“Why Does My Back Hurt When I Wake Up? ” (And How to Fix It) Discover why your back hurts when you wake up. Explore causes like poor sleep posture, weak core, and mattress issues—and how to fix them.

Is your back pain getting worse at night?
Waking Up to Pain
You didn’t wake up to your alarm – your back pain did the job. This frustrating scenario affects over 16 million adults in the United States who experience chronic morning back pain, transforming what should be a refreshing start into a daily struggle with discomfort and stiffness. Morning back pain represents one of the most common musculoskeletal complaints, encompassing everything from mild morning stiffness to debilitating low back pain that can persist throughout the day.
Understanding why your spine rebels against you each morning requires examining multiple interconnected factors: your sleep environment, underlying medical conditions, lifestyle habits, and even your body’s natural circadian rhythms. This comprehensive guide will explore the complex relationship between sleep and spinal health, examine both common and overlooked causes of morning back pain, and provide evidence-based solutions to help you wake up pain-free. We’ll also discuss when morning back pain signals a serious medical condition requiring professional intervention, ensuring you have the knowledge to make informed decisions about your spinal health.
Common Causes of Morning Back Pain
Upper Back Pain After Sleeping
Sleeping Position & Mattress Support
Poor sleeping posture ranks as the primary culprit behind morning back pain, with your chosen sleep position directly impacting spinal alignment throughout the night. Stomach sleeping forces your neck into an unnatural rotation while creating excessive lumbar lordosis, placing tremendous stress on your intervertebral discs and facet joints. Side sleeping, while generally healthier, can cause problems when your spine curves laterally due to inadequate pillow support or mattress sagging. Back sleeping typically provides optimal spinal alignment, though it requires proper pillow height to maintain the natural cervical curve.
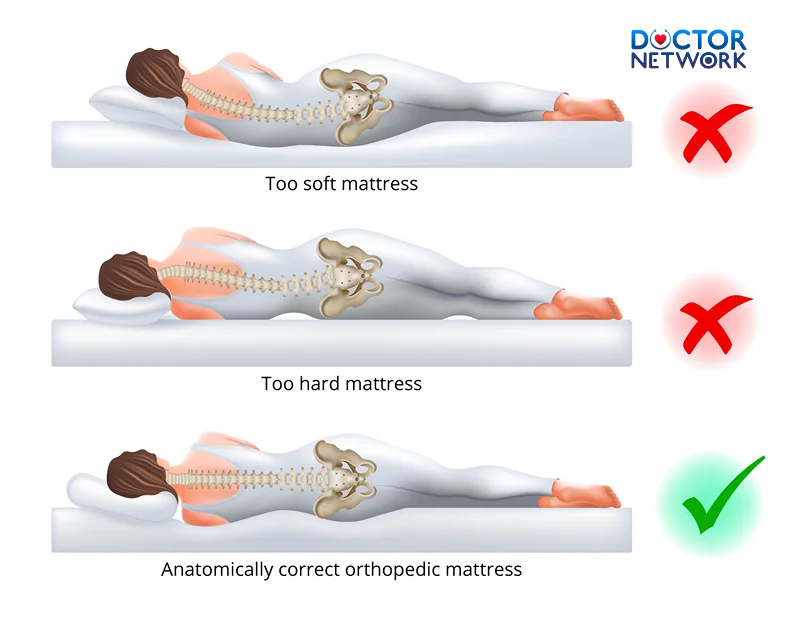
Mattress firmness plays a crucial role in maintaining proper spinal alignment and pressure point relief. A mattress that’s too soft allows your body to sink excessively, creating a hammock effect that strains your lumbar spine. Conversely, an overly firm surface fails to accommodate your body’s natural curves, creating pressure points at your shoulders and hips. The ideal mattress provides medium-firm support that contours to your body while maintaining spinal neutrality. Orthopedic pillows and proper pillow alignment are equally important, supporting your neck’s natural curve and preventing compensatory muscle tension.
| Sleep Position | Spinal Impact | Recommended Support |
|---|---|---|
| Stomach Sleeping | Excessive lumbar extension, neck rotation | Thin pillow, avoid if possible |
| Side Sleeping | Potential lateral spine curvature | Firm pillow between knees, supportive head pillow |
| Back Sleeping | Optimal spinal alignment potential | Medium-height pillow, small lumbar roll |
Morning Stiffness Explained
Morning stiffness occurs due to prolonged inactivity during sleep, which reduces synovial fluid circulation within your spinal joints. This natural lubricant becomes thicker and less mobile after hours of immobility, causing your joints to feel stiff and resistant to movement upon waking. Normal morning stiffness typically resolves within 15-30 minutes of gentle movement and is considered a natural physiological response to extended rest periods.
Pathological morning stiffness, however, persists for more than an hour and may indicate underlying inflammatory conditions or degenerative changes in your spine. The key distinction lies in both duration and response to movement – normal stiffness improves quickly with gentle activity, while pathological stiffness may worsen initially before gradually improving. Understanding this difference helps determine whether your morning back pain represents a normal physiological response or requires medical evaluation.
Degenerative Disc Disease (DDD)
Degenerative disc disease affects millions of adults, causing intervertebral discs to lose water content and height over time. This natural aging process becomes problematic when discs lose their ability to absorb shock and maintain proper spacing between vertebrae. During sleep, your discs naturally rehydrate as gravitational pressure decreases, but this process can be incomplete in degenerated discs, leading to increased morning stiffness and pain.
The relationship between disc degeneration and morning pain involves complex biomechanical changes in your spine. As discs lose height, facet joints experience increased stress, and surrounding ligaments may become slack or overstretched. Spinal decompression occurs naturally during sleep as your body lies horizontal, but the transition back to upright posture can be particularly challenging when discs cannot adequately support your spine’s weight. This explains why many people with degenerative disc disease experience their worst pain within the first hour of waking.
Weak Core Muscles & Postural Imbalance
Inadequate core strength creates a cascade of problems that manifest most prominently in the morning when your muscles are least active. Your core muscles – including the deep abdominals, pelvic floor, diaphragm, and multifidus – work together to stabilize your lumbar spine and maintain proper posture. When these muscles are weak or poorly coordinated, your passive structures (ligaments, discs, and bones) must compensate, leading to increased stress and morning pain.
Postural imbalance develops gradually as certain muscle groups become tight while others weaken, creating dysfunction that persists even during sleep. Hip flexors often become shortened from prolonged sitting, while glutes become inhibited and weak. This imbalance tilts your pelvis forward, increasing lumbar lordosis and placing excessive stress on your lower back. Companies like Hinge Health have developed digital therapeutics programs that specifically address these muscular imbalances through targeted exercises and movement coaching, demonstrating the growing recognition of core stability’s importance in managing back pain.
Medical Conditions to Rule Out
Ankylosing Spondylitis (AS)
Ankylosing spondylitis represents a serious inflammatory autoimmune disease that primarily affects the spine and sacroiliac joints. The hallmark feature of AS-related back pain is its improvement with movement – a characteristic that distinguishes it from mechanical back pain, which typically worsens with activity. This inflammatory back pain often begins gradually in young adults and follows a pattern of morning stiffness lasting more than an hour, with symptoms improving throughout the day as activity increases.
The pathophysiology of AS involves chronic inflammation of the entheses (sites where tendons and ligaments attach to bone), leading to progressive fusion of spinal joints if left untreated. Early recognition is crucial because modern biologic medications can significantly slow disease progression and improve quality of life. Red flag symptoms include back pain that begins before age 40, gradual onset over months rather than acute injury, pain that improves with exercise, and stiffness lasting more than 30 minutes each morning.
Disc Herniation or Spinal Stenosis
Disc herniation occurs when the soft inner core of an intervertebral disc protrudes through its outer fibrous ring, potentially compressing nearby nerve roots. Morning symptoms can be particularly severe because discs naturally expand slightly during sleep due to decreased gravitational pressure, making herniated material more likely to compress neural structures. Pain typically radiates into the buttock or leg, following specific nerve distribution patterns that help identify the affected spinal level.
Spinal stenosis involves narrowing of the spinal canal or neural foramina, creating pressure on nerve roots or the spinal cord itself. This condition often causes neurogenic claudication – leg pain that worsens with walking and improves with sitting or leaning forward. Morning symptoms may include numbness, tingling, or weakness in the legs, particularly after lying flat all night. When conservative treatments fail to provide relief, consultation with a pain specialist or spine surgeon becomes necessary to explore advanced treatment options including epidural injections or surgical decompression.
Overlooked Causes You Should Know
Stress, Cortisol & Sleep Disruption
The relationship between psychological stress and morning back pain involves complex neuroendocrine pathways that many patients and healthcare providers overlook. Cortisol levels naturally peak in the early morning as part of your body’s circadian awakening response, but chronic stress can dysregulate this pattern, leading to excessive cortisol production that heightens pain sensitivity and promotes muscle tension. This stress-pain cycle creates a self-perpetuating pattern where pain increases stress, which in turn amplifies pain perception.
Sleep disruption compounds this problem by interfering with your body’s natural recovery processes. During deep sleep stages, your body releases growth hormone and reduces inflammatory cytokines, both essential for tissue repair and pain management. Chronic stress disrupts your circadian rhythm and can suppress melatonin production, leading to fragmented sleep that prevents adequate recovery. The result is morning awakening with increased muscle tension, heightened pain sensitivity, and reduced coping mechanisms for managing discomfort.
Chronotype Matters: Night Owl vs Morning Person
Your natural chronotype – whether you’re naturally a morning person or night owl – significantly influences your pain perception and recovery patterns. Research shows that circadian misalignment, where your sleep schedule conflicts with your natural biological clock, can worsen morning pain symptoms. Night owls forced to wake early for work or family obligations often experience more severe morning stiffness because their bodies haven’t completed natural recovery cycles.
REM sleep and deep sleep stages play crucial roles in pain processing and muscle recovery. When your sleep schedule conflicts with your natural chronotype, you may miss optimal windows for these critical sleep stages, leading to incomplete recovery and increased morning pain. Sleep quality becomes more important than sleep quantity when your circadian rhythms are misaligned, making it essential to work with your natural tendencies rather than against them when possible.
Occupation-Related Morning Pain
Certain occupations significantly increase the risk of morning back pain through their impact on daytime posture and nighttime recovery. Desk workers who spend eight or more hours in seated positions develop characteristic patterns of muscle tightness and weakness that persist into sleep. Hip flexors become shortened, thoracic spine rounds forward, and deep neck flexors weaken, creating postural distortions that affect spinal alignment even when lying down.
Occupation-related factors extend beyond obvious physical demands to include stress levels, work schedules, and access to movement throughout the day. Truck drivers face the double challenge of prolonged sitting and vibration exposure, both of which increase disc pressure and muscle fatigue. Warehouse workers and healthcare professionals who perform repetitive lifting or bending motions may develop asymmetrical muscle patterns that create uneven stress on the spine during sleep. The key insight is that daytime posture and movement patterns directly influence nighttime recovery, making occupational factors crucial considerations in managing morning back pain.
How to Wake Up Without Back Pain
Getting Out of Bed With Better Posture
Upgrade Your Sleep Setup
Selecting the right mattress requires understanding how different materials and constructions affect spinal support and pressure relief. Memory foam mattresses excel at contouring to body shape and reducing pressure points, making them ideal for side sleepers with hip or shoulder pain. However, traditional memory foam can trap heat and may lack sufficient support for heavier individuals or those requiring firmer surfaces. Hybrid mattresses combine memory foam comfort layers with innerspring support cores, providing balanced support and temperature regulation.
Latex mattresses offer natural resilience and cooling properties while providing consistent support across all sleep positions. They resist sagging longer than memory foam and provide more responsive support that facilitates easy position changes during sleep. Sleep Number beds allow couples to customize firmness on each side, addressing individual needs without compromise. Tempur-Pedic pioneered pressure-relieving memory foam technology and continues to innovate with cooling technologies and zoned support systems.
| Mattress Type | Best For | Pros | Cons |
|---|---|---|---|
| Memory Foam | Side sleepers, pressure relief | Excellent contouring, motion isolation | Heat retention, slow response |
| Hybrid | Combination sleepers | Balanced support and comfort | Higher cost, potential for sagging |
| Latex | Hot sleepers, eco-conscious | Natural materials, cooling, durable | Expensive, limited contouring |
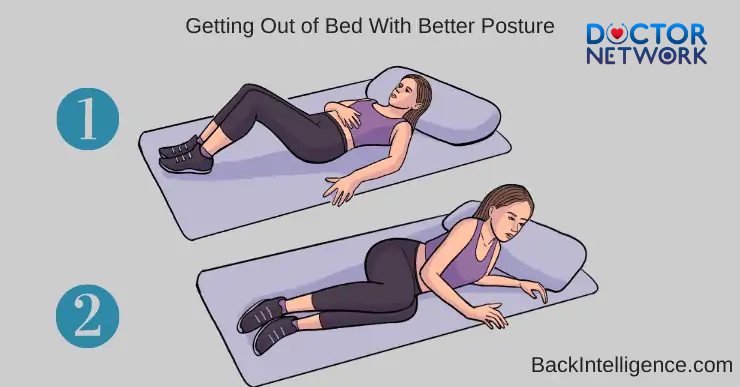
Get-Out-of-Bed Techniques That Protect Your Spine
Proper bed exit technique significantly reduces morning back pain by minimizing stress on your spine during the vulnerable transition from horizontal to vertical positioning. The five-step technique begins with rolling onto your side rather than sitting straight up, which places enormous stress on your lumbar discs and can trigger muscle spasms in already stiff morning muscles.
The complete sequence involves: roll to your side, push up using your arms while keeping your spine neutral, sit on the bed edge with feet flat on the floor, pause to allow your cardiovascular system to adjust and muscles to activate, then stand using your leg muscles rather than your back. This technique, endorsed by posture correction specialists and physical therapists, reduces disc pressure by up to 40% compared to traditional straight-up sitting. Spinal decompression continues during the pause phase as your discs gradually adjust to gravitational loading, making the final transition to standing much safer and more comfortable.
Morning Bed Stretches: A 5-Minute Routine
A targeted morning stretch routine can significantly reduce back pain by gradually activating muscles and improving joint mobility before getting out of bed. The American Physical Therapy Association recommends gentle movements that progress from passive positioning to active muscle engagement, respecting your body’s need for gradual awakening.
Essential morning bed stretches include:
- Pelvic tilts – Lie on your back with knees bent, gently rock your pelvis to flatten your lower back against the mattress, hold for 5 seconds, repeat 10 times
- Knee-to-chest stretch – Pull one knee toward your chest, hold for 30 seconds, switch sides, then pull both knees together
- Spinal rotation – Keep knees bent and drop them to one side while keeping shoulders flat, hold 30 seconds each direction
- Cat-cow on side – While lying on your side, arch and round your back gently to mobilize the entire spine
- Hip flexor stretch – Lie at bed edge, let one leg hang down while pulling the opposite knee to chest
These movements activate your deep stabilizing muscles, improve synovial fluid circulation, and prepare your spine for the demands of upright posture. The routine takes only five minutes but can prevent hours of discomfort throughout your day.
Using Sleep Tech to Track & Improve
Modern wearable tech offers unprecedented insights into sleep patterns and their relationship to morning back pain. The Oura Ring tracks sleep stages, heart rate variability, and movement patterns, providing data that correlates with pain levels and recovery quality. Apple Watch sleep tracking features monitor movement, heart rate, and sleep duration, helping identify patterns that contribute to morning stiffness.
Smart mattresses with built-in sensors can track sleep posture, movement frequency, and pressure distribution throughout the night. This sleep data reveals whether you’re spending too much time in positions that stress your spine or if you’re tossing and turning due to discomfort. Back pain monitoring apps allow you to correlate sleep metrics with morning pain levels, identifying triggers and tracking improvement over time.
Advanced sleep technology also includes adjustable bases that can elevate your head or feet, reducing pressure on specific areas of your spine. Some systems integrate with smart home technology to optimize bedroom temperature and lighting for better sleep quality. The key is using this technology purposefully rather than obsessively, focusing on trends and patterns rather than nightly variations.
Personalized Assessment: What Kind of Pain Do You Have?
Understanding your specific type of morning back pain requires careful analysis of symptoms, timing, and triggers. This interactive self-assessment helps categorize your pain and guide appropriate treatment approaches:
Pain Characteristics Assessment:
- ✔ Is your pain better after 30 minutes of movement? (Suggests inflammatory component)
- ✔ Do you often sleep less than 6 hours? (Indicates inadequate recovery time)
- ✔ How old is your mattress? (Ages over 7 years may lack adequate support)
- ✔ Does pain radiate into your legs? (May indicate nerve involvement)
- ✔ Is stiffness worse on weekends when you sleep longer? (Suggests positional factors)
- ✔ Do you wake up multiple times during the night? (Points to sleep quality issues)
Pain Categories:
Muscular Pain typically responds well to movement, feels tight or achy, and improves with stretching and gentle activity. This type often results from poor sleep positioning or inadequate mattress support.
Postural Pain develops gradually and correlates with work activities or lifestyle factors. It often improves with posture correction and ergonomic modifications.
Inflammatory Pain is characterized by prolonged morning stiffness (over 1 hour), improvement with movement, and may be associated with systemic symptoms like fatigue.
Behavioral Pain relates to stress, sleep habits, or lifestyle factors and often varies with life circumstances and stress levels.
Bonus: Stats You Should Know
Recent research reveals compelling statistics about morning back pain that highlight both its prevalence and impact on daily life. Over 63% of people with chronic back pain report that their symptoms are worst in the morning, with many describing it as the most challenging part of their day. This statistic underscores the importance of addressing sleep-related factors in comprehensive back pain management.
Age-related trends show that individuals over 40 are twice as likely to experience morning back pain compared to younger adults, reflecting the cumulative effects of degenerative changes, lifestyle factors, and sleep pattern changes that occur with aging. The Sleep Foundation reports that sleep quality decreases significantly after age 40, coinciding with increased prevalence of morning musculoskeletal complaints.
Key Statistics Summary:
- 16+ million Americans experience chronic morning back pain
- 63% of back pain sufferers report worst symptoms upon waking
- Adults over 40 have 2x higher risk of morning back pain
- Average mattress replacement cycle is 7-10 years, but 40% of people sleep on mattresses older than 8 years
- Morning back pain accounts for 23% of lost productivity in the first two hours of the workday
These statistics, compiled from sources including Medical News Today and the Sleep Foundation, demonstrate that morning back pain represents a significant public health issue with substantial economic and personal impacts.
A Better Morning Starts Tonight
Morning back pain stems from a complex interplay of factors including sleep positioning, mattress quality, underlying medical conditions, stress levels, and individual anatomical variations. The key insight is that achieving pain-free mornings requires a holistic approach that addresses sleep hygiene, physical conditioning, stress management, and environmental factors rather than focusing solely on symptom treatment.
Proactive changes you can implement immediately include evaluating your current sleep setup, practicing proper bed exit techniques, and incorporating gentle morning stretches into your routine. Consider your mattress age and quality, pillow support, and sleep position preferences as foundational elements that significantly impact your morning comfort. Stress reduction techniques, regular exercise, and core strengthening exercises provide long-term benefits that extend beyond pain relief to overall health improvement.
Call-to-action: While many cases of morning back pain respond well to conservative management and lifestyle modifications, persistent pain that lasts more than two weeks despite appropriate self-care measures warrants professional evaluation. Early intervention by qualified healthcare providers can prevent chronic pain development and identify underlying conditions that require specific treatment. Don’t let morning back pain become your new normal – take action today to reclaim comfortable, energizing mornings that set a positive tone for your entire day.
Frequently asked questions about the topic “Why does my back hurt when I wake up?”
1. Why does my back hurt when I wake up in the morning?
Answer:
Back pain upon waking is often caused by poor sleeping posture, an unsupportive mattress, or lack of proper spinal alignment during sleep. Overnight, muscles and joints can become stiff, and if your mattress or pillow does not support your body correctly, it can lead to discomfort and pain.
2. Can sleeping position cause back pain in the morning?
Answer:
Yes, certain sleeping positions can strain your back. For example, sleeping on your stomach can put pressure on your spine and neck, while sleeping on your back or side with proper support can help maintain spinal alignment and reduce pain.
3. Could my mattress be the reason for my morning back pain?
Answer:
Absolutely. A mattress that is too soft or too firm can cause your spine to be out of alignment during sleep. Over time, this can lead to muscle strain and back pain. It’s important to choose a mattress that supports your natural spinal curve.
4. When should I see a doctor about my morning back pain?
Answer:
If your back pain is severe, lasts more than a few weeks, or is accompanied by other symptoms like numbness, weakness, or loss of bladder control, you should see a healthcare professional promptly. Persistent or worsening pain may indicate an underlying condition that needs medical attention.
5. What can I do to reduce back pain when I wake up?
Answer:
To reduce morning back pain, try improving your sleep posture, use a supportive mattress and pillow, stretch gently before getting out of bed, and maintain a regular exercise routine to strengthen your back muscles. Avoid sleeping on your stomach and consider consulting a physical therapist for personalized advice.
References
Link: https://onlinelibrary.wiley.com/doi/10.1002/art.24491 (Study on Circadian Rhythms of Cytokines)
Link: https://arthritis-research.biomedcentral.com/articles/10.1186/ar744 (Review on Intervertebral Disc Degeneration by Dr. Urban)
Link: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(03)14792-7/fulltext (Kovacs study on mattress firmness)
Link: https://journals.lww.com/spinejournal/Abstract/1996/11150/Inefficient_Muscular_Stabilization_of_the_Lumbar.8.aspx (Hodges study on core muscle stabilization)
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.

























