques for patients with special hydration needs
- Precise pressure measurements correlating with dry socket risk
Frequently Asked Questions about “When can i use a straw after wisdom teeth removal?”
1. When can I safely use a straw after wisdom teeth removal?
Most dentists recommend waiting at least one week before using a straw after wisdom teeth extraction. This is because the suction created by using a straw can dislodge the blood clot that forms in the extraction site, which is essential for healing. Using a straw too soon increases the risk of a painful complication called dry socket. Some sources suggest waiting at least 3 to 5 days, but a full week is safer to ensure the clot has stabilized.
2. Why is using a straw risky after wisdom teeth removal?
The main risk is that the suction from a straw can dislodge the blood clot that forms in the tooth socket after extraction. This clot protects the underlying bone and nerves and helps the wound heal. If the clot is dislodged, it can cause dry socket, a painful condition that delays healing and may require additional dental treatment.
3. What happens if I use a straw too early after surgery?
Using a straw too early can cause the blood clot to be sucked out from the socket, exposing the bone and nerves underneath. This leads to dry socket, which causes severe pain, delayed healing, and sometimes infection. It can make recovery longer and more uncomfortable, often requiring extra visits to the dentist for treatment.
4. Are there alternatives to using a straw during recovery?
Yes. Instead of a straw, you can drink liquids directly from a cup or glass to avoid suction. This helps protect the blood clot and surgical site. Also, using a straw can be helpful later on for precise liquid intake, especially if opening your mouth wide is uncomfortable. But this should only be done after the recommended waiting period.
5. How can I ensure a smooth recovery after wisdom teeth removal?
- Avoid using straws for at least one week or as advised by your dentist.
- Do not smoke or engage in other activities that create suction.
- Follow your dentist’s instructions on oral hygiene and diet.
- Stick to soft foods and avoid hot or spicy foods initially.
- Keep the surgical area clean but avoid vigorous rinsing in the first days.
- Contact your dentist if you experience severe pain, bleeding, or signs of infection.
Conclusion
Patience during the initial healing phase following wisdom teeth removal proves essential for preventing painful complications and ensuring optimal recovery outcomes. The one-week minimum waiting period for straw usage reflects evidence-based recommendations designed to protect vital blood clots and minimize dry socket risk.
Understanding the scientific rationale behind suction avoidance—preventing clot dislodgement through negative pressure—helps patients appreciate the importance of following post-operative restrictions. Effective hydration alternatives including direct cup drinking, spoon-fed liquids, and moisture-rich foods maintain adequate fluid intake without compromising healing.
Comprehensive post-operative care encompassing dietary modifications, gentle oral hygiene, appropriate pain management, and activity restrictions significantly influences recovery success. Early recognition of potential complications enables prompt professional intervention and prevents serious sequelae.
Always prioritize your oral surgeon’s or dentist’s specific instructions over general guidelines, as they possess intimate knowledge of your particular surgical circumstances and individual risk factors. Open communication with your dental team throughout the recovery process ensures personalized care and optimal healing outcomes.
Following evidence-based post-operative protocols leads to smoother, more comfortable recovery experiences and reduces the likelihood of complications that could extend healing timelines or require additional treatment interventions.
References
A. General Dental and Oral Surgery Guidelines (Authoritative Bodies):
Source: American Dental Association (ADA) – MouthHealthy.org (patient education site)
Content: While not a specific research paper, the ADA provides patient guidance based on established dental practices. In their advice for post-extraction care, they typically warn against actions that can dislodge the blood clot.
Typical Advice (Paraphrased from general post-op care): “Don’t use straws for the first few days. The sucking motion can loosen the clot and delay healing.” (Exact wording may vary, but the principle is consistent).
Specific page example (though they might update layouts): Look for articles on “Dry Socket” or “Wisdom Tooth Extraction Aftercare” on mouthhealthy.org.
For instance, under “Dry Socket Symptoms and Treatment”: “Things that can increase your risk of developing dry socket include… Sucking through a straw.”
Source: American Association of Oral and Maxillofacial Surgeons (AAOMS) – MyOMS.org (patient information)
Content: AAOMS provides comprehensive guidelines for post-operative care following oral surgery procedures, including wisdom tooth removal.
Typical Advice (Paraphrased): “Do not use straws… Sucking on a straw can dislodge the blood clot that is essential for healing.” They often recommend avoiding straws for at least a week.
Specific information can be found in their patient care sections relating to wisdom teeth removal.
Source: UK National Health Service (NHS)
Content: The NHS provides public health information and often includes advice on dental procedures.
Typical Advice (Paraphrased from wisdom tooth removal aftercare): “For the first 24 hours… avoid sucking on straws… as this can dislodge blood clots that are helping your wound to heal.” Some advice extends this period.
Example: Search “wisdom tooth removal aftercare NHS” – you’ll find guidance like: “For 24 hours… Avoid drinking through a straw.” (They often give a minimum, but advise following surgeon’s specific instructions for longer).
B. Scientific Literature on Dry Socket (Alveolar Osteitis):
While it’s harder to find a specific double-blind, placebo-controlled study solely on “straw use vs. no straw use” because the mechanism is fairly well understood and subjecting patients to a known risk factor would be ethically questionable, the literature on dry socket risk factors consistently points to activities that create negative pressure or disturb the clot.
Study/Review: Bowe, D. C., Rogers, S., Stassen, L. F. A. (2011). “The management of dry socket/alveolar osteitis.” Journal of the Irish Dental Association, 57(6), 305-310.
Content: This review discusses the etiology, risk factors, and management of alveolar osteitis. While not focused solely on straws, it discusses factors that lead to fibrinolysis (breakdown of the clot) or mechanical dislodgement.
Relevance: “Mechanical disruption of the clot in the early postoperative phase” is listed as a contributing factor. Straw use falls under this category.
Study/Review: Blum, I. R. (2002). “Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of pathogenesis and management.” International Journal of Oral and Maxillofacial Surgery, 31(3), 309-317.
Content: This article reviews the pathogenesis of dry socket. It highlights that the “loss or disintegration of the blood clot” is the key event.
Relevance: While not singling out straws in a dedicated experiment, it explains that “excessive mouth rinsing or negative pressure (e.g., sucking on a straw)” are commonly cited patient-related factors that can lead to clot dislodgement.
Textbook Reference: Hupp, J. R., Ellis III, E., & Tucker, M. R. (Eds.). (2019). Contemporary Oral and Maxillofacial Surgery (7th ed.). Mosby Elsevier.
Content: Standard textbooks in oral surgery detail post-operative instructions and complication management.
Relevance: Such texts will universally list avoiding suction (from straws, smoking) as a key preventative measure against dry socket due to the risk of dislodging the blood clot. The mechanism is considered established knowledge. For example, in sections on prevention of complications: “Patients should be instructed to avoid activities that might dislodge the blood clot, such as vigorous rinsing, spitting, or sucking through a straw for several days.”
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.