Corticosteroids, powerful anti-inflammatory medications, are widely prescribed for various skin conditions. However, their use can lead to significant adverse effects on dermal health. This article delves into “harmful effects of corticosteroids on the skin“, exploring both topical and systemic side effects, long-term consequences, and strategies to minimize harm. We’ll examine the science behind these drugs, their impact on skin structure and function, and alternative treatment options for those concerned about corticosteroid-related complications.
Understanding Corticosteroids and Their Uses
What are Corticosteroids?
Corticosteroids are synthetic drugs that mimic the effects of hormones naturally produced by the adrenal glands. These potent medications are used to treat a wide range of inflammatory and autoimmune conditions affecting the skin and other organs.

Corticosteroids are synthetic drugs that mimic the effects of hormones naturally produced by the adrenal glands
Types of Corticosteroids and their Uses
Corticosteroids come in various forms, including:
- Topical preparations (creams, ointments, lotions)
- Oral tablets
- Injectable solutions
- Inhalers
For dermatological conditions, topical corticosteroids are most commonly prescribed. They’re used to treat:
- Eczema
- Psoriasis
- Dermatitis
- Allergic reactions
- Insect bites
How Corticosteroids Work on the Skin
Corticosteroids exert their effects by:
- Reducing inflammation
- Suppressing the immune response
- Constricting blood vessels
- Inhibiting cell proliferation
While these actions can provide relief from skin symptoms, they also contribute to the potential side effects.
Common Side Effects of Topical Corticosteroids
Skin Thinning and Atrophy
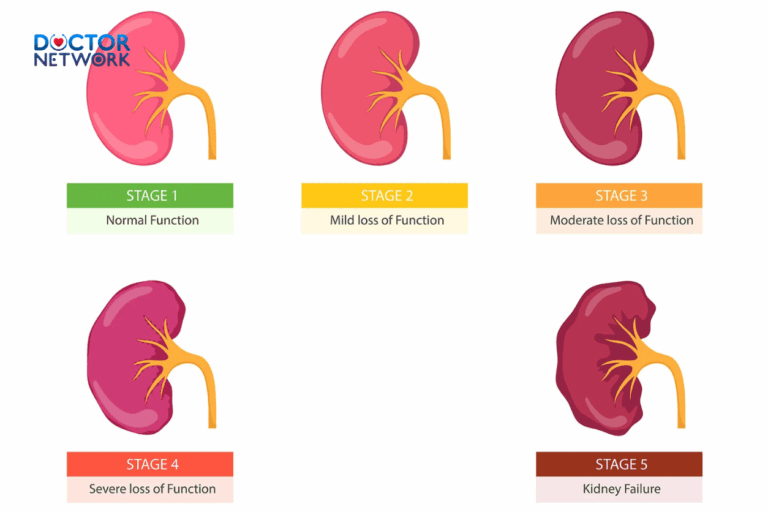
The most well-known adverse effect of topical corticosteroids is skin atrophy. Prolonged use can lead to:
- Decreased collagen synthesis
- Reduced elastin production
- Thinning of the epidermis and dermis
The most well-known adverse effect of topical corticosteroids is skin atrophy
These changes make the skin more fragile and susceptible to injury.
Striae (Stretch Marks)
Corticosteroids can cause the formation of striae, or stretch marks, particularly when used on areas with thin skin such as the face, armpits, or groin.
Acneiform Eruptions
Some patients may develop acne-like lesions, especially when using potent corticosteroids on the face.
Rosacea-like Changes
Long-term use of topical corticosteroids on the face can lead to a condition known as steroid rosacea, characterized by persistent redness and inflammation.
Increased Sensitivity and Irritation
Paradoxically, corticosteroids can sometimes increase skin sensitivity, leading to:
- Burning sensations
- Itching
- Redness
Skin Discoloration (Hyperpigmentation or Hypopigmentation)
Corticosteroids can alter melanin production, resulting in:
- Darkening of the skin (hyperpigmentation)
- Lightening of the skin (hypopigmentation)
Delayed Wound Healing
By suppressing cell proliferation and collagen synthesis, corticosteroids can significantly impair the skin’s ability to heal wounds.
Systemic Side Effects of Corticosteroids
While less common with topical use, prolonged or high-dose corticosteroid therapy can lead to systemic effects:
Cushing’s Syndrome
Excessive corticosteroid exposure can result in Cushing’s syndrome, characterized by:
- Weight gain
- Moon face
- Buffalo hump
- Striae
Osteoporosis
Corticosteroids interfere with calcium metabolism and bone formation, increasing the risk of osteoporosis.

Corticosteroids interfere with calcium metabolism and bone formation, increasing the risk of osteoporosis
Immunosuppression
By suppressing the immune system, corticosteroids can increase susceptibility to infections.
High Blood Pressure
Corticosteroids can cause fluid retention and increased blood pressure.
High Blood Sugar
These medications can interfere with glucose metabolism, potentially leading to or exacerbating diabetes.
Risks of Long-Term Corticosteroid Use
Dependence and Withdrawal Symptoms
Table: Corticosteroid Withdrawal Symptoms
| Symptom | Description | Management |
|---|---|---|
| Skin flare | Worsening of original condition | Gradual tapering of medication |
| Redness | Increased blood flow to skin | Cool compresses, emollients |
| Burning sensation | Heightened skin sensitivity | Avoid irritants, use gentle skincare |
| Peeling | Excessive skin shedding | Moisturize frequently |
| Itching | Intense urge to scratch | Antihistamines, oatmeal baths |
Increased Risk of Infections
Long-term corticosteroid use can compromise the skin’s barrier function, making it more susceptible to bacterial, fungal, and viral infections.
Cumulative Skin Damage
The harmful effects of corticosteroids on skin structure can accumulate over time, leading to:
- Permanent thinning
- Increased fragility
- Impaired healing capacity
Minimizing the Risks of Corticosteroid Treatment
To reduce the potential for adverse effects, consider the following strategies:
- Use the lowest effective dose
- Limit treatment duration
- Implement intermittent treatment cycles
- Avoid use on sensitive areas (face, genitals, skin folds)
- Maintain proper skin hygiene and hydration
Using the Lowest Effective Dose
Work with your healthcare provider to determine the minimum corticosteroid strength needed to manage your condition effectively.
Shortest Possible Duration of Treatment
Limit corticosteroid use to the shortest time necessary to achieve symptom control.
Intermittent Treatment Cycles
Consider using corticosteroids in cycles, with periods of non-use to allow skin recovery.
Avoiding Use on Sensitive Areas
Be cautious when applying corticosteroids to thin-skinned areas like the face, as these regions are more prone to side effects.
Keeping the Skin Clean and Moisturized
Proper skincare can help maintain skin health and potentially reduce the need for corticosteroid treatment.
Alternative Treatments for Skin Conditions
For those concerned about corticosteroid side effects, several alternatives exist:
Topical Antihistamines
These can help relieve itching and inflammation without the risks associated with corticosteroids.
Topical Immunomodulators
Medications like tacrolimus and pimecrolimus can manage certain skin conditions without causing skin atrophy.
Phototherapy
Controlled exposure to specific wavelengths of light can help treat conditions like psoriasis and eczema.
Natural Remedies
Some patients find relief with natural options such as:
- Aloe vera gel
- Tea tree oil
- Coconut oil
- Oatmeal baths
When to Consult a Doctor
Seek medical attention if you experience:
- Signs of severe side effects (e.g., excessive skin thinning, widespread discoloration)
- Failure of corticosteroid treatment to improve your condition
- Concerns about your current treatment regimen
Signs of Severe Side Effects
Watch for:
- Excessive bruising
- Visible blood vessels (telangiectasia)
- Persistent redness or swelling
Failure of Corticosteroid Treatment
If your skin condition doesn’t improve or worsens despite corticosteroid use, consult your healthcare provider.
Concerns About Treatment
Don’t hesitate to discuss any worries or questions about your corticosteroid treatment with a medical professional.
FAQs about “harmful effects of corticosteroids on the skin”
How long can I safely use topical corticosteroids on my skin?
The safe duration of topical corticosteroid use depends on several factors, including the strength of the medication, the area of application, and the specific skin condition being treated. Generally, potent topical corticosteroids should not be used for more than 2-3 weeks continuously without medical supervision. For milder formulations, longer use may be appropriate under a doctor’s guidance. Prolonged use of topical corticosteroids can lead to skin atrophy, striae formation, and other adverse effects. It’s crucial to follow your dermatologist’s instructions and use the lowest effective strength for the shortest necessary duration.
Can corticosteroid creams cause permanent skin damage?
Yes, long-term or improper use of corticosteroid creams can potentially cause permanent skin damage. Chronic application of topical corticosteroids, especially high-potency formulations, can lead to irreversible skin atrophy, where the skin becomes permanently thin, fragile, and prone to bruising and tearing. Other potential long-lasting effects include striae (stretch marks), telangiectasia (visible blood vessels), and hypopigmentation (skin lightening). These changes may persist even after discontinuing the medication. To minimize the risk of permanent damage, it’s essential to use corticosteroids as directed by a healthcare professional and to have regular follow-ups to assess skin health.
What are the signs of topical steroid withdrawal, and how can I manage them?
Topical steroid withdrawal (TSW), also known as Red Skin Syndrome, can occur when abruptly stopping long-term use of topical corticosteroids. Signs and symptoms may include:
- Intense redness and burning of the skin
- Severe itching
- Skin peeling or flaking
- Oozing or weeping of the skin
- Swelling and edema
- Increased skin sensitivity
- Rebound flare of the original skin condition
Managing TSW can be challenging and may require professional medical guidance. Some strategies include:
- Gradually tapering off the corticosteroid use under medical supervision
- Using emollients and moisturizers to soothe the skin
- Applying cool compresses to relieve burning sensations
- Taking oral antihistamines to reduce itching
- Considering alternative treatments for the underlying skin condition
- Practicing stress-reduction techniques, as stress can exacerbate symptoms
It’s crucial to consult with a dermatologist if you suspect you’re experiencing topical steroid withdrawal.
Are there any natural alternatives to corticosteroids for treating skin inflammation?
While corticosteroids are often highly effective for treating skin inflammation, some natural alternatives may help manage mild to moderate skin conditions:
- Aloe vera: Known for its anti-inflammatory properties, aloe vera gel can soothe irritated skin and promote healing.
- Calendula: This herb has anti-inflammatory and wound-healing properties, often used in creams or ointments for skin irritation.
- Chamomile: Applied topically, chamomile can help reduce inflammation and soothe the skin.
- Oatmeal baths: Colloidal oatmeal can help relieve itching and inflammation associated with various skin conditions.
- Omega-3 fatty acids: Consuming foods rich in omega-3s or taking supplements may help reduce skin inflammation from within.
It’s important to note that these natural alternatives may not be as potent as corticosteroids and may not be suitable for all skin conditions. Always consult with a healthcare provider before switching treatments or incorporating new remedies into your skincare routine.
How do corticosteroids affect wound healing, and what precautions should I take?
Corticosteroids can significantly impact wound healing through several mechanisms:
- Inhibition of collagen synthesis: Corticosteroids reduce the production of collagen, a crucial component in wound healing.
- Suppression of inflammatory response: While this can reduce pain and swelling, it may also slow the initial stages of wound healing.
- Decreased angiogenesis: Corticosteroids can inhibit the formation of new blood vessels, which are essential for tissue repair.
- Increased risk of infection: By suppressing the immune response, corticosteroids may make wounds more susceptible to bacterial, fungal, or viral infections.
Precautions to take when using corticosteroids on or near wounds:
- Avoid applying topical corticosteroids directly to open wounds unless specifically instructed by a healthcare provider.
- If you’re taking systemic corticosteroids and need to undergo surgery, inform your healthcare team, as dosage adjustments may be necessary.
- Monitor wounds closely for signs of infection, such as increased redness, warmth, swelling, or purulent discharge.
- Maintain good wound hygiene and follow proper wound care protocols.
- Consider using wound dressings that promote moist wound healing, as corticosteroids can cause skin dryness.
- If you notice delayed wound healing, consult your healthcare provider for alternative management strategies.
Remember, the impact of corticosteroids on wound healing can vary depending on the dose, duration of use, and individual factors. Always follow medical advice when managing wounds while using corticosteroid treatments.
Scientific researches on “harmful effects of corticosteroids on the skin”
- “Long-term effects of topical corticosteroids on skin structure and function” – This study was conducted by Castela E. et al., published in the Journal of Clinical and Experimental Dermatology.
- “Topical corticosteroid withdrawal syndrome: A comprehensive review” – Study by Hajar T. et al., published in the Journal of the American Academy of Dermatology.
- “Cutaneous side effects of topical corticosteroids: Prevention and treatment” – Study by Coondoo A. et al., published in the Indian Journal of Dermatology.
- “Corticosteroid-induced skin atrophy: Mechanisms and prevention” – Study by Schoepe S. et al., published in the Journal of Experimental Dermatology.
- “Effects of topical corticosteroids on the skin barrier function” – Study by Jensen JM. et al., published in the Journal of the European Academy of Dermatology and Venereology.
Conclusion
Summary of Key Points
Corticosteroids are potent medications that can effectively manage various skin conditions. However, their use comes with potential risks, including skin thinning, increased sensitivity, and systemic effects. By understanding these risks and implementing strategies to minimize them, patients can make informed decisions about their treatment options.
Promoting Skin Health and Safety
While corticosteroids remain an important tool in dermatology, it’s crucial to use them judiciously and under medical supervision. By exploring alternative treatments, practicing good skincare, and maintaining open communication with healthcare providers, patients can achieve optimal skin health while minimizing the risks associated with corticosteroid use.
Disclaimer
This information is intended to increase general knowledge and does not substitute for professional medical advice. Always consult a qualified healthcare provider before starting, stopping, or modifying any treatment regimen.
References:
How Safe Are Steroid Creams? – Arthritis Foundationarthritis·1
Topical Corticosteroids: Choice and Application – AAFPaafp·2
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.