“Why Experts Now Say Not To Remove Your Wisdom Teeth” – Learn modern criteria for safe retention and when surgical removal is necessary.

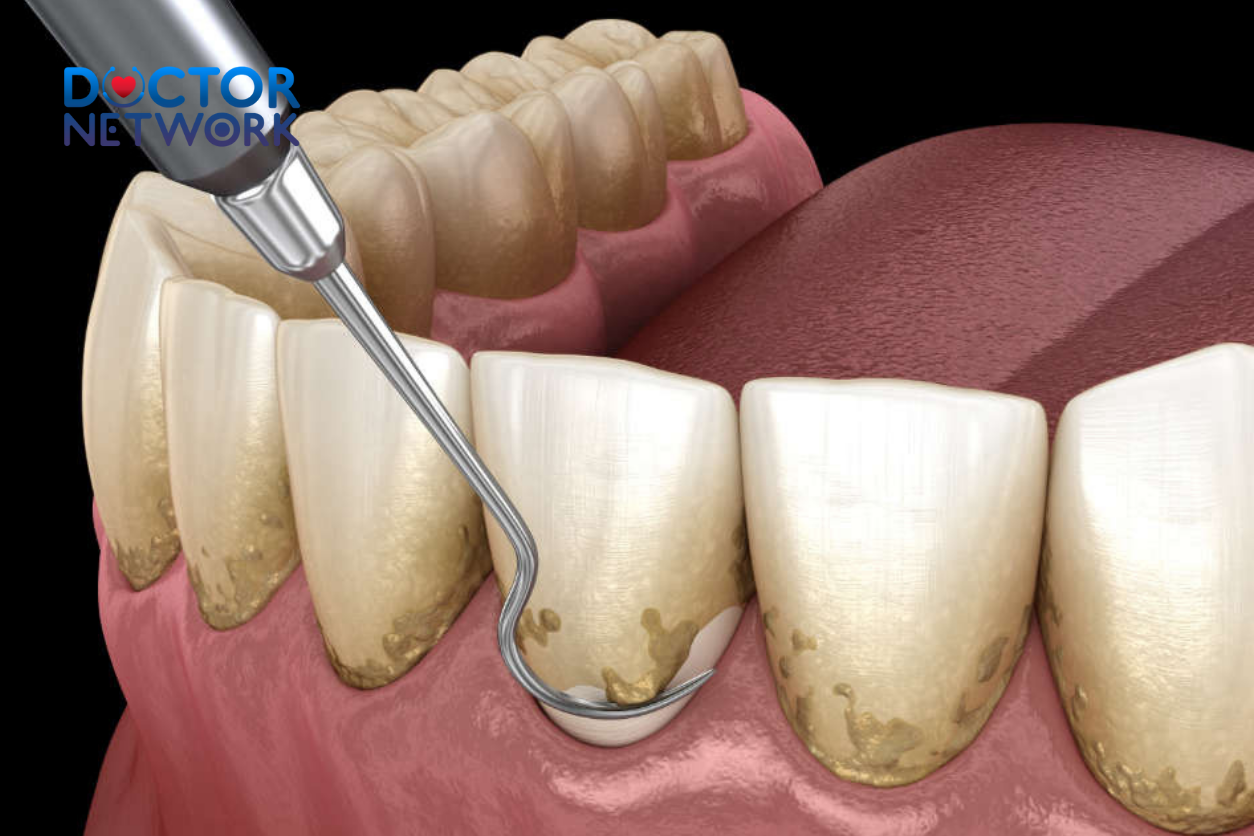
What wisdom tooth removal look like
For decades, extracting wisdom teeth was considered standard preventative care, with oral surgeons routinely recommending removal to avoid potential future complications. However, contemporary dental professionals and maxillofacial surgeons now advocate for a fundamentally different approach—one that prioritizes individual assessment over blanket prophylactic procedures. This paradigm shift stems from mounting clinical evidence demonstrating that asymptomatic third molars rarely cause the predicted problems, while unnecessary extractions expose patients to avoidable surgical risks, financial burden, and recovery complications.
This comprehensive analysis examines the evolution of clinical guidelines surrounding wisdom tooth management, explores the scientific rationale behind current recommendations, identifies criteria for safe retention, and provides essential guidance for patients navigating this important oral health decision.
The Evolution of Expert Opinion on Wisdom Tooth Extraction
The historical preference for routine wisdom tooth removal originated from theoretical concerns about dental crowding, impaction, and periodontal disease. Traditional oral surgery protocols emphasized prophylactic extraction during adolescence or early adulthood, based on assumptions that third molars would inevitably cause orthodontic relapse or become sites of pathology. This preventative philosophy dominated dental education and clinical practice throughout the mid-20th century, influencing generations of practitioners to recommend systematic removal regardless of symptomatology.
Recent longitudinal studies and systematic reviews have fundamentally challenged these long-held beliefs. Evidence-based dentistry now demonstrates that prophylactic wisdom tooth extraction lacks scientific justification in most cases. The American Association of Oral and Maxillofacial Surgeons, along with the American Dental Association, have revised their clinical guidelines to reflect this paradigmatic transformation. Contemporary protocols emphasize individualized risk assessment, continuous monitoring, and intervention only when clear pathological indicators manifest.
This evolution represents a broader shift toward precision medicine in oral healthcare. Modern dental professionals now recognize that each patient’s anatomical configuration, oral hygiene capacity, and risk profile requires customized evaluation rather than standardized treatment protocols. The integration of advanced diagnostic imaging, including cone-beam computed tomography and panoramic radiography, enables more accurate assessment of third molar positioning and associated structures.
Reasons Why Experts Now Advise Against Routine Removal

Wisdom tooth extraction can cause dry socket
Absence of Clinical Justification for Asymptomatic Teeth
The primary factor driving expert recommendations against routine extraction centers on the lack of empirical evidence supporting prophylactic removal of healthy, asymptomatic wisdom teeth. Extensive population-based studies reveal that the majority of properly positioned third molars remain functionally stable throughout adulthood without causing predicted complications such as dental crowding or periodontal deterioration.
Research conducted by the Cochrane Collaboration and published in systematic reviews demonstrates minimal correlation between wisdom tooth presence and anterior tooth irregularity. The orthodontic community has largely abandoned the theory that third molars significantly contribute to post-treatment relapse, recognizing that multiple factors—including genetic predisposition, muscular forces, and periodontal changes—influence long-term dental alignment more substantially than wisdom tooth pressure.
Pathological manifestations such as cyst formation, root resorption of adjacent molars, and severe periodontal disease occur in fewer than 12% of retained wisdom teeth over a 25-year follow-up period, according to longitudinal cohort studies. This relatively low incidence rate challenges the traditional rationale for preventative extraction, particularly when weighed against the inherent risks of surgical intervention.
Surgical Risks Outweighing Potential Benefits
Contemporary risk-benefit analyses consistently demonstrate that the morbidity associated with wisdom tooth extraction frequently exceeds the probability of future complications from retention. Surgical removal of third molars carries significant procedural risks, particularly for mandibular extractions where proximity to the inferior alveolar nerve and lingual nerve creates potential for temporary or permanent sensory disturbances.
Post-operative complications include alveolar osteitis (dry socket) occurring in 2-5% of extractions, post-surgical infections requiring antibiotic intervention, excessive hemorrhaging necessitating emergency care, and damage to adjacent dental structures. Maxillofacial trauma, though rare, can result from complex extractions involving deeply impacted or horizontally positioned teeth requiring extensive bone removal and soft tissue manipulation.
The American Journal of Oral and Maxillofacial Surgery reports complication rates ranging from 4.6% for simple erupted extractions to 30.9% for surgical removal of impacted mandibular third molars. These statistics underscore the importance of reserving surgical intervention for cases with documented pathology rather than theoretical prevention scenarios.
Economic Burden and Recovery Impact
Unnecessary wisdom tooth extraction imposes substantial financial costs on patients and healthcare systems. Average extraction fees range from $225-$750 per tooth for simple procedures, escalating to $1,500-$4,000 for complex surgical cases requiring general anesthesia and specialist intervention. Insurance coverage varies significantly, often leaving patients responsible for substantial out-of-pocket expenses for elective procedures.
The recovery period following wisdom tooth extraction typically spans 3-7 days for simple cases and up to 2-3 weeks for complicated surgical procedures. This downtime affects work productivity, academic performance, and daily functioning. Patients frequently require prescription pain medication, antibiotics, and multiple follow-up appointments, adding indirect costs to the overall treatment burden.
Societal healthcare expenditure for routine wisdom tooth removal exceeds $3 billion annually in the United States alone. This substantial resource allocation could be redirected toward evidence-based preventative care and treatment of established pathology, improving overall population oral health outcomes more effectively.
Enhanced Diagnostic Capabilities and Monitoring Protocols
Modern dental technology provides unprecedented ability to monitor third molar development and detect early pathological changes without resorting to prophylactic extraction. Digital panoramic radiography, cone-beam computed tomography, and intraoral scanning enable precise assessment of root morphology, bone density, periodontal status, and spatial relationships with adjacent structures.
Advances in periodontal probing techniques, bacterial sampling, and inflammatory biomarker detection allow clinicians to identify incipient disease processes before they progress to irreversible pathology. This enhanced diagnostic precision facilitates targeted intervention when truly necessary while avoiding unnecessary surgical procedures for stable, healthy teeth.
Patient education programs emphasizing proper oral hygiene techniques, dietary modifications, and regular professional maintenance have significantly improved long-term outcomes for retained wisdom teeth. Evidence-based preventative strategies prove more cost-effective and less invasive than routine surgical removal for managing third molar-related concerns.
Criteria for When Wisdom Teeth Can Be Safely Retained

Fully erupted and properly aligned with opposing teeth
Complete Eruption and Functional Integration
Wisdom teeth demonstrating complete eruption through the gingival tissues with adequate crown exposure can often be safely maintained throughout adulthood. Properly erupted third molars that achieve functional occlusion with opposing teeth contribute to masticatory efficiency and help maintain posterior support for the dental arch. These teeth integrate seamlessly into the patient’s bite pattern without causing interference or traumatic contact with surrounding soft tissues.
Radiographic evaluation confirms complete root development and appropriate positioning within the alveolar bone. Full eruption eliminates the risk of operculitis (inflammation of overlying gum tissue) and reduces bacterial accumulation in partially covered areas. Patients with sufficient arch length and normal jaw development typically accommodate fully erupted wisdom teeth without compromising adjacent dental structures.
Clinical examination reveals normal crown morphology, intact enamel surfaces, and healthy gingival margins surrounding completely erupted third molars. These favorable anatomical conditions indicate successful integration into the oral environment and predict long-term stability without pathological complications.
Healthy Periodontal Environment
The preservation of wisdom teeth requires maintenance of healthy supporting structures, including gingival tissues, periodontal ligament, and alveolar bone. Periodontal probing depths measuring 3mm or less around third molars indicate stable attachment levels and absence of pathological pocket formation. Healthy gingival tissues exhibit pink coloration, firm consistency, and minimal bleeding upon gentle probing.
Radiographic assessment demonstrates normal bone architecture surrounding wisdom tooth roots, with intact lamina dura and appropriate trabecular patterns. Absence of horizontal or vertical bone loss, furcation involvement, or periapical pathology supports the decision to retain these teeth. Longitudinal monitoring confirms stable periodontal parameters over extended observation periods.
Bacterial sampling from the gingival sulcus around retained wisdom teeth should reveal normal oral flora without pathogenic species associated with progressive periodontal disease. Inflammatory biomarkers such as interleukin-1β and prostaglandin E2 remain within physiological ranges, indicating absence of active tissue destruction or chronic inflammatory processes.
Accessible Oral Hygiene Maintenance
Successful long-term retention of wisdom teeth depends critically on the patient’s ability to maintain effective oral hygiene in posterior regions of the mouth. Adequate mouth opening (minimum 35-40mm interincisal distance) permits proper toothbrush and floss access to third molar surfaces. Patients must demonstrate proficiency in cleaning techniques specific to posterior teeth, including angled brushing strokes and interdental cleaning methods.
The spatial relationship between wisdom teeth and the ascending ramus of the mandible influences accessibility for oral hygiene procedures. Sufficient buccal and lingual space allows for effective plaque removal without excessive difficulty or discomfort. Patients with limited manual dexterity, cognitive impairments, or physical disabilities may require modified oral hygiene protocols or professional assistance to maintain adequate cleanliness.
Regular assessment of plaque accumulation patterns, gingival inflammation indices, and calculus formation around retained wisdom teeth provides objective evidence of hygiene maintenance success. Patients demonstrating consistent oral cleanliness and minimal plaque retention can safely maintain their third molars with appropriate professional support and monitoring.
Asymptomatic Status and Absence of Pathology
The most fundamental criterion for wisdom tooth retention involves complete absence of symptoms and pathological conditions. Asymptomatic third molars cause no pain, swelling, dysfunction, or discomfort during normal oral activities including mastication, speaking, and oral hygiene procedures. Patients report no awareness of these teeth during daily function, indicating successful integration into the oral environment.
Clinical examination reveals no evidence of caries, pericoronitis, abscess formation, or soft tissue ulceration associated with retained wisdom teeth. Surrounding tissues appear healthy with normal coloration, texture, and response to palpation. Absence of lymphadenopathy, trismus, or extraoral swelling confirms lack of infectious or inflammatory processes.
Radiographic imaging demonstrates normal bone patterns, intact tooth structure, and appropriate spatial relationships with adjacent dental and anatomical structures. No evidence of cyst formation, external root resorption, or damage to neighboring second molars supports the decision for continued retention with regular monitoring protocols.
The Potential Downsides of Unnecessary Extraction
Surgical Complications and Nerve Injury Risks
Routine wisdom tooth extraction carries inherent surgical risks that can result in significant morbidity, particularly involving sensory nerve damage. The inferior alveolar nerve, which provides sensation to the lower lip, chin, and teeth, courses through the mandibular canal in close proximity to mandibular third molar roots. Surgical trauma during extraction can cause temporary or permanent paresthesia affecting these anatomical regions.
Lingual nerve injury represents another serious complication, resulting in altered sensation to the tongue, floor of the mouth, and lingual gingiva. This nerve lies in immediate contact with the lingual cortical plate near mandibular wisdom teeth, making it vulnerable to laceration, compression, or stretching during surgical procedures. Recovery from lingual nerve injury often proves incomplete, leaving patients with permanent sensory deficits.
| Complication Type | Incidence Rate | Duration | Recovery Likelihood |
|---|---|---|---|
| Inferior Alveolar Nerve Injury | 0.5-5.3% | Temporary: 2-6 months | 95-98% |
| Lingual Nerve Injury | 0.1-2.0% | Permanent: >6 months | 60-80% |
| Dry Socket (Alveolar Osteitis) | 2-5% | 5-10 days | 100% with treatment |
| Post-operative Infection | 1-3% | 7-14 days | 98% with antibiotics |
| Excessive Bleeding | 0.5-1% | 24-48 hours | 99% with intervention |
Infectious Complications and Healing Disorders
Post-surgical infections following wisdom tooth extraction can range from localized alveolar osteitis to severe fascial space involvement requiring hospitalization. Dry socket (alveolar osteitis) occurs when the blood clot fails to form properly or becomes dislodged, exposing underlying bone and nerve endings to oral bacteria and debris. This condition causes severe, throbbing pain that typically develops 2-4 days post-operatively and may persist for several weeks without appropriate intervention.
Deeper infections can spread through anatomical fascial planes, potentially causing Ludwig’s angina, parapharyngeal space involvement, or descending necrotizing fasciitis. These life-threatening complications require immediate antibiotic therapy, surgical drainage, and often intensive care management. Risk factors include immunocompromised status, diabetes mellitus, smoking, and poor oral hygiene.
Secondary complications from post-extraction infections include osteomyelitis of the jawbone, pathological fractures through weakened extraction sites, and chronic draining sinuses requiring extensive reconstructive procedures. The financial and personal costs of managing these complications far exceed the original extraction fees, highlighting the importance of appropriate case selection.
Anesthetic Complications and Medical Risks
Wisdom tooth extraction often requires local anesthesia supplemented with sedation or general anesthesia, particularly for complex surgical cases. Allergic reactions to local anesthetics, though rare, can range from mild skin reactions to life-threatening anaphylaxis requiring emergency medical intervention. Cardiovascular complications include cardiac arrhythmias, hypertension, and myocardial ischemia in susceptible patients.
Sedation-related complications encompass respiratory depression, airway obstruction, and aspiration pneumonia. Patients with underlying medical conditions such as sleep apnea, cardiac disease, or pulmonary disorders face elevated risks during sedated dental procedures. Pre-operative medical clearance and appropriate monitoring protocols help minimize these risks but cannot eliminate them entirely.
General anesthesia complications, while uncommon, include malignant hyperthermia, cardiac arrest, brain injury from hypoxia, and death. The mortality rate for outpatient oral surgery under general anesthesia approximates 1 in 400,000 procedures, making risk-benefit analysis crucial for elective wisdom tooth removal. Patients requiring general anesthesia for routine extractions may be better served by retention with appropriate monitoring.
Recovery Period Challenges and Quality of Life Impact
The post-operative recovery period following wisdom tooth extraction significantly impacts patients’ daily activities, work productivity, and overall quality of life. Swelling typically peaks 48-72 hours after surgery, often limiting mouth opening, speaking ability, and nutritional intake. Patients frequently require 3-7 days away from work or school, affecting academic performance and earning potential.
Pain management during recovery often requires prescription opioid medications, contributing to the ongoing opioid crisis and risk of dependency. Gastrointestinal side effects from pain medications and antibiotics can prolong recovery and create additional discomfort. Dietary restrictions limiting patients to soft foods for 1-2 weeks can result in nutritional deficiencies and weight loss, particularly problematic for elderly patients or those with underlying health conditions.
Sleep disruption from post-operative pain and discomfort affects healing, immune function, and psychological well-being. Many patients report anxiety, depression, and frustration during extended recovery periods, particularly when complications develop or healing progresses slower than anticipated. These psychosocial impacts often receive insufficient attention in treatment planning discussions.
When Removal IS Still Recommended
Problematic Impaction Patterns and Associated Complications
Wisdom tooth impaction occurs when insufficient space prevents normal eruption, resulting in the tooth becoming trapped beneath gingival tissues or against adjacent dental structures. Different impaction patterns present varying degrees of clinical significance and intervention requirements. Angular impaction, where the tooth tilts toward the second molar, creates food traps and cleaning difficulties that promote bacterial accumulation and tissue inflammation.
Horizontal impaction represents the most problematic configuration, with the wisdom tooth lying perpendicular to normal eruption paths. This positioning frequently causes external root resorption of adjacent second molars, potentially compromising their long-term viability. Bony impaction involves teeth completely encased within alveolar bone, while soft tissue impaction allows partial crown exposure through overlying gingiva.
Types of Wisdom Tooth Impaction:
- Mesial Angular Impaction: Tooth angled toward second molar (most common)
- Distal Angular Impaction: Tooth angled away from second molar
- Horizontal Impaction: Tooth lying sideways (highest complication rate)
- Vertical Impaction: Upright position but insufficient eruption space
- Bony Impaction: Complete bone coverage preventing eruption
- Soft Tissue Impaction: Partial gingival coverage allowing bacterial entry
Pericoronitis represents the most frequent complication associated with partially erupted wisdom teeth, involving inflammation of the operculum (overlying gum tissue). This condition typically manifests as pain, swelling, difficulty opening the mouth, and sometimes fever or lymphadenopathy. Recurrent episodes of pericoronitis indicate the need for surgical intervention, as conservative management with antibiotics and irrigation provides only temporary relief.
Irreparable Decay and Endodontic Complications
Wisdom teeth developing extensive caries that cannot be effectively restored require extraction rather than complex endodontic treatment. The posterior location of third molars creates significant access challenges for conventional restorative procedures, often resulting in suboptimal treatment outcomes and high failure rates. Deep carious lesions approaching or involving the pulp chamber typically necessitate root canal therapy, which proves technically difficult and expensive for wisdom teeth.
The complex root anatomy of wisdom teeth, including curved or dilacerated roots, multiple canals, and accessory foramina, complicates endodontic treatment and reduces success rates compared to anterior and premolar teeth. Limited mouth opening and restricted visibility further compromise the ability to achieve adequate disinfection and obturation of the root canal system.
Recurrent caries around existing restorations in wisdom teeth often indicates poor oral hygiene access and ongoing bacterial challenge. Multiple restoration failures, particularly involving large composite restorations or crowns, suggest that long-term maintenance will prove difficult and expensive. In these cases, extraction provides a more predictable solution than repeated restorative interventions.
Adjacent Tooth Damage and Bone Pathology
Wisdom teeth causing damage to neighboring second molars through external root resorption, caries initiation, or periodontal destruction require prompt removal to preserve the more functionally important adjacent teeth. Pressure from impacted third molars can create root surface defects in second molars that compromise their structural integrity and long-term prognosis.
Cyst formation around impacted wisdom teeth, including dentigerous cysts, odontogenic keratocysts, and ameloblastomas, necessitates surgical intervention to prevent expansion and destruction of surrounding bone structures. These pathological lesions can grow to considerable size, potentially causing pathological fractures, nerve displacement, or involvement of adjacent anatomical structures such as the maxillary sinus or inferior alveolar canal.
| Pathological Condition | Treatment Urgency | Associated Complications | Removal Necessity |
|---|---|---|---|
| External Root Resorption | Immediate | Second molar loss | Mandatory |
| Dentigerous Cyst | Urgent | Bone destruction, nerve damage | Mandatory |
| Odontogenic Keratocyst | Urgent | High recurrence, aggressive growth | Mandatory |
| Severe Periodontal Disease | Moderate | Adjacent tooth involvement | Usually required |
| Recurrent Pericoronitis | Moderate | Systemic infection risk | Often required |
Extensive bone loss around wisdom teeth from chronic periodontal disease can affect the supporting structures of adjacent second molars, creating treatment challenges that extend beyond the third molar itself. Advanced periodontitis with deep pocket formation, furcation involvement, and mobility typically indicates irreversible damage requiring extraction to prevent further progression.
Orthodontic Treatment Considerations
Specific orthodontic treatment scenarios may require wisdom tooth removal to achieve optimal treatment outcomes or maintain post-treatment stability. Patients with severe crowding requiring significant arch expansion or posterior tooth movement may benefit from third molar extraction to create additional space for tooth alignment. This consideration proves particularly relevant in cases involving orthognathic surgery where precise occlusal relationships are critical.
Impacted wisdom teeth that interfere with orthodontic tooth movement or appliance placement may require removal during active treatment phases. The presence of third molars can complicate molar uprighting procedures, distalization movements, and space closure in extraction cases. Orthodontists may recommend prophylactic extraction when wisdom teeth are likely to interfere with planned tooth movements.
Post-orthodontic stability concerns occasionally justify wisdom tooth removal, particularly in patients with pre-existing crowding tendencies or narrow arch forms. However, current evidence suggests that wisdom teeth contribute minimally to post-treatment relapse, and their removal solely for retention purposes lacks strong scientific support. Individual risk assessment considering multiple factors provides better guidance than blanket recommendations.
What to Do If You Keep Your Wisdom Teeth
Establishing Effective Oral Hygiene Protocols
Maintaining optimal oral health with retained wisdom teeth requires specialized cleaning techniques adapted to posterior oral anatomy and access limitations. Standard toothbrushing methods often prove inadequate for third molar cleaning, necessitating modified approaches using angled brushes, interdental aids, and supplementary antimicrobial agents. Patients must master techniques for reaching distal and lingual surfaces of wisdom teeth where plaque accumulation typically occurs.
Electric toothbrushes with oscillating or sonic technology demonstrate superior plaque removal efficacy around posterior teeth compared to manual brushing techniques. The compact brush heads and enhanced cleaning action help compensate for limited access and visibility in third molar regions. Interdental brushes, water flossers, and antimicrobial mouth rinses provide additional cleaning benefits for maintaining gingival health around retained wisdom teeth.
Essential Oral Hygiene Tools for Wisdom Tooth Maintenance:
- Compact-head electric toothbrush – Enhanced cleaning in restricted spaces
- Interdental brushes – Remove plaque between teeth and under gum line
- Water flosser – Irrigate hard-to-reach areas with pulsating water
- Antimicrobial mouthwash – Reduce bacterial load and inflammation
- Single-tuft brush – Target specific areas around individual teeth
- Fluoride gel – Strengthen enamel and prevent decay
Professional demonstration of proper cleaning techniques ensures patients develop effective habits for long-term success. Dental hygienists can identify individual challenges and customize oral hygiene protocols based on each patient’s anatomical configuration, manual dexterity, and compliance factors. Regular reinforcement and technique refinement help maintain optimal cleaning effectiveness over time.
Implementing Regular Professional Monitoring
Retained wisdom teeth require systematic professional evaluation at intervals determined by individual risk factors and clinical findings. Standard six-month dental examinations may prove insufficient for patients with challenging third molar anatomy or hygiene limitations. High-risk patients may benefit from three-month professional monitoring to detect early pathological changes before they progress to irreversible damage.
Comprehensive examinations should include visual inspection, periodontal probing, radiographic assessment, and documentation of any changes from baseline conditions. Dental professionals must maintain detailed records of third molar status, including pocket depths, bleeding indices, plaque accumulation patterns, and patient-reported symptoms. This longitudinal data provides essential information for making informed decisions about continued retention versus extraction.
Professional cleaning appointments should emphasize thorough debridement around wisdom teeth, including subgingival scaling and root planing when indicated. Fluoride applications, antimicrobial treatments, and oral hygiene reinforcement help maintain optimal conditions for continued retention. Patients benefit from regular professional assessment of their home care effectiveness and technique modifications as needed.
Recognizing Warning Signs and Seeking Prompt Care
Patient education regarding symptoms that may indicate developing problems with retained wisdom teeth enables early intervention and prevents progression to serious complications. Pain, swelling, bleeding, or discharge around third molars requires prompt professional evaluation to determine appropriate treatment. Changes in taste, difficulty opening the mouth, or swelling extending beyond the immediate tooth area may indicate spreading infection requiring urgent care.
Persistent bad breath or taste specifically associated with wisdom tooth areas often indicates bacterial accumulation or tissue breakdown that may not be visible during routine self-examination. Patients should report any changes in sensation, including numbness or tingling, as these symptoms may indicate nerve involvement or developing pathology requiring immediate attention.
Regular self-monitoring using proper lighting and mirrors helps patients detect early changes in tissue appearance, tooth position, or functional difficulties. Any concerns about wisdom tooth health warrant professional consultation rather than attempting self-treatment or ignoring symptoms. Early intervention typically proves more conservative and successful than delayed treatment of advanced problems.
Rethinking Wisdom Tooth Extraction: A Personalized Approach
The modern approach to wisdom tooth management represents a fundamental shift from routine prophylactic extraction toward individualized, evidence-based decision-making. Contemporary dental professionals now recognize that asymptomatic, properly positioned third molars rarely cause the complications once feared, while unnecessary surgical intervention exposes patients to avoidable risks, costs, and recovery challenges. This evolution in clinical thinking reflects broader advances in evidence-based medicine and patient-centered care principles.
The key factors supporting retention of healthy wisdom teeth include complete eruption with functional integration, maintenance of healthy periodontal tissues, accessibility for effective oral hygiene, and absence of pathological conditions. When these criteria are met, patients can successfully maintain their third molars throughout adulthood with appropriate professional monitoring and home care protocols. Conversely, extraction remains indicated for problematic impaction, irreparable decay, adjacent tooth damage, or documented pathology requiring surgical intervention.
Successful management of retained wisdom teeth depends on establishing effective oral hygiene routines, implementing regular professional monitoring, and maintaining vigilance for warning signs of developing problems. Patients who demonstrate commitment to optimal oral health practices and regular professional care can expect excellent long-term outcomes with their retained third molars.
The decision regarding wisdom tooth retention versus extraction requires personalized evaluation by qualified dental professionals, including general dentists, periodontists, and oral and maxillofacial surgeons. Individual assessment considering anatomical factors, risk profile, oral hygiene capacity, and patient preferences provides the foundation for developing appropriate treatment plans. This collaborative approach ensures that each patient receives care tailored to their specific needs and circumstances, optimizing both immediate and long-term oral health outcomes.
Frequently asked questions about “Why Experts Now Say Not To Remove Your Wisdom Teeth”
1. “I thought everyone had to get their wisdom teeth removed. Why are experts now saying it’s not always necessary?”
Answer: “The shift in expert opinion is largely due to a lack of strong evidence supporting routine prophylactic (preventive) removal of asymptomatic, disease-free wisdom teeth. Many years ago, it was common practice to remove them to prevent potential future problems. However, current thinking emphasizes that, like any surgical procedure, wisdom tooth extraction carries risks (such as pain, swelling, infection, and nerve injury). If wisdom teeth are healthy, properly erupted, functional, and can be kept clean, the benefits of removal may not outweigh these risks. Experts now advocate for a more individualized assessment.”
2. “So, if not everyone needs them out, when is wisdom tooth removal still recommended?”
Answer: “Wisdom tooth removal is still strongly recommended in several situations. These include:
* Pain, Infection, or Recurrent Inflammation: If they are causing pericoronitis (inflammation of the gum tissue around a partially erupted tooth) or other infections.
* Cysts or Tumors: If a cyst or tumor has developed around the wisdom tooth.
* Damage to Adjacent Teeth: If an impacted wisdom tooth is damaging the roots or structure of the neighboring molar.
* Significant Tooth Decay or Gum Disease: If the wisdom tooth itself has extensive decay or gum disease that cannot be effectively treated.
3. “What are the potential risks of keeping my wisdom teeth if they aren’t causing problems now?”
Answer: “Even if asymptomatic now, there are potential risks to monitor if you keep your wisdom teeth, especially if they are impacted or difficult to clean:
* Future Impaction Problems: They might still cause crowding or damage to adjacent teeth later on.
* Increased Risk of Decay: Wisdom teeth are far back in the mouth and can be hard to brush and floss effectively, making them prone to cavities.
* Gum Disease (Pericoronitis/Periodontitis): Difficulty cleaning can lead to gum inflammation or more severe periodontal disease around the wisdom tooth and potentially affecting adjacent teeth.
* Cyst Development: Though less common, cysts can form around impacted teeth silently and may only be detected on an X-ray.
This is why regular dental check-ups and X-rays are crucial if you decide to keep your wisdom teeth, so any emerging issues can be caught early.”
4. “What are the benefits of avoiding unnecessary wisdom tooth removal?”
Answer: “The primary benefits of avoiding unnecessary wisdom tooth removal include:
* Avoiding Surgical Risks: You bypass the potential complications associated with surgery, such as pain, swelling, bruising, infection, dry socket, and temporary or (rarely) permanent nerve damage leading to numbness of the lip, chin, or tongue.
* Cost Savings: Surgical extraction can be expensive, especially if not fully covered by insurance.
* No Recovery Time: You avoid the discomfort and time off work or school typically needed for recovery.
* Preserving Healthy Teeth: If your wisdom teeth are healthy, erupted correctly, and functional, they can contribute to chewing and overall dental structure.
* Reduced Antibiotic Use: Avoiding surgery means avoiding the potential need for antibiotics, which contributes to mitigating antibiotic resistance.”
5. “How can I determine if my wisdom teeth need to be removed, given this new perspective?”
Answer: “The decision should be made on an individual basis in consultation with your dentist or an oral surgeon. They will:
* Perform a Clinical Examination: Assess the current state of your wisdom teeth and surrounding gums.
* Take X-rays (e.g., panoramic X-ray): To see the position, development, and angulation of your wisdom teeth, and their relationship to adjacent teeth and nerves.
* Discuss Your Symptoms (if any): Any pain, swelling, or difficulty cleaning.
* Assess Your Oral Hygiene: How well you can clean the area.
* Evaluate Risk vs. Benefit: They will weigh the potential risks of keeping the teeth against the risks and benefits of removing them in your specific situation.
References
https://onedentaluk.com/why-experts-now-say-not-to-remove-your-wisdom-teeth/
https://damorelaw.com/the-real-risks-of-wisdom-tooth-removal/
https://www.theoralsurgerygroup.com/https-www-theoralsurgerygroup-com-early-wisdom-teeth-removal/
https://crystallinedental.com/why-experts-now-say-not-to-remove-your-wisdom-teeth/
https://eyeanddentalclinic.com/blog/why-experts-now-say-not-to-remove-your-wisdom-teeth/
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.