The increasing prevalence of gastroesophageal reflux disease (GERD) and obesity has raised significant concerns about the correlation between these two conditions. While studies have explored “Why does obesity cause gastroesophageal reflux disease?” and the precise mechanisms through which obesity contributes to reflux remain unclear. This article, presented by Assoc. Prof. Dr. Nguyen Anh Tuan, delves into the intricate connection between obesity and GERD.
1. What is Gastroesophageal Reflux Disease (GERD), and how common is it?
GERD is a condition characterized by frequent excessive backward flow of stomach contents into the esophagus, leading to chronic inflammation and potential complications such as acid regurgitation, heartburn, and Barrett’s esophagus. Its prevalence ranges from 10% to 20% in Western countries, while in Asia, it is reported to be below 5%.
2. How does Obesity relate to GERD?
Research has focused on the potential links between GERD and obesity, revealing that obesity is associated with an increased risk of experiencing GERD symptoms and complications such as erosive esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma compared to individuals with normal BMI. The degree of this association appears to vary based on BMI, with recent studies highlighting a heightened risk in adult women with higher BMI.

Obesity is associated with the pathological condition of gastroesophageal reflux disease
3. Why does Obesity Cause Gastroesophageal Reflux Disease
Why does obesity cause gastroesophageal reflux disease? Various mechanisms have been proposed to explain how obesity contributes to GERD. One widely accepted mechanism is the increased abdominal pressure in obese individuals, exerted consistently on the lower esophageal sphincter, leading to its relaxation and subsequent reflux. Studies monitoring pH levels over 24 hours indicate a substantial increase in reflux episodes, duration, and acidic content in obese individuals, particularly after meals.
Recent research assessing the pressure and function of the lower esophageal sphincter through high-resolution manometry reported alterations in pressure differentials influenced by obesity. Abdominal obesity, specifically, may induce hiatal hernia, affecting GERD pathophysiology by increasing reflux frequency due to increased tension, reducing lower esophageal sphincter pressure, and altering esophageal sensitivity.
4. Is Abdominal Obesity the Primary Cause of GERD in Obese Patients?
Both gastric pressure and lower esophageal sphincter pressure differentials correlate significantly with BMI and waist circumference. However, when analyzed simultaneously in a regression model, waist circumference was found to be independently associated with various pressure differentials, whereas the relationship between BMI and pressure differentials was often negligible.
Abdominal obesity, especially visceral adiposity, may lead to hiatus hernia, impacting GERD by increasing reflux frequency, reducing lower esophageal sphincter pressure, diminishing esophageal acid clearance, and enhancing sensitivity to lower esophageal sphincter relaxation.
5. The Role of the Lower Esophageal Sphincter in GERD, and How Obesity Influences It
Among the mechanisms contributing to reflux, the role of lower esophageal sphincter relaxation is paramount. Recent studies evaluating postprandial reflux in obese and overweight patients, using combined measurements of postprandial 2-hour esophageal pressures and pH monitoring, revealed a significant increase in lower esophageal sphincter relaxation rates and acid reflux rates in both obese and overweight individuals compared to those with normal BMI.
Both BMI and waist circumference exhibited a significant positive correlation with lower esophageal sphincter relaxation, with a dose-response relationship. Thus, it seems that postprandial gastric pressure in obesity leads to stronger stimulation of mechanoreceptors in the proximal stomach, resulting in prolonged relaxation of the lower esophageal sphincter after meals.

The lower esophageal sphincter plays a crucial role in GERD pathology
6. Proposed Mechanisms through Which Abdominal Obesity Induces Reflux
| Mechanical Factors | Increased pressure differentials in the stomach and stomach-esophagus junction |
| Increased risk of hiatus hernia | |
| Enhanced sensitivity to lower esophageal sphincter relaxation | |
| Reduced lower esophageal sphincter pressure | |
| Molecular and Biological Factors | Elevated levels of adipocytokines, including interleukin-6 and tumor necrosis factor-alpha |
| Impaired esophageal motility | Delayed gastric emptying and slowed esophageal clearance |
7. Visceral Obesity
In contrast to subcutaneous adiposity, visceral obesity or visceral adipose tissue (VAT) significantly differs in its metabolic activity, characterized by increased immune cell presence, higher inflammation, and greater insulin resistance. Visceral fat is associated with a higher overall mortality rate compared to subcutaneous fat.
Visceral obesity may explain certain epidemiological features of Barrett’s esophagus and esophageal adenocarcinoma. Studies have shown that the distribution of fat in the abdomen, measured by waist circumference, independently correlates with the risk of Barrett’s esophagus, with this relationship persisting even after adjusting for BMI. The findings emphasize the key role of abdominal fat in linking obesity to Barrett’s esophagus. Apart from mechanical pressure, visceral fat, with its metabolic activity, is associated with increased levels of adipocytokines in serum, including interleukin-6 and tumor necrosis factor-alpha, potentially playing a role in GERD and its sequelae, including cancer.
In fact, recent research has identified a substantial association between increased visceral fat volume and a significantly elevated risk of Barrett’s esophagus.
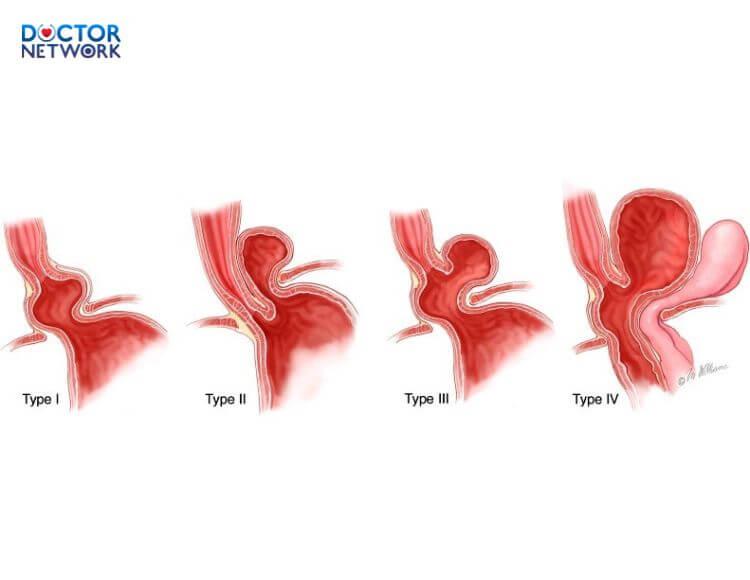
Hiatal hernia is also a complicating factor in the treatment of GERD associated with reflux esophagitis
8. Study Outcomes
Investigating the dose-response relationship and interaction between obesity and GERD, an inverse relationship between weight loss and GERD symptoms is anticipated. The prevalence of GERD symptoms in overweight and obese individuals, as well as the impact of weight loss on these symptoms, has been assessed in a recent prospective study. Weight loss strategies, including dietary changes, increased physical activity, and behavioral modifications, led to a substantial improvement in GERD symptoms, positioning weight loss as a crucial lifestyle intervention in GERD management. Moreover, weight loss within a 6-month period was associated with a remarkable reduction in GERD symptoms in 81% of patients, with complete resolution in 65%. While these findings support the recommendation of weight loss as a primary intervention for overweight and obese GERD patients, further research is needed to explore the long-term effects of weight loss on the incidence of reflux and symptom reduction before definitive conclusions can be drawn.
9. Conclusion
Obesity appears not only to be linked to the development of GERD symptoms but also contributes to GERD complications such as erosive esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma.
Although substantial evidence underscores the crucial role of increased esophagus-stomach pressure differentials and the inflammatory mediators produced by abdominal fat in the pathophysiology of GERD, the bidirectional impact of obesity and GERD remains unclear. Furthermore, weight loss seems to alleviate GERD symptoms, but ongoing studies aim to decipher the precise mechanisms by which obesity induces reflux, establishing novel treatment approaches.
This article has provided insights into “Why does obesity cause gastroesophageal reflux disease?” and related information on the intricate relationship between these two conditions. It is hoped that the article proves beneficial to the readers.
Kiểm Duyệt Nội Dung
More than 10 years of marketing communications experience in the medical and health field.
Successfully deployed marketing communication activities, content development and social networking channels for hospital partners, clinics, doctors and medical professionals across the country.
More than 6 years of experience in organizing and producing leading prestigious medical programs in Vietnam, in collaboration with Ho Chi Minh City Television (HTV). Typical programs include Nhật Ký Blouse Trắng, Bác Sĩ Nói Gì, Alo Bác Sĩ Nghe, Nhật Ký Hạnh Phúc, Vui Khỏe Cùng Con, Bác Sỹ Mẹ, v.v.
Comprehensive cooperation with hundreds of hospitals and clinics, thousands of doctors and medical experts to join hands in building a medical content and service platform on the Doctor Network application.



























