“Can You Have TPO Antibodies From Adrenal Fatigue?” Learn if adrenal fatigue plays a role in raising TPO antibodies. Understand the connection between stress, hormones, and your thyroid.
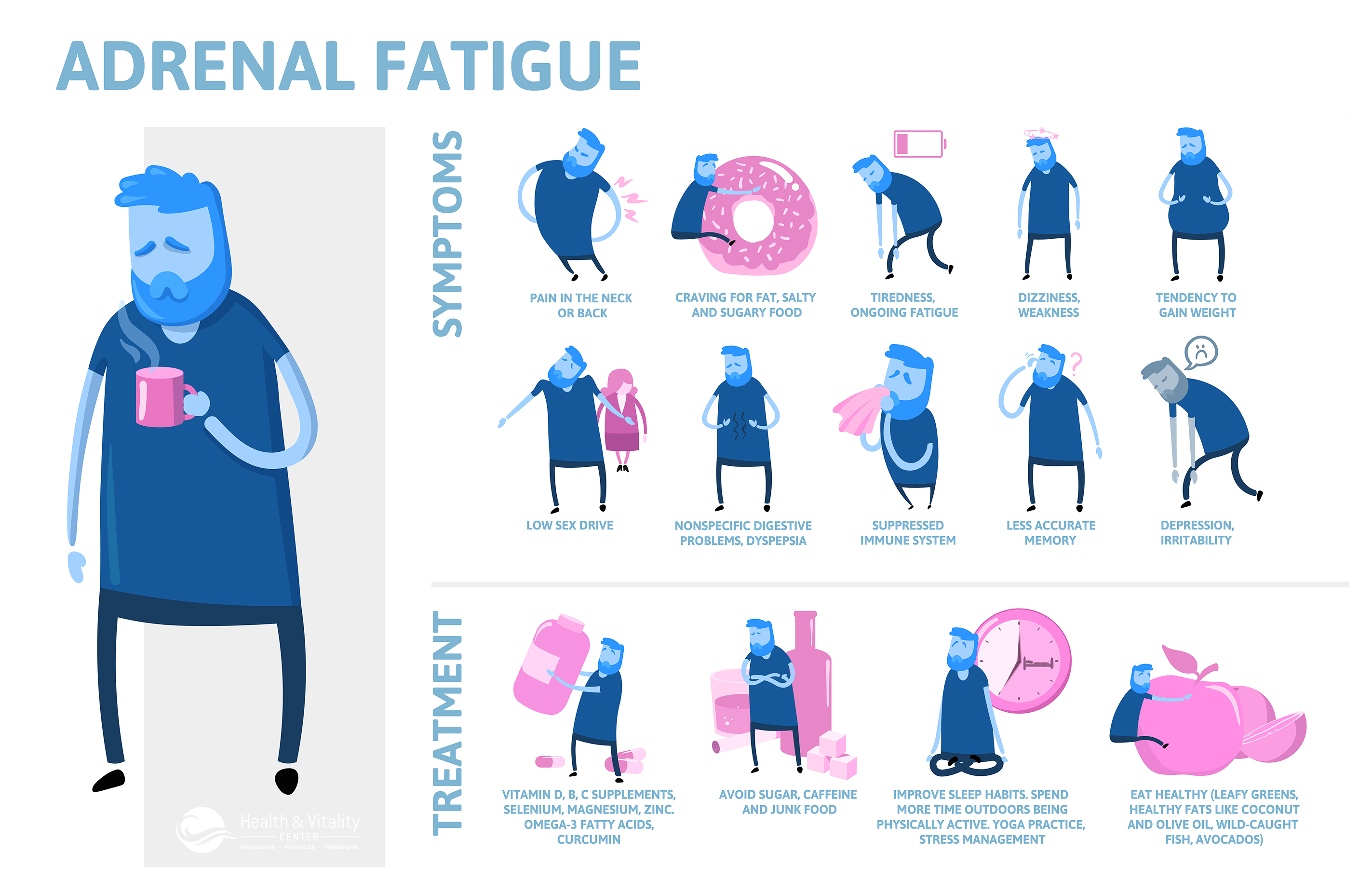
Adrenal Fatigue Stages
Millions of people worldwide struggle with unexplained fatigue, brain fog, and metabolic dysfunction, often wondering if their exhausted adrenal glands could trigger autoimmune thyroid conditions like Hashimoto’s thyroiditis. While direct causation between adrenal fatigue and TPO (thyroid peroxidase) antibodies remains scientifically unproven, mounting evidence suggests chronic stress significantly influences immune system regulation and thyroid function through complex neuroendocrine pathways. This comprehensive analysis explores the intricate connections between hypothalamic-pituitary-adrenal (HPA) axis dysfunction, systemic inflammation, and autoimmune thyroid disease development.
We’ll examine the biological mechanisms behind TPO antibody formation, deconstruct the controversial concept of adrenal fatigue, and investigate how chronic stress impacts immune tolerance and thyroid hormone metabolism. Additionally, we’ll explore evidence-based management strategies that address root causes of fatigue while supporting optimal thyroid health, providing clarity for patients navigating these interconnected health challenges.
Understanding TPO Antibodies and Autoimmune Thyroid Disease
TPO antibodies represent the immune system’s misguided attack against thyroid peroxidase, a crucial enzyme responsible for thyroid hormone synthesis within follicular cells. The thyroid gland, positioned strategically in the anterior neck, orchestrates metabolic processes throughout the body by producing thyroxine (T4) and triiodothyronine (T3), hormones that regulate cellular energy production, thermogenesis, and cardiovascular function.
The Thyroid Gland’s Essential Functions
The butterfly-shaped thyroid gland serves as the body’s metabolic control center, synthesizing hormones that influence virtually every organ system. Thyroid-stimulating hormone (TSH) from the anterior pituitary triggers the release of T4, which undergoes peripheral conversion to the more potent T3 through deiodinase enzymes. This intricate feedback loop maintains homeostatic balance between energy expenditure and conservation.
Thyroid peroxidase facilitates the oxidation of iodide and subsequent iodination of tyrosine residues within thyroglobulin, essential steps in hormone biosynthesis. When TPO antibodies bind to this enzyme, they disrupt normal thyroid function and indicate underlying autoimmune processes.
Mechanisms of TPO Antibody Formation
TPO antibodies develop when the adaptive immune system loses tolerance to thyroid antigens, recognizing thyroid peroxidase as foreign rather than self. This autoimmune response involves complex interactions between genetic predisposition, environmental triggers, and immune system dysregulation.
The presence of TPO antibodies serves as a biomarker for Hashimoto’s thyroiditis, the most prevalent cause of hypothyroidism in iodine-sufficient regions. These antibodies can be detected years before clinical hypothyroidism manifests, suggesting a gradual autoimmune destruction of thyroid tissue.
| TPO Antibody Levels | Clinical Significance | Associated Conditions |
|---|---|---|
| <35 IU/mL | Normal range | Euthyroid state |
| 35-100 IU/mL | Mildly elevated | Subclinical thyroiditis |
| 100-1000 IU/mL | Moderately elevated | Hashimoto’s thyroiditis |
| >1000 IU/mL | Severely elevated | Advanced autoimmune destruction |
Causes of Autoimmune Thyroid Disease
Autoimmune thyroid conditions arise from multifactorial influences including genetic susceptibility, environmental exposures, and immune system perturbations. Human leukocyte antigen (HLA) polymorphisms, particularly HLA-DR3 and HLA-DR5, increase susceptibility to thyroid autoimmunity.
Environmental triggers encompass:
- Infectious agents (Epstein-Barr virus, Helicobacter pylori)
- Excessive iodine intake
- Selenium deficiency
- Chronic psychological stress
- Endocrine disruptors
- Smoking cessation (paradoxically)
Deconstructing “Adrenal Fatigue” and the Stress Response

Adrenal Fatigue
Adrenal fatigue represents a controversial concept proposing that chronic stress exhausts the adrenal glands’ capacity to produce adequate cortisol and other stress hormones. The hypothalamic-pituitary-adrenal (HPA) axis orchestrates the body’s stress response through intricate neuroendocrine signaling between the hypothalamus, anterior pituitary, and adrenal cortex.
The HPA Axis: Central Command of Stress Response
The HPA axis functions as the body’s primary stress-response system, coordinating physiological adaptations to perceived threats or challenges. Corticotropin-releasing hormone (CRH) from the hypothalamus stimulates adrenocorticotropic hormone (ACTH) release from the pituitary, which subsequently triggers cortisol production in the adrenal cortex.
Cortisol, often called the “stress hormone,” exerts wide-ranging effects including glucose mobilization, anti-inflammatory actions, and immune system modulation. Under normal circumstances, cortisol follows a circadian rhythm with peak levels in the early morning and nadir concentrations at night.
The adrenal glands also produce aldosterone for electrolyte balance, catecholamines (epinephrine and norepinephrine) for acute stress responses, and sex hormone precursors including dehydroepiandrosterone (DHEA).
The “Adrenal Fatigue” Hypothesis
Proponents of adrenal fatigue theory propose a progressive decline in adrenal function through distinct stages:
- Alarm Stage: Initial stress response with elevated cortisol
- Resistance Stage: Sustained high cortisol with gradual depletion
- Exhaustion Stage: Severely diminished cortisol production
Reported symptoms include chronic fatigue, difficulty awakening, salt cravings, reduced stress tolerance, brain fog, and immune dysfunction. However, these nonspecific symptoms overlap considerably with numerous medical conditions.
Medical Consensus on “Adrenal Fatigue”
Mainstream endocrinology organizations, including the Endocrine Society and American Association of Clinical Endocrinologists, do not recognize adrenal fatigue as a legitimate medical diagnosis. Rigorous scientific studies have failed to demonstrate the proposed mechanism of adrenal exhaustion from chronic stress.
True adrenal insufficiency conditions include:
- Primary adrenal insufficiency (Addison’s disease): Autoimmune destruction of adrenal cortex
- Secondary adrenal insufficiency: Pituitary ACTH deficiency
- Tertiary adrenal insufficiency: Hypothalamic CRH deficiency
These conditions require specific diagnostic criteria and hormone replacement therapy, contrasting sharply with the vague symptomatology attributed to adrenal fatigue.
Symptoms commonly attributed to adrenal fatigue frequently result from other medical conditions including depression, sleep disorders, thyroid dysfunction, chronic fatigue syndrome, fibromyalgia, or lifestyle factors such as poor sleep hygiene and nutritional deficiencies.
Exploring the Proposed Intersections: Stress, Adrenals, and Autoimmunity
While direct causation between adrenal fatigue and TPO antibodies lacks scientific validation, chronic stress undeniably influences immune function and thyroid physiology through multiple pathways. Understanding these complex interactions provides insights into how psychological stress might contribute to autoimmune thyroid disease development or progression.
The Indirect Link: Stress and Thyroid Dysfunction
Chronic stress impacts thyroid function through several mechanisms beyond direct antibody formation. HPA axis dysregulation can significantly alter thyroid hormone metabolism, conversion, and peripheral sensitivity without necessarily triggering autoimmune responses.
HPA Axis Dysregulation Effects:
- Elevated cortisol inhibits TSH secretion from the pituitary
- Reduced peripheral T4 to T3 conversion through deiodinase enzyme suppression
- Increased reverse T3 (rT3) production, creating metabolically inactive hormone
- Altered thyroid hormone-binding protein concentrations
- Decreased cellular thyroid hormone sensitivity
These mechanisms can produce subclinical hypothyroid symptoms even with normal standard thyroid function tests, explaining why some individuals experience thyroid-like symptoms despite unremarkable TSH and T4 levels.
Inflammation and Immune Dysregulation: Chronic stress promotes systemic inflammation through multiple pathways, creating an environment conducive to autoimmune disease development. Persistent elevations in pro-inflammatory cytokines including interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP) can disrupt immune tolerance and potentially trigger autoimmune responses.
Stress-induced inflammation also impairs regulatory T-cell (Treg) function, which normally maintains immune tolerance and prevents autoimmune reactions. When Treg cells become dysfunctional, the risk of autoimmune disease development increases significantly.
Gut Health and the Microbiome Connection
The bidirectional relationship between chronic stress, gastrointestinal health, and immune regulation represents another potential pathway linking stress to autoimmune thyroid disease. Chronic stress alters gut microbiome composition, increases intestinal permeability (“leaky gut”), and disrupts the gut-associated lymphoid tissue (GALT).
| Stress Effects on Gut Health | Impact on Immune Function | Thyroid Implications |
|---|---|---|
| Reduced beneficial bacteria | Increased inflammation | Enhanced autoimmune risk |
| Increased intestinal permeability | Molecular mimicry | Cross-reactive antibodies |
| Altered short-chain fatty acids | Regulatory T-cell dysfunction | Loss of immune tolerance |
| Dysbiosis-related endotoxemia | Systemic immune activation | Thyroid tissue inflammation |
The Autoimmune Angle: Can Stress Trigger Autoimmunity?
Epidemiological studies consistently demonstrate associations between psychological stress and autoimmune disease onset or exacerbation. Major life stressors, including bereavement, divorce, job loss, or traumatic events, often precede autoimmune disease diagnosis by months or years.
Stress-Related Immune System Changes:
- Altered T-helper cell balance (Th1/Th2/Th17/Treg)
- Increased molecular mimicry susceptibility
- Enhanced antigen presentation
- Reduced immune surveillance
- Disrupted circadian immune rhythms
Research suggests that chronic stress may serve as an environmental trigger for Hashimoto’s thyroiditis in genetically susceptible individuals. However, stress alone is insufficient to cause autoimmune thyroid disease; genetic predisposition and additional environmental factors typically contribute to disease development.
Nutrient Deficiencies and Lifestyle Factors

Nutrient Deficiencies
Chronic stress and the lifestyle patterns associated with “adrenal fatigue” can deplete essential nutrients crucial for optimal thyroid function and immune regulation. These deficiencies may indirectly contribute to autoimmune thyroid disease risk or progression.
Critical Nutrients for Thyroid Health:
- Selenium: Essential for deiodinase enzymes and antioxidant protection
- Deficiency increases TPO antibody levels
- Supplementation may reduce antibody titers in Hashimoto’s patients
- Vitamin D: Crucial for immune regulation and tolerance
- Deficiency associated with increased autoimmune disease risk
- Modulates Treg cell function
- Magnesium: Required for enzyme function and stress resilience
- Depletion common in chronic stress
- Essential for T4 to T3 conversion
- Zinc: Important for thyroid hormone synthesis and immune function
- Deficiency impairs cellular immunity
- Required for optimal deiodinase activity
- B-Complex vitamins: Essential for adrenal function and energy metabolism
- B6, B12, and folate particularly important
- Depletion common in chronic stress states
The Functional Medicine Perspective
Functional medicine practitioners emphasize identifying and addressing root causes of symptoms rather than simply managing isolated conditions. This approach recognizes the interconnected nature of physiological systems and focuses on optimizing overall health through comprehensive lifestyle interventions.
Functional Medicine Approach to Thyroid-Adrenal Health:
- Comprehensive hormone and nutrient testing
- Stress management and HPA axis support
- Gut health optimization
- Anti-inflammatory dietary interventions
- Targeted nutritional supplementation
- Sleep hygiene improvement
- Regular moderate exercise
- Toxin exposure reduction
This holistic perspective acknowledges that supporting overall endocrine system balance may benefit thyroid health regardless of specific diagnostic labels or the validity of “adrenal fatigue” as a medical condition.
Diagnosis and Management Approaches
Proper evaluation of suspected thyroid autoimmunity and stress-related symptoms requires comprehensive assessment combining clinical evaluation, laboratory testing, and consideration of lifestyle factors. Accurate diagnosis forms the foundation for effective treatment strategies.
Diagnosing TPO Antibodies and Thyroid Conditions
Thyroid function assessment should include multiple parameters beyond the standard TSH screening typically performed in primary care settings. Comprehensive thyroid evaluation provides more complete information about thyroid health and autoimmune activity.
Essential Thyroid Tests:
- Thyroid-stimulating hormone (TSH)
- Free thyroxine (Free T4)
- Free triiodothyronine (Free T3)
- Reverse T3 (rT3)
- Thyroid peroxidase antibodies (TPO Ab)
- Thyroglobulin antibodies (TgAb)
- TSH receptor antibodies (TRAb) when indicated
Optimal reference ranges may differ from laboratory “normal” ranges, with functional medicine practitioners often targeting TSH levels between 1.0-2.5 mIU/L for optimal well-being. However, individual variation exists, and treatment decisions should consider symptoms alongside laboratory values.
Interpreting TPO Antibody Results: TPO antibody elevation indicates autoimmune thyroid involvement but doesn’t necessarily correlate with symptom severity or thyroid function impairment. Some individuals maintain normal thyroid function despite high antibody levels, while others develop clinical hypothyroidism with modest antibody elevations.
Addressing “Adrenal Fatigue” Symptoms
Rather than focusing on the controversial diagnosis of adrenal fatigue, evidence-based approaches target the underlying factors contributing to fatigue, stress intolerance, and related symptoms. These interventions support optimal HPA axis function and overall resilience.
Stress Management Strategies:
- Mindfulness and Meditation: Regular practice reduces cortisol levels and improves stress resilience
- Cognitive Behavioral Therapy: Addresses stress-related thought patterns and coping strategies
- Deep Breathing Exercises: Activates parasympathetic nervous system
- Progressive Muscle Relaxation: Reduces physical tension and stress hormones
- Yoga and Tai Chi: Combine movement, breathing, and mindfulness
Sleep Optimization: Quality sleep is essential for HPA axis recovery and immune system regulation. Sleep disturbances can perpetuate both stress-related symptoms and autoimmune activity.
- Maintain consistent sleep-wake schedules
- Create optimal sleep environment (cool, dark, quiet)
- Limit screen exposure before bedtime
- Address sleep disorders (sleep apnea, restless leg syndrome)
- Consider natural sleep aids when appropriate
Nutritional Support: Targeted nutrition addresses nutrient deficiencies common in chronic stress while supporting thyroid and immune function.
| Nutrient | Daily Dose Range | Primary Benefits | Food Sources |
|---|---|---|---|
| Selenium | 200-400 mcg | Reduces TPO antibodies | Brazil nuts, seafood |
| Vitamin D3 | 2000-5000 IU | Immune regulation | Sunlight, fatty fish |
| Magnesium | 300-600 mg | Stress resilience | Leafy greens, nuts |
| Omega-3 fatty acids | 1000-3000 mg EPA/DHA | Anti-inflammatory | Fish oil, algae |
| Adaptogenic herbs | Varies by herb | HPA axis support | Ashwagandha, rhodiola |
Exercise Considerations: Appropriate exercise supports stress resilience and thyroid function, but excessive high-intensity training can worsen HPA axis dysfunction and increase cortisol production.
Recommended exercise approaches:
- Moderate-intensity aerobic exercise (walking, swimming, cycling)
- Resistance training with adequate recovery
- Yoga and gentle stretching
- Avoid excessive endurance training during recovery phases
Conventional vs. Integrative Treatment
Optimal patient care often combines evidence-based conventional treatments with integrative approaches addressing lifestyle and root cause factors. This collaborative approach maximizes therapeutic outcomes while ensuring patient safety.
Conventional Thyroid Treatment:
- Thyroid hormone replacement therapy (levothyroxine, liothyronine)
- Regular monitoring of thyroid function tests
- Adjustment of medication dosing based on symptoms and laboratory values
- Treatment of associated conditions (depression, cardiovascular disease)
Integrative Approaches:
- Comprehensive nutrient assessment and supplementation
- Stress management program implementation
- Gut health optimization through probiotics and dietary changes
- Environmental toxin reduction
- Sleep hygiene improvement
- Mind-body therapies
The integration of conventional and complementary approaches provides the most comprehensive treatment strategy, addressing both immediate symptom relief and long-term prevention of disease progression.
Navigating the Complexities – Can You Have TPO Antibodies From Adrenal Fatigue
The relationship between chronic stress, adrenal dysfunction, and TPO antibody development represents a complex interplay of neuroendocrine, immune, and environmental factors rather than a simple cause-and-effect relationship. While direct scientific evidence linking “adrenal fatigue” to TPO antibody formation remains absent, chronic stress undeniably influences immune system regulation and thyroid physiology through multiple indirect mechanisms.
The HPA axis dysfunction associated with chronic stress can impair thyroid hormone metabolism, promote systemic inflammation, and potentially contribute to the environmental triggers that precipitate autoimmune thyroid disease in genetically susceptible individuals. However, these effects represent indirect influences rather than direct causation of TPO antibody production.
Key Clinical Takeaways:
- Focus on evidence-based assessment of both thyroid function and stress-related symptoms
- Address root causes including chronic stress, nutrient deficiencies, and lifestyle factors
- Implement comprehensive treatment approaches combining conventional and integrative therapies
- Recognize that symptom improvement may occur through multiple pathways regardless of specific diagnostic labels
- Maintain realistic expectations about treatment timelines and outcomes
The most effective approach emphasizes holistic health optimization through stress reduction, nutritional support, sleep improvement, and appropriate medical treatment when indicated. This comprehensive strategy supports overall well-being and may help prevent or manage autoimmune thyroid conditions while addressing the symptoms commonly attributed to adrenal fatigue.
Rather than seeking simple answers to complex health challenges, patients and practitioners benefit from embracing the multifactorial nature of chronic illness and implementing evidence-based interventions that support optimal physiological function across multiple systems. Consulting with qualified healthcare professionals remains essential for accurate diagnosis, appropriate treatment, and ongoing monitoring of both thyroid health and stress-related symptoms.
Top 5 Frequently Asked Questions About TPO Antibodies and Adrenal Fatigue
1. Can adrenal fatigue cause TPO antibodies?
There is no scientific evidence that adrenal fatigue directly causes the production of TPO (thyroid peroxidase) antibodies. TPO antibodies are most commonly associated with autoimmune thyroid diseases, such as Hashimoto’s thyroiditis and Graves’ disease, rather than adrenal dysfunction. While both adrenal and thyroid issues can cause fatigue, the mechanisms and origins are different.
2. Is there a link between adrenal fatigue and autoimmune thyroid disease?
Adrenal fatigue is a controversial and unproven diagnosis in mainstream medicine, but chronic stress can influence immune function. However, studies have not established a direct link between adrenal fatigue and the development of autoimmune thyroid diseases or TPO antibodies. Fatigue is common in autoimmune thyroid diseases, but it does not mean adrenal fatigue is the cause.
3. Can you have high TPO antibodies without thyroid disease?
Yes, some people have elevated TPO antibodies without showing signs or symptoms of thyroid disease. The presence of TPO antibodies increases the risk of developing thyroid disorders in the future, but not everyone with these antibodies will develop hypothyroidism or other thyroid issues.
4. What are the main causes of TPO antibodies?
TPO antibodies are caused by an autoimmune response in which the immune system mistakenly attacks the thyroid gland. The most common causes are autoimmune thyroid diseases, such as Hashimoto’s thyroiditis and Graves’ disease. Factors like genetics, environmental triggers, and possibly stress may contribute, but adrenal fatigue is not a recognized cause.
5. Can fatigue from thyroid disease be mistaken for adrenal fatigue?
Yes, fatigue is a common symptom in both thyroid disorders and what is sometimes called adrenal fatigue. However, in autoimmune thyroid disease, fatigue is related to changes in thyroid hormone levels and immune activity, not to adrenal gland dysfunction. Proper diagnosis requires laboratory testing for thyroid function and antibodies, not just symptoms.
References
Cadegiani, F. A., & Kater, C. E. (2016). Adrenal fatigue does not exist: a systematic review. BMC Endocrine Disorders.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4997656/Mizokami, T., Wu Li, A., El-Kaissi, S., & Wall, J. R. (2004). Stress and thyroid autoimmunity. Thyroid.
https://pubmed.ncbi.nlm.nih.gov/15650357/Tsatsoulis, A., & Fountoulakis, S. (2006). The protective role of exercise on stress-induced dysregulation of the thyroid axis. Annals of the New York Academy of Sciences.
https://nyaspubs.onlinelibrary.wiley.com/doi/abs/10.1196/annals.1367.016Kahaly, G. J. (2009). Polyglandular autoimmune syndromes. European Journal of Endocrinology.
https://eje.bioscientifica.com/view/journals/eje/161/1/11.xml
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.