Childhood obesity is a critical issue not only in developed countries but also in developing nations like Vietnam. The severity of obesity escalates when it occurs in children, leading to long-lasting and substantial consequences on physical, mental, and developmental aspects. The prevalence of childhood obesity is on the rise globally, reaching approximately 17% in the United States. In Vietnam, due to excessive parental care, the obesity rate in children has surged rapidly in recent years. According to the Ministry of Health’s report, the obesity rate in children aged 6 to 11 in urban areas of Ho Chi Minh City is now 12%, while in Hanoi, it is 8-9%. Obesity and its consequences increasingly pose a risk to community health. In this article, let’s explore the causes, consequences, and treatment options for childhood obesity with Associate Professor Doctor Nguyen Anh Tuan.
What is Overweight and Obesity?
According to the World Health Organization (WHO):
– Overweight: A condition where body weight exceeds the normal weight for a given height.
– Obesity: An abnormal or excessive accumulation of fat that negatively impacts the body’s health. In 2013, the American Medical Association officially recognized obesity as a disease.
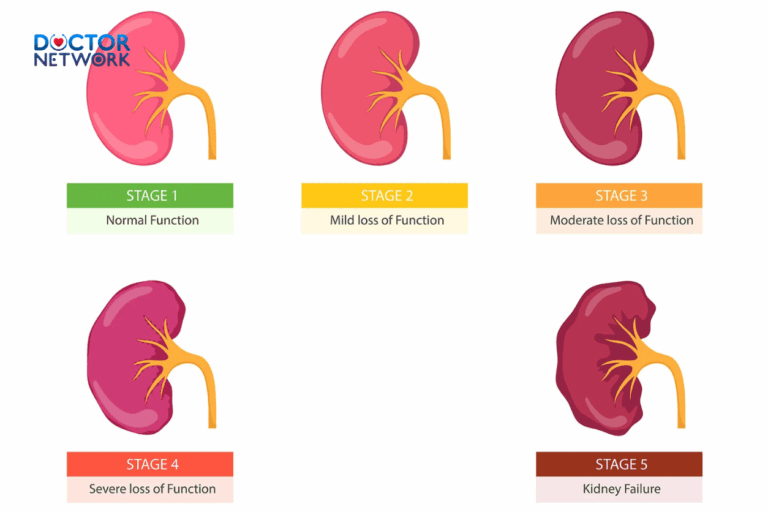
How to Determine Childhood Obesity and Overweight?
BMI (Body Mass Index) is still used for assessment. However, the BMI formula for children considers gender and age, as their bodies are still growing and changing.
– BMI Formula: BMI = Weight (kg) / (Height (m) * Height (m))
– Assessment: Evaluate the nutritional status of children based on the BMI percentile chart according to age.
Early adiposity rebound is a risk factor for childhood obesity. BMI increases rapidly in the first year, then decreases to its lowest point around 6 years (average 6 years) and gradually increases until adulthood. The rebound in BMI during the early years is called early adiposity rebound. Early adiposity rebound before 5.5 years is a risk factor for childhood obesity. Therefore, BMI values before and during the adiposity rebound period must be determined to accurately assess the risk progression.
Types of Childhood Obesity
1. Classification Based on Pathological Causes – type of childhood obesity
- Simple Obesity: Represents more than 90% of cases without clear pathological causes.
- Obesity due to Pathological Conditions: Results from endocrine disorders or genetic defects, accounting for 10%.
2. Classification Based on Onset Age – type of childhood obesity
- Early-Onset Obesity: Appears before the age of 5.
- Late-Onset Obesity: Develops after 5 years of age.
The critical periods for obesity are infancy, 5-7 years, and adolescence. Obesity during these stages increases the risk of ongoing obesity and complications such as a higher risk of heart disease compared to late-onset obesity.

In adolescence, susceptibility to overweight and obesity is heightened
3. Classification Based on Fat Distribution – type of childhood obesity
- Abdominal Obesity (central obesity): Fat concentrates in the abdominal area.
- Thigh Obesity (peripheral obesity): Fat concentrates mainly in the buttocks and thighs.
Abdominal obesity poses a higher risk for heart disease, increased insulin blood levels, lipid disorders, and reduced glucose tolerance compared to thigh obesity.
Common Causes of Childhood Obesity
1. Endocrine-Related Obesity
- Hypothyroidism-Related Obesity: Rare cause (1 in 350). Late-onset obesity, proportional, slow growth, dry skin, constipation, delayed mental development.
- Cushing’s Syndrome Obesity: Caused by adrenal or pituitary tumors or steroid medications. Obese face and body, red or purple stretch marks, early pubic hair development, slow growth.
- Growth Hormone Deficiency-Related Obesity: Regional obesity in the chest area, reduced height velocity. May coexist with anterior pituitary hormone deficiencies like ACTH, TSH, FSH, LH.
- Obesity due to Lesions in the Hypothalamic-Pituitary Area: These lesions induce increased appetite, commonly found in boys.
2. Syndromic Obesity
- Prader-Willi Syndrome: Common and severe cause. Early-onset obesity due to excessive eating starting from 3-4 years, facial dysmorphia (narrow forehead, almond-shaped eyes), small hands and feet, intellectual disability, possible diabetes, and reproductive dysfunction. Most cases result from the deletion of chromosome 15 (50%).
- Laurence-Moon-Biedl Syndrome: Early-onset obesity often accompanied by delayed intellectual development, polydactyly, delayed appearance of retinitis pigmentosa (10-12 years). Reproductive dysfunction due to decreased sex hormone production. Usually, it is an autosomal recessive disorder.
- Astrom Syndrome: Obesity with diabetes, deafness, retinitis pigmentosa, and reproductive dysfunction. Typically, it has a recessive genetic pattern.
- Biemon Syndrome: Obesity with nail deformities, polydactyly, and reproductive dysfunction. Typically, it has a recessive genetic pattern.
- Borjson Syndrome: Obesity, short stature, coarse face, and reproductive dysfunction.
3. External Risk Factors for Obesity
- Family and Genetic Factors: Many cases of obesity have a family history. Children with obese parents may develop obesity at any age; this risk is three times higher in families with obese parents compared to non-obese parents.
- Low Physical Activity: Insufficient physical activity is a source of obesity. Obesity, in turn, leads to a sedentary lifestyle.
- Inadequate Sleep: Studies show that children who sleep less than 8 hours per night have an increased risk of obesity after the age of 15. Inadequate sleep, early bedtime, excessive TV viewing, and reduced physical activity can lead to sleep disturbances in obese children, such as fluctuations in hormone levels like serotonin.
- Breastfeeding as a Protective Factor: Studies consistently show that breastfeeding has a preventive effect against obesity in children. The shorter the duration of breastfeeding, the higher the risk of obesity in young children.
- Psychological and Emotional Factors: Psychological and emotional factors are risk factors for childhood obesity. Lack of care and education from parents during early childhood is a risk factor for obesity.
- Early Puberty and Obesity: Research shows that 30% of overweight girls and 15% of obese girls experience early menstruation before 11 years.
Unhealthy Habits Leading to Childhood Obesity
- Uncontrolled Snacking: Limit or eliminate cookies and French fries at home. Choose healthy snacks like fruits and vegetables, low-fat puddings, yogurt, and cheese. Ensure that your child does not snack all day, even on healthy foods.
- Eating While Watching TV: Lack of focus may lead children to not realize when they are full. Help your child learn to listen to the body’s signals to know when they are full. Watching TV while eating can make a child unaware of feeling full.

Watching TV while eating may cause children to not realize when they are full
- Consuming Too Many Sugary Drinks or Fruit Juices: Save soda and sugary drinks for special occasions. Fruit
- juices, even those labeled 100% natural, contain a lot of sugar and calories. Limit fruit juice intake to 4-6 ounces per day.
- Excessive Screen Time: Limit screen time to 1-2 hours a day, and encourage outdoor play or other physical activities. Children should engage in moderate to vigorous physical activity for at least 1 hour per day.
- Lack of Family Meals: Children who eat with their families are less likely to consume high-calorie snacks or soda. Share meals as a family whenever possible.
Consequences of Childhood Obesity
Physical Consequences
- Metabolic Syndrome: Defined by a combination of factors, including abdominal obesity, high blood pressure, high blood sugar, and abnormal lipid levels.
- Type 2 Diabetes: Childhood obesity increases the risk of developing type 2 diabetes.
- Cardiovascular Diseases: High blood pressure and high cholesterol levels are more common in obese children, increasing the risk of heart disease later in life.
- Orthopedic Problems: Excess weight can stress the bones and joints, leading to issues such as fractures, knee pain, and back pain.
- Sleep Apnea: Obese children are at a higher risk of sleep apnea, which can lead to daytime fatigue and other health problems.
- Liver Disease: Nonalcoholic fatty liver disease (NAFLD) is more prevalent in obese children.
Psychological Consequences
- Low Self-Esteem: Obese children may experience low self-esteem and face discrimination from peers.
- Depression and Anxiety: There is a higher prevalence of depression and anxiety in obese children.
- Social Isolation: Due to societal biases, obese children may face social isolation and bullying.
- Eating Disorders: Some obese children may develop unhealthy eating patterns and, in extreme cases, eating disorders.
Long-term Consequences
– Childhood obesity often persists into adulthood, increasing the risk of obesity-related health issues.
– Long-term consequences include a higher risk of heart disease, stroke, type 2 diabetes, and certain types of cancer.
Prevention and Intervention Strategies
Family-Based Approaches
- Promote Healthy Eating Habits: Encourage a balanced diet with plenty of fruits, vegetables, whole grains, and lean proteins. Limit the intake of sugary snacks and beverages.
- Regular Physical Activity: Encourage at least 60 minutes of moderate to vigorous physical activity per day.
- Family Meals: Aim for regular family meals, as they provide an opportunity to model healthy eating behaviors.
- Limit Screen Time: Set limits on screen time to encourage physical activity and prevent mindless snacking.
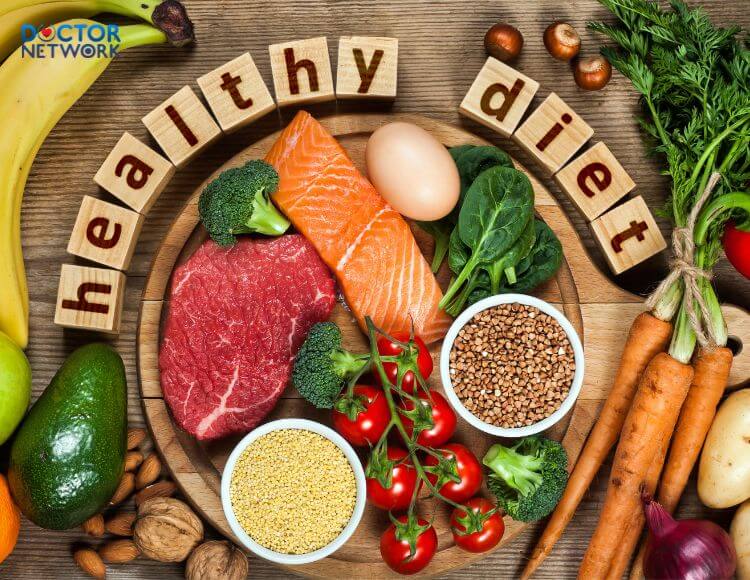
Diet plays a crucial role in combating obesity
School-Based Approaches
- Physical Education Programs: Implement and support physical education programs in schools.
- Healthy School Lunches: Ensure that school cafeterias offer nutritious meals and snacks.
- Education on Healthy Habits: Provide education on nutrition and the importance of a healthy lifestyle.
Community and Policy Approaches
- Community Programs: Support community-based programs that promote healthy living.
- Policy Changes: Advocate for policies that create environments conducive to healthy eating and physical activity.
- Media Literacy: Promote media literacy to help children critically evaluate food advertisements and make informed choices.
Medical Interventions
- Multidisciplinary Approach: In severe cases, a multidisciplinary team involving healthcare professionals, nutritionists, and psychologists can provide comprehensive care.
- Behavioral Interventions: Behavioral therapy can help children and their families adopt healthier habits.
- Pharmacological Treatment: In specific cases, pharmacological interventions may be considered under medical supervision.
- Surgical Interventions: In extreme cases of obesity, surgical options like bariatric surgery may be considered for adolescents.
Childhood obesity is a complex and multifaceted issue that requires a comprehensive approach from families, schools, communities, and healthcare systems. Early intervention and prevention strategies are crucial in addressing this public health concern and mitigating the long-term consequences associated with obesity. By promoting healthy lifestyles, fostering supportive environments, and implementing evidence-based interventions, we can work towards ensuring a healthier and brighter future for our children.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.