Sudden excessive saliva production—medically termed hypersalivation, sialorrhea, or ptyalism—represents a complex physiological response that can transform from a minor inconvenience into a significant health concern affecting millions worldwide. This phenomenon occurs when salivary glands produce substantially more saliva than the typical 0.5-1.5 liters daily, sometimes reaching up to 8 cups per day, or when the body struggles to clear normal saliva volumes effectively from the oral cavity.
“Why is my mouth producing so much saliva suddenly?“- This comprehensive guide explores the multifaceted causes behind unexpected increases in salivary flow, ranging from temporary dietary triggers and medication-induced side effects to serious underlying pathologies including gastroesophageal reflux disease (GERD), neurological disorders, and systemic infections. We’ll examine diagnostic approaches, evidence-based treatment modalities, potential complications, and when immediate medical intervention becomes necessary. Additionally, this article provides practical management strategies, interdisciplinary care considerations, and emerging therapeutic developments to help patients and healthcare providers navigate this challenging condition effectively.
Understanding Normal vs. Excessive Saliva Production
Normal salivary function serves four critical physiological roles: facilitating digestion through enzyme-rich secretions, maintaining oral hygiene by washing away pathogenic bacteria and food debris, enhancing gustatory perception by dissolving flavor compounds, and lubricating oral tissues for proper articulation during speech. The human oral cavity contains three major salivary glands—parotid, submandibular, and sublingual—alongside numerous minor glands that collectively maintain optimal moisture levels.
Hypersalivation manifests in two distinct patterns: anterior sialorrhea, characterized by saliva spilling forward and causing visible drooling, and posterior sialorrhea, where excess saliva flows backward toward the pharynx and potentially into respiratory pathways. This condition can present as either acute (lasting days to weeks) or chronic (persisting months to years), depending on underlying etiology and individual patient factors.
The distinction between physiological adaptation and pathological overproduction requires careful clinical assessment, as temporary increases following spicy meals or during pregnancy represent normal homeostatic responses, while persistent hypersalivation often signals deeper medical issues requiring professional evaluation and targeted therapeutic intervention.
Common Causes of Sudden Excessive Saliva Production
Dietary and Environmental Triggers
Specific food categories consistently stimulate enhanced salivary gland activity through well-established physiological mechanisms. Acidic foods including citrus fruits, tomatoes, and vinegar-based products trigger compensatory alkaline saliva production to neutralize potentially harmful acid levels and protect enamel integrity. Similarly, capsaicin-containing spicy foods activate thermoreceptors, prompting cooling salivary responses, while high-sugar content stimulates digestive enzyme secretion in preparation for carbohydrate metabolism.
These dietary-induced changes typically resolve within 30-60 minutes post-consumption and represent adaptive responses rather than pathological conditions. However, individuals with gastroesophageal reflux disease may experience prolonged hypersalivation following trigger food consumption due to compromised esophageal function and persistent acid exposure.
Medication-Induced Hypersalivation
Pharmaceutical agents represent a frequently overlooked yet significant contributor to sudden-onset excessive salivation through various mechanisms including cholinergic stimulation, tissue irritation, and altered neuromuscular coordination affecting swallowing reflexes.
| Medication Class | Common Examples | Mechanism of Action | Management Approach |
|---|---|---|---|
| Antipsychotics | Haloperidol, Clozapine, Olanzapine | Dopamine receptor blockade affecting neural control | Dosage adjustment, alternative agents |
| Anti-seizure medications | Phenytoin, Carbamazepine, Valproate | Gingival hyperplasia, altered neural signaling | Dental consultation, medication switching |
| Sedatives | Benzodiazepines, Barbiturates | Muscle relaxation affecting swallowing | Gradual tapering, swallowing therapy |
| Antibiotics | Doxycycline, Tetracycline | Esophageal irritation, altered oral flora | Take with food, probiotic supplementation |
Healthcare providers must carefully evaluate medication regimens when patients present with new-onset hypersalivation, considering both direct pharmacological effects and indirect consequences such as altered consciousness levels affecting saliva clearance mechanisms.
Infectious and Inflammatory Conditions
The body’s immune response to oral and systemic infections frequently includes increased salivary production as a protective mechanism designed to flush pathogenic organisms and provide antimicrobial compounds including lysozyme, lactoferrin, and immunoglobulin A.
Common infectious causes include:
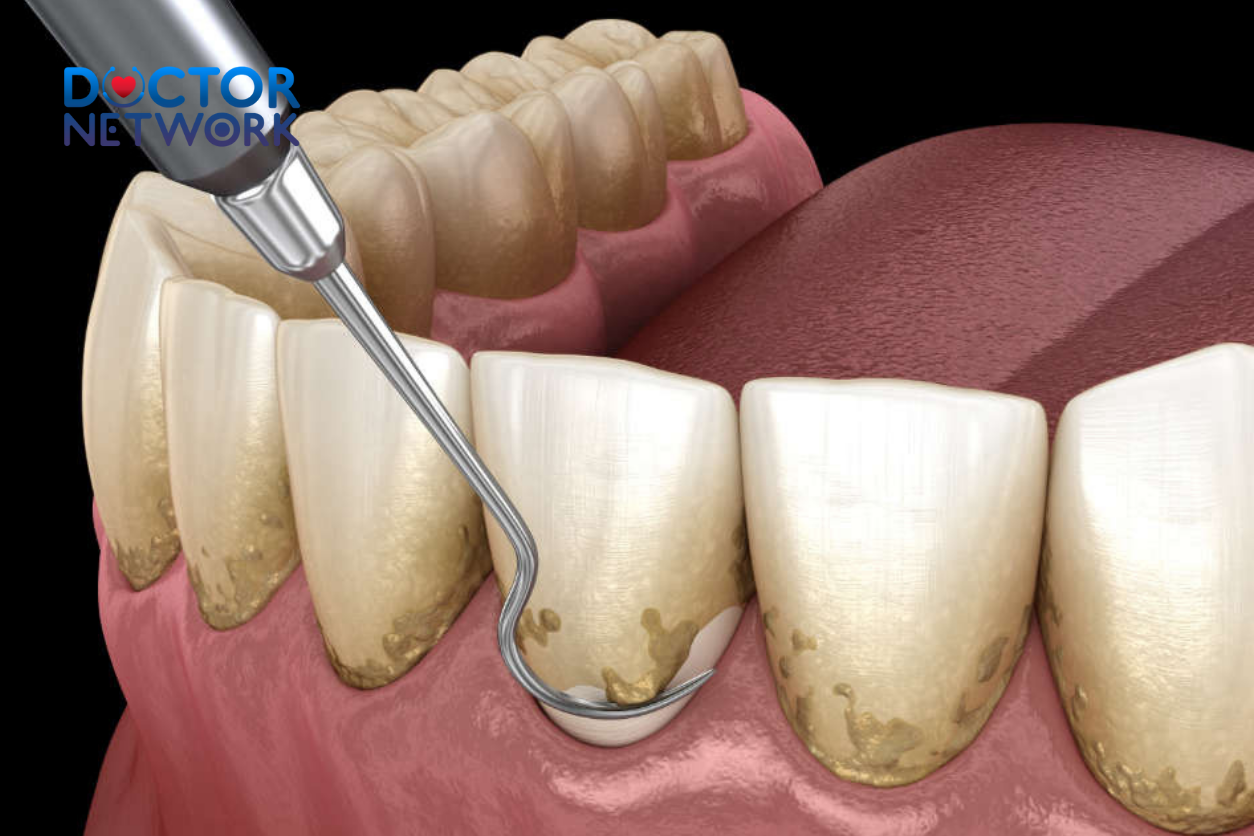
- Dental infections: Caries, periodontal abscesses, and gingivitis create localized inflammation triggering regional hypersalivation
- Upper respiratory infections: Streptococcal pharyngitis, viral tonsillitis, and sinusitis with post-nasal drainage
- Oral fungal infections: Candida albicans overgrowth (thrush) particularly in immunocompromised patients
- Systemic viral infections: Epstein-Barr virus, cytomegalovirus, and influenza affecting salivary gland function
These infection-related cases typically present with accompanying symptoms including fever, pain, lymphadenopathy, and characteristic oral lesions, facilitating differential diagnosis and targeted antimicrobial therapy.
Gastroesophageal Reflux Disease (GERD)
GERD represents one of the most common yet underrecognized causes of chronic hypersalivation, affecting approximately 20% of adults in developed countries. The pathophysiology involves retrograde gastric acid flow into the esophagus and potentially the oral cavity, triggering protective salivary hypersecretion to neutralize acid and protect mucosal surfaces from chemical injury.
Patients with GERD-associated hypersalivation typically experience symptom exacerbation following meals, when lying flat, or during periods of increased intra-abdominal pressure. Associated manifestations include heartburn, regurgitation, chronic cough, hoarseness, and dental enamel erosion from repeated acid exposure.
Neurological Disorders Affecting Salivary Control
Neurological conditions disrupt the complex neural networks controlling both salivary production and clearance mechanisms, leading to apparent hypersalivation that may actually represent impaired swallowing rather than increased production.
| Neurological Condition | Primary Mechanism | Associated Features | Treatment Considerations |
|---|---|---|---|
| Parkinson’s Disease | Reduced swallowing frequency, bradykinesia | Tremor, rigidity, bradykinesia | Dopaminergic medications, swallowing therapy |
| Cerebral Palsy | Generalized motor dysfunction | Spasticity, developmental delays | Multidisciplinary approach, adaptive devices |
| Stroke | Unilateral weakness, dysphagia | Facial droop, speech difficulties | Rehabilitation, positioning strategies |
| Multiple Sclerosis | Demyelination affecting cranial nerves | Fatigue, vision changes, weakness | Disease-modifying therapies, symptom management |
| Motor Neuron Disease | Progressive muscle weakness | Fasciculations, atrophy, respiratory compromise | Supportive care, advanced directives |
These conditions require specialized neurological assessment and often benefit from interdisciplinary management approaches combining medical therapy, rehabilitation services, and adaptive strategies.
Pregnancy-Related Hypersalivation (Ptyalism Gravidarum)
Pregnancy-associated excessive salivation affects approximately 2.4% of pregnant women, typically manifesting during the first trimester and correlating with hormonal fluctuations, particularly elevated estrogen and progesterone levels. The condition often accompanies hyperemesis gravidarum and heightened sensory sensitivity to tastes and odors.
Ptyalism gravidarum usually resolves spontaneously following delivery but can significantly impact quality of life during pregnancy, requiring supportive management and reassurance regarding its temporary nature. Severe cases may necessitate medical intervention to prevent dehydration and nutritional deficiencies.
Dental and Oral Structural Issues
Various dental conditions and oral appliances can trigger reactive hypersalivation through mechanical irritation, altered oral anatomy, or compromised swallowing mechanics. New dentures, orthodontic appliances, and oral piercings commonly cause temporary increases in saliva production as the oral tissues adapt to foreign objects.
Malocclusion, macroglossia (enlarged tongue), and temporomandibular joint disorders can impair normal saliva clearance mechanisms, creating a perception of excess production when the actual issue involves inadequate drainage or swallowing efficiency.
Toxin Exposure and Poisoning
Acute-onset severe hypersalivation can indicate exposure to various toxic substances, representing a medical emergency requiring immediate intervention. The salivary response serves as a protective mechanism attempting to dilute and clear harmful compounds from the oral cavity and upper gastrointestinal tract.
High-risk exposures include:
- Organophosphate pesticides: Cause cholinergic overstimulation
- Heavy metals: Mercury, arsenic, and lead accumulation
- Plant toxins: Mushroom poisoning, particularly Amanita species
- Venomous bites: Snake envenomation, spider bites affecting cholinergic pathways
- Chemical vapors: Industrial solvents, cleaning agents, and fumigants
These cases require immediate medical evaluation, toxicological assessment, and specific antidotal therapy when available.

Symptoms and Complications of Excessive Salivation
Physical Manifestations
Hypersalivation produces a constellation of physical symptoms that can significantly impact patient comfort and daily functioning. Primary manifestations include visible drooling with saliva spillage from the mouth, constant swallowing sensations, and the persistent feeling of oral cavity fullness despite repeated attempts at saliva clearance.
Chronic moisture exposure causes perioral skin irritation, including erythema, maceration, and secondary bacterial infections around the mouth and chin area. Patients frequently develop chapped lips, angular cheilitis, and contact dermatitis from constant saliva contact with facial skin surfaces.
Functional Impairments
Speech articulation becomes compromised when excess saliva interferes with precise tongue movements and sound production. Patients report slurred speech, difficulty with certain phonemes, and social embarrassment during conversations requiring clear communication.
Mastication and deglutition processes suffer as excessive saliva dilutes taste sensations and creates swallowing coordination challenges. Food bolus formation becomes difficult, potentially leading to inadequate nutrition and meal-related anxiety.
| Functional Domain | Specific Impairments | Severity Indicators | Intervention Targets |
|---|---|---|---|
| Speech | Articulation errors, wet speech sounds | Intelligibility ratings, listener comprehension | Speech therapy, oral motor exercises |
| Swallowing | Delayed initiation, aspiration risk | Videofluoroscopy findings, pneumonia history | Swallowing rehabilitation, texture modification |
| Social interaction | Withdrawal, communication avoidance | Quality of life scores, participation levels | Counseling, adaptive strategies |
Serious Health Complications
Aspiration pneumonia represents the most serious complication of severe hypersalivation, particularly in patients with concurrent neurological conditions affecting protective reflexes. Inadvertent inhalation of saliva or food particles can trigger life-threatening lung infections requiring aggressive antibiotic therapy and respiratory support.
Choking episodes occur when patients cannot adequately clear accumulated saliva, especially during sleep or when consciousness is altered. These events can lead to hypoxic episodes and emergency medical interventions.
Sleep disruption affects many patients as excessive saliva causes frequent awakening due to choking sensations, pillow soiling, and positional changes to facilitate drainage. Chronic sleep deprivation compounds underlying neurological conditions and impairs immune function.
Psychosocial Impact
The social stigma associated with visible drooling creates profound emotional distress, leading to decreased self-esteem, social withdrawal, and avoidance of public situations. Patients report feeling embarrassed during meals, conversations, and professional interactions.
Depression and anxiety commonly develop as secondary complications, particularly in patients with progressive neurological conditions where hypersalivation represents visible disease progression. The unpredictable nature of drooling episodes creates anticipatory anxiety and hypervigilance regarding social situations.
Quality of life measurements consistently show significant impairment across multiple domains including physical functioning, emotional well-being, social relationships, and occupational performance among patients with chronic hypersalivation.
Diagnostic Approaches for Hypersalivation
Initial Clinical Assessment
A comprehensive medical history forms the foundation of hypersalivation evaluation, focusing on symptom onset, duration, temporal patterns, and associated manifestations. Clinicians systematically explore potential triggers including recent medication changes, dietary modifications, dental procedures, and concurrent illnesses.
The medication review requires particular attention to timing relationships between drug initiation and symptom onset, with consideration of both prescription pharmaceuticals and over-the-counter preparations. Patients should provide complete lists including supplements, herbal remedies, and recreational substances that might influence salivary function.
Family history assessment identifies hereditary conditions predisposing to hypersalivation, while social history evaluation explores occupational exposures, lifestyle factors, and environmental toxin risks. A detailed dietary history helps identify trigger foods and eating patterns contributing to symptom development.
Physical Examination Techniques
The oral examination systematically evaluates all intraoral structures for signs of infection, inflammation, trauma, or anatomical abnormalities. Dentition assessment includes caries detection, periodontal evaluation, and identification of irritating dental appliances or sharp tooth edges.
Salivary gland palpation assesses for enlargement, tenderness, or masses that might indicate sialadenitis, tumors, or ductal obstruction. Bilateral comparison helps identify unilateral pathology affecting individual glands.
Neurological assessment focuses on cranial nerve function, particularly nerves controlling salivation and swallowing. Evaluation includes facial symmetry, tongue movement, palatal elevation, and protective reflex testing to identify neurological deficits contributing to apparent hypersalivation.
Quantitative Saliva Assessment
Objective saliva measurement provides crucial diagnostic information distinguishing true hypersalivation from impaired clearance mechanisms. Standardized collection methods include unstimulated whole saliva collection over specified time periods, typically 15 minutes, with normal values ranging from 0.3-0.5 ml/minute.
Stimulated saliva testing using citric acid or paraffin wax chewing evaluates glandular reserve capacity and helps differentiate between production and clearance disorders. Results exceeding 1.5 ml/minute suggest true hypersalivation rather than clearance impairment.
Saliva Collection Methods:
- Draining method: Patient leans forward allowing saliva to drain into collection container
- Spitting method: Patient spits accumulated saliva at regular intervals
- Suction method: Continuous aspiration using dental suction for precise measurement
- Cotton roll method: Pre-weighed cotton rolls absorb saliva for gravimetric analysis
Advanced Diagnostic Testing
Blood chemistry panels help identify systemic conditions contributing to hypersalivation including infections, metabolic disorders, and medication toxicity. Complete blood count, comprehensive metabolic panel, and inflammatory markers provide baseline assessment for underlying pathology.
Imaging studies become necessary when structural abnormalities are suspected. Ultrasound evaluation of major salivary glands identifies masses, stones, or inflammatory changes. Magnetic resonance imaging provides detailed soft tissue visualization for complex cases requiring surgical planning.
Videofluoroscopic swallowing studies (VFSS) objectively assess swallowing function and aspiration risk in patients with suspected dysphagia. These studies guide therapeutic decisions regarding diet modifications, positioning strategies, and swallowing rehabilitation approaches.
Neurological testing including electromyography, nerve conduction studies, and specialized movement disorder evaluations help diagnose underlying neurological conditions contributing to hypersalivation through motor control impairments.
Treatment and Management Strategies
Addressing Underlying Conditions
Primary treatment focuses on identifying and managing root causes of hypersalivation rather than merely controlling symptoms. Successful outcomes depend on accurate diagnosis and targeted intervention addressing specific pathophysiological mechanisms.
Infectious conditions require appropriate antimicrobial therapy based on culture results and sensitivity patterns. Dental infections may necessitate root canal therapy, extraction, or periodontal treatment in addition to antibiotic administration.
GERD management involves lifestyle modifications including dietary changes, weight reduction, elevation of the head during sleep, and avoidance of late evening meals. Proton pump inhibitors, H2-receptor antagonists, and prokinetic agents help control acid production and enhance gastric emptying.
Neurological conditions require specialized management approaches tailored to specific diagnoses. Parkinson’s disease treatment includes dopaminergic medications, deep brain stimulation, and comprehensive rehabilitation programs addressing multiple motor symptoms including hypersalivation.
Pharmacological Interventions
Anticholinergic medications represent the primary pharmacological approach for reducing salivary production through muscarinic receptor blockade at the glandular level. These agents effectively decrease saliva volume but require careful monitoring for systemic side effects.
Commonly Used Anticholinergic Agents:
| Medication | Dosage Range | Administration Route | Duration of Action | Primary Side Effects |
|---|---|---|---|---|
| Glycopyrrolate | 1-2 mg BID-TID | Oral, Injectable | 6-8 hours | Dry mouth, constipation, urinary retention |
| Scopolamine | 1.5 mg patch | Transdermal | 72 hours | Drowsiness, confusion, blurred vision |
| Atropine | 0.4-0.6 mg | Sublingual drops | 4-6 hours | Tachycardia, mydriasis, hyperthermia |
| Benztropine | 0.5-1 mg BID | Oral | 8-12 hours | Sedation, cognitive impairment |
Beta-adrenergic antagonists like propranolol can reduce saliva viscosity and improve clearance in some patients, particularly those with anxiety-related hypersalivation. These agents work through different mechanisms than anticholinergics and may be beneficial in combination therapy.
Botulinum Toxin Therapy
Botulinum toxin type A injection into major salivary glands provides effective, targeted treatment for refractory hypersalivation cases. The neurotoxin blocks acetylcholine release at neuromuscular junctions, temporarily paralyzing glandular function without systemic anticholinergic effects.
Ultrasound-guided injection techniques ensure precise toxin delivery to parotid and submandibular glands while avoiding critical neurovascular structures. Treatment effects typically begin within 3-7 days, reach maximum benefit at 2-4 weeks, and last 3-6 months before requiring repeat injections.
Patient selection criteria include failure of conservative management, contraindications to anticholinergic medications, and sufficient life expectancy to justify repeated treatments. Pre-treatment counseling should address realistic expectations, potential side effects, and long-term management commitment.
Surgical Interventions
Surgical options become considerations for severe, medically refractory hypersalivation significantly impairing quality of life despite optimal conservative management. These procedures carry inherent risks and require careful patient selection and informed consent processes.
Surgical Approaches:
- Submandibular gland excision: Complete removal of sublingual and submandibular glands
- Parotid duct ligation: Blocking major salivary duct to redirect flow
- Duct rerouting procedures: Redirecting saliva flow to posterior oral cavity
- Four-gland excision: Complete major salivary gland removal for severe cases
Complications include facial nerve injury, gustatory sweating (Frey’s syndrome), xerostomia, and wound healing problems. Success rates vary from 70-90% depending on procedure type and patient characteristics.
Radiation Therapy
Low-dose radiation therapy to major salivary glands offers an alternative to surgery for high-risk surgical candidates. Fractionated external beam radiation causes glandular atrophy and reduced saliva production with relatively low complication rates.
Treatment typically involves 20-30 Gy delivered in multiple fractions over 2-3 weeks. Side effects include mucositis, taste alterations, and potential long-term xerostomia. Patient selection requires careful risk-benefit analysis considering life expectancy and treatment goals.
Therapeutic Appliances and Rehabilitation
Custom oral appliances can improve saliva management through enhanced lip seal, improved swallowing patterns, and better oral posture. These devices are particularly beneficial for patients with neurological conditions affecting oral motor function.
Types of Oral Appliances:
- Lip closure trainers: Improve perioral muscle strength and coordination
- Palatal training appliances: Enhance tongue-palate contact during swallowing
- Bite blocks: Maintain optimal jaw position for improved swallowing
- Modified dentures: Incorporate saliva collection reservoirs or improved retention
Speech-language pathology intervention focuses on swallowing rehabilitation, oral motor exercises, and compensatory techniques. Treatment approaches include thermal stimulation, effortful swallowing techniques, supraglottic swallow maneuvers, and postural modifications.
Occupational therapy addresses adaptive strategies for daily living activities, positioning recommendations, and environmental modifications to minimize hypersalivation impact on functional independence.
Home Management and Lifestyle Modifications
Oral Hygiene Optimization
Meticulous oral hygiene reduces bacterial overgrowth that can stimulate reactive hypersalivation while preventing secondary complications including halitosis and periodontal disease. Enhanced cleaning protocols become particularly important when excessive saliva creates favorable conditions for microbial proliferation.
Comprehensive Oral Care Regimen:
- Brushing: Fluoride toothpaste, soft-bristled brush, 2-3 times daily minimum
- Flossing: Daily interdental cleaning with appropriate technique
- Antiseptic rinses: Chlorhexidine or cetylpyridinium chloride solutions
- Tongue cleaning: Mechanical removal of bacterial biofilm with tongue scrapers
- Professional maintenance: Increased frequency of dental prophylaxis visits
Patients should avoid alcohol-containing mouthwashes that can cause tissue irritation and potentially worsen hypersalivation through local inflammatory responses.
Dietary Management Strategies
Strategic dietary modifications can significantly reduce hypersalivation triggers while maintaining adequate nutrition and patient satisfaction. The approach requires identifying individual trigger foods and implementing sustainable alternatives.
Foods to Limit or Avoid:
- High-acid content: Citrus fruits, tomatoes, vinegar-based products
- Spicy preparations: Hot peppers, curry, wasabi, hot sauces
- Excessive sugar: Candy, sweetened beverages, desserts
- Artificial sweeteners: Some patients report increased salivation with certain sugar substitutes
Recommended Food Choices:
- Bland, low-acid options: Rice, bananas, plain crackers, mild cheeses
- Room temperature items: Avoiding very hot or cold foods that stimulate reflexes
- Smooth textures: Reducing mechanical stimulation from rough or crunchy foods
- Small, frequent meals: Preventing overwhelming of clearance mechanisms
Hydration and Saliva Management
Paradoxically, maintaining adequate hydration helps dilute excess saliva and facilitates more comfortable swallowing. Small, frequent sips of room-temperature water throughout the day prove more effective than large volume consumption.
Ice chips, sugar-free popsicles, and frozen fruit provide cooling relief while temporarily reducing saliva viscosity. However, extremely cold items may trigger increased production in some individuals, requiring personalized approaches.
Practical Management Techniques:
- Absorption products: Tissues, towels, or specialized saliva-absorbing pads
- Positioning strategies: Sitting upright, slight forward head tilt during meals
- Controlled swallowing: Conscious, deliberate swallowing at regular intervals
- Mouth dabbing: Gentle patting rather than wiping to prevent skin irritation
Stress Reduction and Psychological Support
Anxiety and stress can exacerbate hypersalivation through autonomic nervous system activation and muscle tension affecting swallowing coordination. Comprehensive management addresses both physiological symptoms and psychological impacts.
Relaxation techniques including deep breathing exercises, progressive muscle relaxation, and mindfulness meditation can reduce sympathetic nervous system activation contributing to hypersalivation. Regular practice improves both symptom control and overall quality of life.
Stress Management Approaches:
- Cognitive behavioral therapy: Addressing catastrophic thinking and avoidance behaviors
- Support groups: Connecting with others experiencing similar challenges
- Professional counseling: Individual therapy for depression, anxiety, and adjustment issues
- Biofeedback training: Learning conscious control over autonomic responses
Social skills training helps patients develop confidence in managing symptoms during interpersonal interactions, reducing anticipatory anxiety that can worsen hypersalivation episodes.
When to Seek Professional Help
Emergency Warning Signs
Certain presentations of hypersalivation require immediate medical evaluation due to potential life-threatening complications or underlying serious pathology. Recognition of these warning signs enables appropriate triage and timely intervention.
Seek Immediate Medical Attention for:
- Respiratory distress: Difficulty breathing, choking episodes, cyanosis
- Signs of aspiration: Persistent cough, fever, chest pain following choking
- Suspected poisoning: Known toxin exposure with acute-onset hypersalivation
- Severe dehydration: Despite excessive saliva, signs of fluid loss from vomiting or inability to swallow
- Neurological changes: New weakness, speech difficulties, altered consciousness
Emergency department evaluation includes airway assessment, toxicological screening when indicated, and stabilization of respiratory or cardiovascular complications.
Primary Care Consultation
Patients should schedule primary care evaluation when hypersalivation persists beyond one week without obvious cause or significantly interferes with daily activities including eating, speaking, or sleeping. Early intervention often prevents progression to more severe complications.
The primary care visit should address medication review, basic diagnostic testing, and initial therapeutic trials while determining need for specialist referral. Documentation of symptom patterns, triggers, and functional impact guides treatment decisions.
Preparation for Medical Visits:
- Symptom diary: Daily logs of severity, timing, triggers, and associated symptoms
- Medication list: Complete inventory including over-the-counter and herbal products
- Questions list: Specific concerns about diagnosis, treatment options, and prognosis
- Functional assessment: Impact on work, social activities, and daily living tasks
Specialist Referral Criteria
Complex or refractory cases benefit from subspecialty evaluation to address underlying conditions and access advanced therapeutic options. Referral timing depends on symptom severity, response to initial treatment, and suspected etiology.
Neurology Referral Indications:
- Suspected neurological conditions (Parkinson’s, stroke, MS)
- Progressive symptoms with motor or cognitive changes
- Need for specialized movement disorder evaluation
- Consideration of botulinum toxin therapy
ENT Surgery Consultation:
- Severe, medically refractory symptoms
- Evaluation for surgical intervention
- Salivary gland masses or structural abnormalities
- Complex anatomical issues affecting drainage
Gastroenterology Referral:
- Suspected GERD with inadequate symptom control
- Need for advanced reflux testing or endoscopy
- Evaluation of swallowing disorders
- Consideration of antireflux surgery
Interdisciplinary Care and Prognosis
Team-Based Management Approach
Optimal hypersalivation management often requires coordinated care from multiple healthcare disciplines, each contributing specialized expertise to address different aspects of the condition. This collaborative approach improves outcomes while avoiding fragmented care.
The primary care physician serves as the central coordinator, managing initial evaluation, basic therapeutic trials, and referral decisions while maintaining oversight of the overall treatment plan. Regular communication between team members ensures continuity and prevents conflicting interventions.
Core Team Members:
| Specialty | Primary Contributions | Typical Interventions | Collaboration Points |
|---|---|---|---|
| Primary Care | Initial assessment, medication management | Anticholinergics, lifestyle counseling | Coordinates all referrals and follow-up |
| Neurology | Neurological evaluation, specialized treatments | Botulinum toxin, movement disorder management | Works with primary care on medication interactions |
| Speech Pathology | Swallowing assessment, rehabilitation | Swallowing therapy, compensatory techniques | Collaborates with occupational therapy |
| Dentistry | Oral health, appliance fabrication | Dental treatment, custom oral devices | Coordinates with ENT for complex cases |
| ENT Surgery | Advanced evaluation, surgical options | Gland surgery, duct procedures | Works with anesthesia for surgical planning |
Treatment Outcome Expectations
Prognosis for hypersalivation varies significantly based on underlying etiology, patient factors, and treatment response. Temporary causes typically resolve completely with appropriate intervention, while chronic neurological conditions require ongoing management with realistic goal-setting.
Prognostic Factors:
- Underlying condition: Reversible causes have excellent prognosis
- Disease progression: Degenerative conditions worsen over time
- Treatment adherence: Consistent therapy improves outcomes
- Patient age: Younger patients often have better adaptation
- Social support: Strong support systems enhance coping
Medication therapy success rates range from 60-80% for anticholinergic agents, with side effect tolerance limiting effectiveness in some patients. Botulinum toxin provides 70-90% symptom improvement lasting 3-6 months, requiring repeat treatments for sustained benefit.
Surgical interventions achieve long-term symptom control in 70-85% of appropriately selected patients, though complication rates of 10-20% must be considered in treatment decisions. Patient satisfaction correlates strongly with realistic pre-treatment expectations and comprehensive informed consent.
Long-Term Management Considerations
Chronic hypersalivation management requires regular monitoring, treatment adjustments, and adaptation to changing patient needs over time. Progressive neurological conditions may necessitate escalating interventions as the underlying disease advances.
Follow-Up Schedule Recommendations:
- Initial treatment period: Every 2-4 weeks until symptoms stabilize
- Stable maintenance: Every 3-6 months for medication management
- Botulinum toxin patients: Every 4-6 months for retreatment
- Surgical patients: Regular monitoring for complications and efficacy
Quality of life assessment should be incorporated into routine follow-up visits using validated instruments to objectively measure treatment impact and guide therapeutic decisions. Patient-reported outcome measures provide valuable insights into functional improvement beyond purely clinical parameters.
5 frequently asked questions about “why is my mouth producing so much saliva suddenly”
What causes sudden excessive saliva production?
Sudden excessive saliva production can be caused by infections, dental issues, acid reflux, pregnancy, or neurological conditions.Is sudden excessive saliva production a sign of a medical condition?
Yes, it can be a sign of underlying medical conditions such as infections, neurological disorders, or gastrointestinal problems.How can I reduce sudden excessive saliva production?
You can try chewing sugar-free gum, staying hydrated, avoiding irritants like spicy foods, and practicing good oral hygiene.When should I see a doctor for sudden excessive saliva production?
If the condition persists for more than a few days, is accompanied by pain, difficulty swallowing, or other symptoms, you should see a doctor.Can medications cause sudden excessive saliva production?
Yes, some medications can cause increased saliva production as a side effect, including certain antipsychotics and medications for Alzheimer’s disease.
Conclusion
Sudden excessive saliva production represents a complex medical phenomenon with diverse underlying causes ranging from benign dietary triggers to serious neurological conditions requiring specialized intervention. Understanding the multifaceted nature of hypersalivation empowers patients and healthcare providers to pursue appropriate diagnostic evaluation and evidence-based therapeutic approaches.
The key to successful management lies in accurate identification of root causes rather than merely treating symptoms. Comprehensive assessment including detailed history-taking, physical examination, and appropriate diagnostic testing enables targeted interventions addressing specific pathophysiological mechanisms contributing to excessive salivation.
Modern treatment options provide hope for significant symptom improvement across the spectrum of hypersalivation severity. From simple lifestyle modifications and medications to advanced botulinum toxin therapy and surgical interventions, patients have access to increasingly sophisticated therapeutic approaches tailored to individual needs and circumstances.
Early recognition and prompt professional evaluation remain crucial for optimal outcomes, particularly given the potential for serious complications including aspiration pneumonia and the profound impact on quality of life. The collaborative efforts of interdisciplinary healthcare teams ensure comprehensive care addressing both medical and psychosocial aspects of this challenging condition.
Patients experiencing persistent or concerning hypersalivation should not hesitate to seek medical attention, as timely intervention often prevents progression to more severe complications while providing relief from symptoms that can significantly impair daily functioning and social well-being.
References
Overview of Hypersalivation (Excessive Saliva)
Hypersalivation is the overproduction of saliva. It’s important to distinguish between true hypersalivation (the salivary glands are genuinely producing too much saliva) and pseudo-sialorrhea (the perception of excess saliva due to impaired swallowing or clearance, even with normal saliva production). A sudden onset often points to temporary or acute causes.
General Information Source:
Claim: Hypersalivation can be caused by a wide range of conditions, from benign and temporary issues to more serious underlying diseases. It can result from excessive production or decreased clearance of saliva.
Source: Cleveland Clinic
Author(s): Medical professionals at the Cleveland Clinic (content reviewed by healthcare experts).
Link: https://my.clevelandclinic.org/health/symptoms/23054-hypersalivation
1. Gastrointestinal Causes (Very Common for Sudden Onset)
A. Gastroesophageal Reflux Disease (GERD) / Acid Reflux
This is one of the most frequent causes of sudden, intermittent hypersalivation. The reflux of stomach acid into the esophagus triggers a nerve reflex that stimulates the salivary glands. This specific phenomenon is often called “water brash.”
Claim: Acid in the esophagus stimulates the esophago-salivary reflex, leading to increased saliva production. This saliva is bicarbonate-rich and helps to neutralize the acid and clear it from the esophagus.
Source: Gastroenterology Research and Practice (Scientific Journal)
Author(s): Shaha, M., & Shrestha, S.
Study/Article Title: “Gastroesophageal Reflux Disease: A Review of Typical and Atypical Symptoms”
B. Nausea
Nausea, regardless of its cause (motion sickness, stomach bug, morning sickness), is a powerful trigger for hypersalivation. This is a protective reflex preparing the body for vomiting; the excess saliva helps protect the teeth and esophagus from corrosive stomach acid.
Claim: Nausea is a common trigger for hypersalivation. The mechanism is believed to be a vagal nerve reflex that precedes emesis (vomiting).
Source: Handbook of Clinical Neurology
Author(s): Horn, C. C.
Chapter/Article Title: “Chapter 10 – The neurobiological basis of nausea”
Link: https://www.sciencedirect.com/science/article/pii/B9780444636225000100
2. Pregnancy-Related Causes
Ptyalism Gravidarum
Excessive salivation is a well-known, though not fully understood, symptom of early pregnancy. It is often associated with the nausea and vomiting of morning sickness (hyperemesis gravidarum).
Claim: Ptyalism gravidarum is excessive salivation during pregnancy, affecting a small percentage of pregnant women. Its exact cause is unknown but is thought to be related to hormonal changes and the stimulation of salivary glands by nausea.
Source: Journal of Obstetrics and Gynaecology Canada
Author(s): Promila, Kalra, B., & Kalra, S.
Study/Article Title: “Ptyalism Gravidarum”
Link: https://www.jogc.com/article/S1701-2163(16)35222-2/fulltext
3. Infections and Irritations in the Mouth and Throat
Any inflammation in the oral cavity can trigger a protective increase in saliva production.
Claim: Infections such as tonsillitis, strep throat, peritonsillar abscesses, and even canker sores can cause hypersalivation. The body increases saliva flow to help soothe the area and clear pathogens. Swallowing may also be painful, leading to pooling of normally produced saliva.
Source: Merck Manual (Professional Version)
Author(s): Michael L. Pichichero, MD (Content reviewed by medical experts).
Article Title: “Tonsillopharyngitis”
4. Medication Side Effects
Certain medications are well-known for causing sialorrhea by acting on the nervous system that controls salivation.
Claim: Certain drugs, particularly those with cholinergic properties (which stimulate the parasympathetic nervous system), can cause hypersalivation. Classic examples include clozapine (an antipsychotic) and pilocarpine (used to treat dry mouth and glaucoma).
Source: Journal of Clinical Psychopharmacology
Author(s): Freudenreich, O., & Tran, J.
Study/Article Title: “Drug-Induced Sialorrhea”
Additional Source (General Overview): A review article lists several classes of drugs associated with hypersalivation, including some tranquilizers, anticonvulsants, and antipsychotics.
Source: Australian Prescriber
Link: https://www.nps.org.au/australian-prescriber/articles/drug-induced-sialorrhoea
5. Neurological Conditions
While often associated with chronic rather than sudden hypersalivation, a new diagnosis or a change in a condition could present with this symptom. In these cases, it’s typically pseudo-sialorrhea (impaired swallowing) rather than true overproduction.
Claim: Sialorrhea is a common and disabling symptom in patients with Parkinson’s disease, affecting up to 70-80% of individuals. It is primarily caused by impaired swallowing (dysphagia) and poor oral-motor control, not salivary overproduction.
Source: Movement Disorders Clinical Practice (Scientific Journal)
Author(s): Srivanitchapoom, P., Pandey, S., & Hallett, M.
Study/Article Title: “Drooling in Parkinson’s Disease: A Review”
Note: Other conditions like Amyotrophic Lateral Sclerosis (ALS), stroke, and Bell’s palsy can also cause significant issues with saliva management.
6. Exposure to Toxins
Sudden, severe hypersalivation can be a sign of poisoning.
Claim: Exposure to toxins like mercury, arsenic, and particularly organophosphate insecticides can cause a range of symptoms known as a “cholinergic crisis,” a key feature of which is massive hypersalivation.
Source: Centers for Disease Control and Prevention (CDC)
Author(s): Agency for Toxic Substances and Disease Registry (ATSDR), a part of the CDC.
Article Title: “Medical Management Guidelines for Organophosphates”
Link: https://www.atsdr.cdc.gov/csem/organophosphate/physiologic_effects.html
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.